Abstract
Patients with lower-risk myelodysplastic syndromes (MDS) are affected mainly by chronic anemia and fatigue rather than progression to acute myeloid leukemia. The main aim of treatment is to improve anemia and decrease red blood cell transfusions. Erythropoiesis-stimulating agents (ESAs) are generally first-line therapy, yielding a response in about half of the patients for around 2 years. Predictive factors of response remain non-transfusion dependence and sEPO <200 IU/L. For refractory or relapsing patients after ESA, strategies include lenalidomide alone or with ESA, azacitidine, or luspatercept. For patients with del 5q, lenalidomide is more efficient.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Erythropoiesis-stimulating Agents (ESA)
- Lenalidomide
- Darbepoetin
- Erythroid Response
- International Prognostic Scoring System (IPSS)
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Pathophysiology of Anemia in MDS
Low-risk myelodysplastic syndromes (MDS) with chronic anemia are characterized by an increased susceptibility of clonal myeloid progenitors to apoptosis resulting in cytopenia despite the increased marrow cellularity. The ineffective hematopoiesis of the erythroid lineage is also due in part to a defective maturation of erythroblasts.
Very early work showed an inverse correlation between endogenous EPO levels, hemoglobin concentrations, and percentage of erythroblasts in the bone marrow with a marked variability of endogenous EPO production. It has also long been known that bone marrow cells from MDS patients show an altered response to Epo and other cytokines such as IL-3 and thrombopoietin in terms of in vitro colony formation, while stem cell factor is able to partially rescue clonogenic capacity [1, 2]. Differentiation of progenitors in liquid medium revealed abnormalities of differentiation, in particular erythroid progenitors [3, 4]. This is related to increased apoptosis of erythroid progenitors in the initial stages of MDS, especially in the terminal-stage acidophilic erythroblasts [5].
Analysis of the ex vivo expansion of progenitors in liquid medium shows that 50% of patients respond to a combination of cytokines (stem cell factor, IL-3, IL-6, and GM-CSF). The theoretical basis for treating patients with erythropoietin (EPO) at pharmacological doses is to overcome the lack of proliferation and maturation of the erythroid precursors either by stimulating the normal residual erythroid progenitors or by inducing the proliferation and differentiation of the myelodysplastic clone or even by combining the two effects [6]. There is also an abnormally low EPO level in some patients (30%) when reported for Hb [7]. Thus, there appear to be at least two mechanisms that induce a defect in cell production, a significant apoptosis and an abnormally low EPO level.
The recently uncovered genetic mutations in MDS have also been shown to be associated with specific features of the disease. For instance, TET2 knockdown leads to increased growth and delayed differentiation of erythroid progenitors, recapitulating some features of defective erythropoiesis in MDS and pointing to a role of TET2 in dyserythropoiesis [8]. ASXL1 has been shown to play a role in erythropoiesis as well, and mutations in ASXL1 may contribute to defective erythropoiesis in MDS [9].
2 Rationale for the Use of Erythropoiesis-Stimulating Agents (ESA) in MDS
Long-term transfusion therapy to treat chronic anemia in MDS is associated with several disadvantages. Over time, iron intake with transfusions may require iron-chelating treatment and may potentially lead to secondary organ damage [10]. Patients spend most of their lives with a Hb <10 g/dL, which has been associated with significant fatigue and decreased quality of life in many studies. Chronic anemia has also been shown to cause progressive deterioration of myocardial function due to the increased workload imposed on the heart (increased frequency and cardiac output) [11]. Red blood cell (RBC) transfusion in general involves rather heavy logistics with the collection of blood products, the immunohematological examinations for the donor and the recipient, the availability of a place in hospital or outpatient center, etc., which includes the cost of blood products, transportation from the patient to the hospital, and immuno-hematological examinations. The French Blood Establishment (EFS) in Franche-Comté, on the one hand, and a study by the Groupe Francophone des Myélodysplasies (GFM) showed that the average cost of transfusions for a patient with MDS was more than 800€ per month [12]. The mere fact of being dependent on transfusions implies constraints for the patients: regular visits to the outpatient center, even hospitalization, waiting between samples for investigation of irregular antibody and the transfusion. The fact of having to return regularly to a hospital structure may also increase the feeling of being “sick,” weakened, a feeling of dependence on the medical profession, and a loss of autonomy, even if the constraint of transfusions is considerably less than, for example, that of dialysis in patients with renal insufficiency. The infectious risk associated with transfusions, although now extremely reduced, is not totally zero. Accidents of hemolysis have also not completely disappeared. Finally, accidents of volume overload in these elderly subjects are also a reality.
For these reasons, there is an increasing tendency to try to correct anemia in low-risk MDS by using drugs to improve erythrocyte production or to reduce the phenomena of excessive apoptosis of erythroblastic lineage. As mentioned above, EPO can act both via inhibition of apoptosis of myelodysplastic erythroid precursors, proliferation, and maturation of the dysplastic clone as well as via selection of cytogenetically normal progenitors [13].
Evidence for the use of erythroid-stimulating agents (ESAs) such as recombinant erythropoietin alpha or beta and darbepoetin stems from meta-analyses, systematic reviews of the literature, as well as controlled clinical trials, most of them phase II. ESAs have been investigated as monotherapy as well as in combination with G-CSF. They are not currently licensed for use in MDS since they have not previously been stringently evaluated against placebo in randomized trials, but their usage is widely accepted in the field. Accordingly, their administration is recommended by the French Society of Hematology; the GFM; the German, Austrian, and Swiss Societies for Hematology/Oncology; and the German MDS Study Group, in situations where they appear effective.
Both recombinant human erythropoietin and its glycosylated longer-acting form darbepoetin have been shown to induce erythroid responses (HI-E according to IWG 2006 criteria) in anemic low-risk MDS patients in 30–70% of cases.
Data from the EUMDS registry, a prospective longitudinal registry of newly diagnosed lower-risk MDS patients, has shown that appropriate use of ESA can significantly delay onset of transfusion dependency in lower-risk non-transfused MDS patients [14]. ESA treatment was associated with a nonsignificant survival benefit, which was greater in patients without prior transfusions. Responding patients also had a better prognosis in terms of a lower risk of death although the risk of transformation to acute leukemia was not affected.
In a phase 2 single-arm trial evaluating darbepoetin alpha [15] at a dose of 500 ug/3 weeks, the response rate (major erythroid response) in ESA naïve patients was 49% at 13 weeks, with 82% of patients achieving the target hemoglobin of 11 g/dL. The response rate in prior ESA-treated patients was 26% at 13 weeks, with 55% achieving target hemoglobin level. A systematic review and meta-analysis of ten trials also revealed an advantageous response for ESA naïve as well as ESA-pretreated MDS patients with darbepoetin, with a response rate of 38–72% and a median response duration of 12 to 51+ months [16]. Transfusion rates and hemoglobin levels improved with treatment. This meta-analysis suggests that darbepoetin treatment can be useful for improving erythroid response in MDS patients with anemia, even among patients previously treated with ESA.
Preliminary results of two large multicenter randomized double-blind placebo-controlled clinical trials evaluating either EPO or darbepoetin against placebo in lower-risk MDS (ARCADE and EPOANE studies, NCT01362140 and NCT01381809) have been finshed and published [17] which led to licensing of EPO alfa in the indication of low risk MDS with anemia. In the EPOANE trial, HI-E erythroid response (IWG 2006) with EPO alfa was achieved in 31.8% of patients receiving EPO alfa vs 4.4% of patients receiving placebo, with a reduction of transfusion dependence from 54% to 24.7% at week 16 to week 24. The ARCADE study showed only 14.7% HI-E with darbepoetin vs 0% for placebo, but transfusion dependence was reduced from 59.2% to 36.1% with darbepoetin.
Of note, ESAs do not appear to have a role in the evolutionary course of the disease, i.e., they do not alter the risk of developing acute myeloid leukemia (AML) in one direction or another. In addition, two recent studies (one from the GFM and one from the Italian and the Swedish) showed that ESAs appear to provide a survival advantage in low-risk MDS, at least in responders [18]. Indeed, in the GFM series compared historically with that used to create the International Prognostic Scoring System (IPSS) score, it was shown that the 5-year survival of ESA-treated MDS was 64%, whereas it was only 39% in the historical series matched on the main prognostic factors such as age, the Franco-American-British classification (FAB), the percentage of blasts, and the karyotype [19]. These survival benefit data appear to be confirmed in the randomized study of ESA versus supportive treatments by Greenberg et al. [20].
3 Timing of Treatment Initiation and Dosing
In general, it is necessary to initiate ESA treatment before the patient becomes transfusion dependent. Patients who have not received prior transfusions respond better than patients already transfused. In the GFM series [19], 66% of non-transfused patients responded to ESA (IWG [International Working Group] 2006) versus only 37% of transfused patients. A retrospective study of the GFM also showed that in the non-transfused patients, the sooner ESA was introduced after diagnosis, notably before 6 months, the more patients responded and the longer was the delay of the onset of RBC transfusions. The response rate was 76% versus 46% when patients received ESAs less than 6 months after diagnosis versus more than 6 months [21, 22]. However, these results need to be confirmed prospectively.
Many ESA trials at doses of 30,000–60,000 U/week Epo (or 150–300 μg/week darbepoetin) showed that 20–60% of patients had a significant erythroid response, with lengthening of transfusion intervals or even disappearance of transfusion need. The rate of response depends on prognostic factors and is discussed below. The vast majority of the responses are observed in the first 12 weeks, although they may sometimes occur later [23]. The median response time is 2 years [18,18,20]. Weekly administration of recombinant ESA shows response rates similar to EPO response rates alone administered once/day or 2–3 times/week [24]. The reduction in the number of injections is an important factor in improving the quality of life of these patients.
Several phase II studies have been reported with darbepoetin [25, 26]. In addition to its prolonged activity, the additional glycosylation of darbepoetin increases its stability. Its lifetime is three times longer than traditional ESA, thanks to the two additional carbohydrate chains attached to the protein skeleton by nitrogenous residues. Increased bioavailability allows a reduction in the required frequency of injections of once/week during the induction phase to once every 2 weeks or more during the maintenance phase. Weekly administration of darbepoetin alfa at a dose of 150 μg/week results in response rates varying between 40 and 60%.
A French study was carried out on 62 patients with low-grade MDS, with an EPO level below 500 IU/L and a low or intermediate IPSS score 1. Darbepoetin was administered at a dose of 300 μg once/week for 12 weeks. The response rate was 71% [25]. Another darbepoetin regimen at 500 μg/2 weeks showed a response rate of 56% at 24 weeks [26]. In the Gabrilove et al. study, a 500 μg dose schedule every 3 weeks yielded a 49% major response according to IWG 2000, with 82% of patients reaching the target 11 g/dL Hb [15].
EPO has also been evaluated in several randomized trials with and without addition of either G-CSF or GM-CSF. An analysis of combined data from three phase II Nordic trials (n = 121) on the long-term outcomes with Epo plus G-CSF (given for 12–18 weeks and followed by maintenance in responders) in patients with MDS reported a hematologic response rate of 39% with a median duration of response of 23 months. Long-term outcomes were compared with outcomes from untreated patients (n = 237) as controls. Based on multivariate Cox regression analysis, treatment with Epo plus G-CSF was associated with a significantly improved survival outcome (hazard ratio [HR], 0.61; 95% CI, 0.44–0.83; P = 0.002). An exploratory analysis revealed that the association between treatment and survival was significant only for the IPSS low-risk group and was further restricted to patients requiring fewer than two units of RBC transfusions per month. No significant association was found between the treatment and frequency of AML progression [18].
It remains debatable whether addition of G-CSF/GM-CSF can actually improve response rates achieved with ESA alone. A meta-analysis specifically examining erythroid response to EPO alone compared to EPO + G-CSF or GM-CSF failed to show a clear advantage for either treatment arm with comparable response rates [27] (Table 6.1).
4 Predictive Factors of Response
Predictive models have consistently shown that response rates are higher in low-risk MDS patients with no or low transfusion need and low endogenous Epo levels, ranging between 500 and 100 IU/L in published analyses [18, 19, 28]. These two variables allowed to establish a score that distinguished three groups of patients with a probability of Epo + G-CSF response of 74, 23, and 7%, depending on whether 0, 1, or 2 of these risk factors were present. In addition, an interval between diagnosis and ESA onset <6 months also predicted for response [21, 22].
The other favorable prognostic factors of response are a rate of medullary blasts of less than 5% and an IPSS of less than or equal to 1 [19] and, in a series, the absence of multilineage dysplasia [29]. However, in a larger series of patients, we did not find the latter factor [19]. In our experience, 56% of MDS-EB-1 responded, and this category can therefore also benefit from ESA [19]. MDS with excess of ring sideroblasts had a response rate of 59%, lower than RA or RCMD, but not negligible, and it is still indicated to test ESA in this subgroup of patients with a median duration of response of 18 months [19]. Low-risk MDS with deletion of the long arm of chromosome 5 (del 5q) respond less frequently than other low-risk MDS and have shorter response times [30]. Recently, we showed that the revised version of IPSS, IPSS-R, and ferritin (>350 ng/mL) in addition to the endogenous EPO level of <200 IU/L made it possible to distinguish five groups with response rates ranging from 85 to 20% [31]. In 1/3 of patients with a response rate of about 30%, alternative treatments are likely to be available.
Other more sophisticated biological tools can predict response to ESA, such as flow cytometry that quantifies multilineage dysplasia and the percentage of blasts or which evaluates the degree of ERK or STAT5 phosphorylation in the targeted erythroblast population [32, 33].
Molecular screening for gene mutations most frequently found in MDS by targeted sequencing does not contribute more than the traditional clinical-biological factors to response prediction. The presence of >2 somatic mutations was associated with lower HI-E in ESA-treated MDS patients. However, individual mutations (e.g., SF3B1, TET2, ASXL1, DNMT3A), mutations in particular gene categories, and mutational patterns had no significant impact on response. In fact, in multivariate analysis, prognostic factors of HI-E were serum EPO level, RBC TD, and IPSS-R, while number or type of mutation was not. Although patients with more than three mutations had a lower ESA response rate (46 vs 74%), this impact disappeared in multivariate analysis with IPSS-R, while the presence of >2 mutations was confirmed to be predictive of shorter survival. Thus, although future analysis of somatic mutations in larger patient cohorts may lead to different conclusions, conventional parameters, especially RBC-TD, sEPO level, and IPSS-R currently appear sufficient to predict response to ESA treatment in routine practice [34].
Of note, the lower response rate to ESA in the two large prospective placebo-controlled randomized trials compared to previously reported rates of >50% has questioned the suitability of the current IWG 2006 criteria to evaluate erythroid response to ESA. Adapted response criteria than those currently used in IWG 2006 may be needed to adequately evaluate benefit of ESA in lower-risk MDS (Table 6.2).
5 Benefits of ESA in MDS: OS, Quality of Life, and Safety
Quality of life (QoL) assessment tools measure symptoms such as fatigue, dyspnea, sleep disorders, and physical, emotional, social, cognitive, and spiritual aspects of the patient’s function. In general, the QoL of MDS patients has been shown to be significantly reduced compared to age-matched controls [42, 43] , mainly due to symptoms of anemia such as fatigue. However, published studies have not been able to clearly show a positive impact of regular transfusions on QOL in MDS patients with chronic anemia [44].
The impact of ESA treatment on quality of life (QoL) has also been measured in some studies, although most of these were quite small in terms of patient numbers and the results of the two large placebo controlled clinical trials evaluating either Epo or darbepoetin have yet to be published. The systematic review and meta-analysis of darbepoetin efficacy in a total of 647 patients have demonstrated an increased quality of life with darbepoetin treatment [16]. Increased QoL was correlated with increased hemoglobin levels in four of the six original studies that reported QoL [15, 26, 45, 46].
In general, quality of life scores correlate well with Hb and its increase by ESA, and stable Hb levels are preferable to transfusion-related fluctuations [12, 41, 47]. However, it is more difficult to demonstrate the superiority of ESAs compared to transfusions in terms of QoL because transfused patients are by definition non-responders and have lower Hb levels. Most studies have shown that ESAs improve the quality of life of patients, at least responders.
In a prospective trial examining 53 patients with low-risk MDS and anemia treated with Epo, patients achieving either CR or PR showed clinically significant improvement in global QOL, social functioning, fatigue, and dyspnea. The improvement was statistically significant only for global QOL (P = 0.01), with a borderline significance for fatigue (P < 0.05) [48].
To complement patient-reported quality of life data, the GFM undertook, in a phase II trial, measurement of exercise capacity under darbepoetin alfa and G-CSF using VO2max (maximum capacity oxygen consumption) and the 6-min walking test (distance traveled within 6-min walk) [49, 50]. The study found significant improvement in the treatment of darbepoetin +/− G-CSF of quality of life scores and VO2max in responders compared to non-responders. These findings are important because they demonstrate for the first time in the context of MDS that the correction of anemia has an objective and measurable interest in the physical functioning of patients.
In terms of safety, a total of 127 AEs were reported across 647 patients in ten studies, including 37 deaths (5.7%). Progression to AML was reported in eight cases (1.2%), and disease progression was reported in three cases (0.5%). The most common AEs were neoplasm (3.2%), hypertension (3.2%), and stroke (1.4%). As these reported AEs were from single-arm trials, it is not possible to adequately assess if incidence of AEs was higher than in untreated patients. ESAs are generally well tolerated, with weekly monitoring of the hemogram during the first weeks of treatment, to avoid a possible risk of excessive response (with polycythemia), and then adjusting the dose so as not to exceed Hb levels of 12 g/dL. In MDS, there have been no reports of ESA secondary thromboembolic events in the published series of 403 GFM patients [16, 19]. It is therefore not necessary to initiate antithrombotic therapy, unless in the presence of thrombophilia. Gabrilove reported an incidence of 2% of thromboembolic accidents, without pulmonary embolism [15]. In the case of combination with lenalidomide, recommendations for the prevention of thromboembolic disease are required [51]. Anti-Epo antibodies after treatment with Epo, resulting in erythroblastopenia, have been described mainly in the dialysis population and were due to the immunogenicity of the syringe seal of some Epo formulations, but are exceptionally rare [52].
In summary, administration of Epo or darbepoetin is safe and shows best efficacy in low-risk MDS patients with low or no transfusion dependence and low endogenous Epo levels, highlighting the rationale for timely initiation of ESA treatment in this patient group.
6 Alternatives After ESA Failure
A loss of response to ESA involves checking, by a myelogram and a karyotype, the absence of progression of the disease toward a more advanced stage (increase in medullary blast counts, appearance of new cytogenetic anomalies), found in fact only in about 30% of the cases in our experience. In other patients, an additional cause of anemia (including iron deficiency or folate deficiency) should be investigated and treated.
A variable proportion of patients treated with ESA will be resistant from the start (primary refractory), or they will become secondary resistant (relapsed) after an initial response time close to the median of the response time equal to 2 years, observed in all the responders. Patients who do not respond after 8–12 weeks of ESA +/− G-CSF are defined as primary refractory or resistant. In the GFM series, proportions of patients with ESA failure (refractory and relapsed) were about 50 and 26% with a median follow-up of 7 years. Using a 6-month cut-off for the relapse period, we identified a population with a poorer overall survival with a 36-month median survival after ESA failure vs 54 months (p = 0.02) and a cumulative incidence of AML transformation of 21.6 vs 9% at 5 years [49, 50].
In a larger multinational cohort of 1147 patients with ESA failure, the 5-year cumulative incidence of AML of patients in primary or secondary failure was 13.4%, including 8.1% for secondary failure vs 16.7% for primary failure patients suggesting that patients with primary failure to ESA have the worst prognosis, independently of IPSS-R [53].
Addition of G-CSF to EPO in the event of EPO failure alone results in a response in 20–35% of cases, but it appears to be less when the failure is observed at high doses of Epo (in practice, 60,000 U/week or darbepoetin 300 μg/week) compared to the lowest doses. The most recent data are from Greenberg, where the addition of G-CSF to EPO 150 IU/kg/day (approximately 70,000 IU/week) increased the erythroid response according to IWG 2006 only from 34 to 42% [20]. In addition, two meta-analyses suggest that ESA doses of 60,000–80,000 IU/week would be at least as effective as the addition of G-CSF to EPO at doses of 30,000–40,000 IU/week with response rates of 64% and 50%, respectively [27, 54].
Recently, a trial of GFM showed that the addition of ATRA (all-trans-retinoic acid) to recombinant EPO at a dose of 45 mg/m2/day for 1 week out of two could “catch up” to 1/3 of Epo’s failures alone, even patients with very frequent transfusions, but less patients with high endogenous EPO levels (>500 UI/l) [55]. In the same perspective, stimulation of erythroid differentiation by the association of EPO with retinoic acid, an Italian study proposed the use of 13-retinoic acid (Roaccutane 20 mg/day) and vitamin D3 (1 μg/day) in anemic patients with a low-risk MDS in the first line but with pejorative factors such as the high endogenous EPO level and a high number of RBC transfusions before treatment, with an erythroid response of 60% [56].
Neo-angiogenesis is often observed in myelodysplasia, and studies have also demonstrated an increase of plasma VEGF in patients with myelodysplasia with excess blasts [57, 58]. The anti-angiogenic action of the molecules of the class of immunomodulators (IMID) (thalidomide and lenalidomide) should be noted, although the importance of this mechanism in their therapeutic action is not known. In any case, a GFM study with low-dose thalidomide provides a response in about 30% of patients who are refractory to EPO but at the cost of side effects and non-negligible asthenia [59, 60].
Lenalidomide acts on VEGF and increases the expression of gamma globin and overall erythroid differentiation in addition to its more specific action in del 5q-. The MDS002 trial showed that in patients with transfusion dependence (n = 214), with non-del 5q low-risk MDS, LEN 10 mg/day or 21/28 days yielded a HI-E response of 43% [61]. Lenalidomide has been used in non-del5q lower-risk MDS patients ineligible for or refractory to ESAs, and its efficacy at 10 mg/day versus placebo was recently evaluated in transfusion-dependent lower-risk MDS patients [62]. Transfusion independence was obtained in 26.9% of the cases. A subgroup of patients with endogenous EPO levels <100 U/L who had received previous ESA treatment reached transfusion independence in 42.5% of the cases. These two simple variables, that is, previous therapies and low endogenous EPO, could be used to select patients more prone to benefit from lenalidomide after ESA failure, while investigations on molecular characteristics to better identify responsive subjects are ongoing. At present, no somatic mutation predicts for response to lenalidomide. Quite interestingly, the combination of lenalidomide and ESAs has also been recently shown to have additive effects in restoring erythropoiesis when ESAs fail [21, 22, 51]. Consistent with results obtained with single-drug lenalidomide, patients with EPO levels <100 U/L experienced higher erythroid responses; CRBNrs1672753 polymorphism was also predictive of erythroid improvement. The hematological toxicity is not negligible with 62% neutropenia and 36% grade 3–4 thrombocytopenia [51].
There could also be a rationale to associate lenalidomide and EPO even after EPO failure. LEN induces coalescence of the lipid rafts in the erythroid progenitors, leading to a concentration of EPO receptors on the surface of these cells and better transduction of the EPO-induced signal with phosphorylation of JAK2 and downstream STAT5 [63]. An open, monocentric, two-step trial with a 10 mg lenalidomide regimen followed by 15 mg with 40000 IU of EPO at week 16 in 39 refractory patients resulted in 25% HI-E; 21% of patients were overall rescued with LEN + EPO (in non-5q patients) [62].
In the GFM, a phase III randomized trial proposed LEN alone, 10 mg/day, 21 days/4 weeks, or LEN + EPO beta, 60,000 U/week in low-risk MDS del 5q, not dependent on transfusions and after EPO failure. The response to four cycles was 23.1% in the lenalidomide arm alone vs 39.4% in the LEN + EPO arm (p = 0.04), calling for the addition of EPO to LEN patients refractory to EPO alone. The median response was 15–18 months. Side effects are moderate, but a dose reduction to 5 mg/day was necessary in approximately 40% of patients. The benefit of LEN was reserved for patients with favorable cytogenetics. Patients with a low level of expression of NPM1 and a cereblon type A/A polymorphism are less likely to respond to the LEN + EPO combination [51].
As for the use of demethylating agents, there is an erythroid response of the order of 40% in CALGB trials, low-risk MDSs, and transfusion independence in 70% of transfusion-dependent RAs [64]. In an MD Anderson study with an oral form of azacitidine, there was a 36–40% overall response in MD Anderson and GESMD low-risk SMDs with pejorative factors, including thrombocytopenia [65]. The GFM assay randomizes 5-azacytidine 5 days vs 5-azacytidine + EPO at 60,000 IU/week. Although there is a small imbalance of arms with more RARS in the solely AZA arm, the overall response rates are similar around 16–18% by IWG 2006, with significant toxicity, especially related to fever and infections leading to hospitalization in about 40% of cases [66].
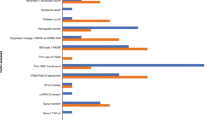
A pathway of the future has been opened with the “trap ligands” of activin II exerting an antagonistic effect on its receptor. Indeed erythroid differentiation is mainly regulated by the EPO in the early phases and inhibited by molecules of the family of TGF-beta, as GDF11 and activin A. Two types of “ligands trap” were synthesized: the sotatercept (ACE-011), initially intended to treat osteoporosis in postmenopausal women, and luspatercept (ACE-536). These two molecules are administered subcutaneously every 3 weeks. Dose escalation trials show encouraging results with an erythroid response rate of 40% at 24 weeks for sotatercept and 40% at 8 weeks for luspatercept with interesting results in the subgroup of sideroblastic anemia [67, 68]. A randomized trial of luspatercept vs placebo is ongoing for transfusion-dependent RARS patients who have lost response or have a low probability of response to ESAs (irrespective of SF3B1 mutation) (ClinicalTrials.gov Identifier: NCT02631070) (Fig. 6.1).
In conclusion, there is increasing interest in the population of patients who are refractory to EPO or who no longer respond to EPO. Although they have a poorer prognosis, complementary adverse prognostic factors would make it possible to delineate a group of patients in whom azacitidine could prove beneficial. Among the currently available drugs, the LEN combination (low dose 5 mg/day) + EPO is an interesting option to offer to patients with ESA failure. The addition of ATRA is to be considered in these cases. Other routes than EPO are currently being investigated such as the “trap ligands” of activin A. And finally allogeneic transplantation could be proposed for a subset of these patients refractory to EPO.
References
Backx B, Broeders L, Lowenberg B. Kit ligand improves in vitro erythropoiesis in myelodysplastic syndrome. Blood. 1992;80(5):1213–7.
Merchav S, Nielsen OJ, Rosenbaum H, Sharon R, Brenner B, Tatarsky I, Scigalla P, Wieczorek L. In vitro studies of erythropoietin-dependent regulation of erythropoiesis in myelodysplastic syndromes. Leukemia. 1990;4(11):771–4.
Asano H, Hotta T, Ichihara M, Murate T, Kobayashi M, Saito H. Growth analysis of marrow CD34-positive hematopoietic progenitor cells in patients with myelodysplastic syndromes. Leukemia. 1994;8(5):833–8.
Sawada K, Sato N, Notoya A, Tarumi T, Hirayama S, Takano H, Koizumi K, Yasukouchi T, Yamaguchi M, Koike T. Proliferation and differentiation of myelodysplastic CD34+ cells: phenotypic subpopulations of marrow CD34+ cells. Blood. 1995;85(1):194–202.
Parker JE, Fishlock KL, Mijovic A, Czepulkowski B, Pagliuca A, Mufti GJ. Low-risk myelodysplastic syndrome is associated with excessive apoptosis and an increased ratio of pro- versus anti-apoptotic bcl-2-related proteins. Br J Haematol. 1998;103(4):1075–82.
Stein RS. The role of erythropoietin in the anemia of myelodysplastic syndrome. Clin Lymphoma. 2003;4(Suppl 1):S36–40.
Bowen DT, Jacobs A, Cotes PM, Lewis TC. Serum erythropoietin and erythropoiesis in patients with myelodysplastic syndromes. Eur J Haematol. 1990;44(1):30–2.
Zhao Z, Chen S, Zhu X, Pan F, Li R, Zhou Y, Yuan W, Ni H, Yang FC, Xu M. The catalytic activity of TET2 is essential for its myeloid malignancy-suppressive function in hematopoietic stem/progenitor cells. Leukemia. 2016;30(8):1784–8.
Shi H, Yamamoto S, Sheng M, Bai J, Zhang P, Chen R, Chen S, Shi L, Abdel-Wahab O, Xu M, Zhou Y, Yang FC. ASXL1 plays an important role in erythropoiesis. Sci Rep. 2016;6:28789.
Shander A, Cappellini MD, Goodnough LT. Iron overload and toxicity: the hidden risk of multiple blood transfusions. Vox Sang. 2009;97(3):185–97.
Anand I, McMurray JJ, Whitmore J, Warren M, Pham A, McCamish MA, Burton PB. Anemia and its relationship to clinical outcome in heart failure. Circulation. 2004;110(2):149–54.
Casadevall N, Durieux P, Dubois S, Hemery F, Lepage E, Quarre MC, Damaj G, Giraudier S, Guerci A, Laurent G, Dombret H, Chomienne C, Ribrag V, Stamatoullas A, Marie JP, Vekhoff A, Maloisel F, Navarro R, Dreyfus F, Fenaux P. Health, economic, and quality-of-life effects of erythropoietin and granulocyte colony-stimulating factor for the treatment of myelodysplastic syndromes: a randomized, controlled trial. Blood. 2004;104(2):321–7.
Tehranchi R, Invernizzi R, Grandien A, Zhivotovsky B, Fadeel B, Forsblom AM, Travaglino E, Samuelsson J, Hast R, Nilsson L, Cazzola M, Wibom R, Hellstrom-Lindberg E. Aberrant mitochondrial iron distribution and maturation arrest characterize early erythroid precursors in low-risk myelodysplastic syndromes. Blood. 2005;106(1):247–53.
Garelius HK, Johnston WT, Smith AG, Park S, de Swart L, Fenaux P, Symeonidis A, Sanz G, Cermak J, Stauder R, Malcovati L, Mittelman M, van de Loosdrecht AA, van Marrewijk CJ, Bowen D, Crouch S, de Witte TJ, Hellstrom-Lindberg E. Erythropoiesis-stimulating agents significantly delay the onset of a regular transfusion need in nontransfused patients with lower-risk myelodysplastic syndrome. J Intern Med. 2017;281(3):284–99.
Gabrilove J, Paquette R, Lyons RM, Mushtaq C, Sekeres MA, Tomita D, Dreiling L. Phase 2, single-arm trial to evaluate the effectiveness of darbepoetin alfa for correcting anaemia in patients with myelodysplastic syndromes. Br J Haematol. 2008;142(3):379–93.
Park S, Fenaux P, Greenberg P, Mehta B, Callaghan F, Kim C, Tomita D, Xu H. Efficacy and safety of darbepoetin alpha in patients with myelodysplastic syndromes: a systematic review and meta-analysis. Br J Haematol. 2016;174(5):730–47.
Platzbecker U, Symeonidis A, Oliva EN, Goede JS, Delforge M, Mayer J, Slama B, Badre S, Gasal E, Mehta B, Franklin J. A phase 3 randomized placebo-controlled trial of darbepoetin alfa in patients with anemia and lower-risk myelodysplastic syndromes. Leukemia. 2017;31(9):1944–50. https://doi.org/10.1038/leu.2017.192. Epub 2017 Jun 19.
Jadersten M, Malcovati L, Dybedal I, Della Porta MG, Invernizzi R, Montgomery SM, Pascutto C, Porwit A, Cazzola M, Hellstrom-Lindberg E. Erythropoietin and granulocyte-colony stimulating factor treatment associated with improved survival in myelodysplastic syndrome. J Clin Oncol. 2008;26(21):3607–13.
Park S, Grabar S, Kelaidi C, Beyne-Rauzy O, Picard F, Bardet V, Coiteux V, Leroux G, Lepelley P, Daniel MT, Cheze S, Mahe B, Ferrant A, Ravoet C, Escoffre-Barbe M, Ades L, Vey N, Aljassem L, Stamatoullas A, Mannone L, Dombret H, Bourgeois K, Greenberg P, Fenaux P, Dreyfus F. Predictive factors of response and survival in myelodysplastic syndrome treated with erythropoietin and G-CSF: the GFM experience. Blood. 2008;111(2):574–82.
Greenberg PL, Sun Z, Miller KB, Bennett JM, Tallman MS, Dewald G, Paietta E, van der Jagt R, Houston J, Thomas ML, Cella D, Rowe JM. Treatment of myelodysplastic syndrome patients with erythropoietin with or without granulocyte colony-stimulating factor: results of a prospective randomized phase 3 trial by the Eastern Cooperative Oncology Group (E1996). Blood. 2009;114(12):2393–400.
Park S, Kelaidi C, Sapena R, Vassilieff D, Beyne-Rauzy O, Coiteux V, Vey N, Ravoet C, Cheze S, Rose C, Legros L, Stamatoullas A, Escoffre-Barbe M, Guerci A, Chaury MP, Fenaux P, Dreyfus F. Early introduction of ESA in low risk MDS patients may delay the need for RBC transfusion: a retrospective analysis on 112 patients. Leuk Res. 2010a;34(11):1430–6.
Park S, Vassilieff D, Bardet V, Viguie F, Dreyfus F. Efficacy of the association of lenalidomide to erythropoiesis-stimulating agents in del (5q) MDS patients refractory to single-agent lenalidomide. Leukemia. 2010b;24(11):1960–2.
Terpos E, Mougiou A, Kouraklis A, Chatzivassili A, Michalis E, Giannakoulas N, Manioudaki E, Lazaridou A, Bakaloudi V, Protopappa M, Liapi D, Grouzi E, Parharidou A, Symeonidis A, Kokkini G, Laoutaris NP, Vaipoulos G, Anagnostopoulos NI, Christakis JI, Meletis J, Bourantas KL, Zoumbos NC, Yataganas X, Viniou NA. Prolonged administration of erythropoietin increases erythroid response rate in myelodysplastic syndromes: a phase II trial in 281 patients. Br J Haematol. 2002;118(1):174–80.
Musto P, Falcone A, Sanpaolo G, Bodenizza C, La Sala A, Perla G, Carella AM. Efficacy of a single, weekly dose of recombinant erythropoietin in myelodysplastic syndromes. Br J Haematol. 2003;122(2):269–71.
Mannone L, Gardin C, Quarre MC, Bernard JF, Vassilieff D, Ades L, Park S, Vaultier S, Hamza F, Beyne-rauzy MO, Cheze S, Giraudier S, Agape P, Legros L, Voillat L, Dreyfus F, Fenaux P. High-dose darbepoetin alpha in the treatment of anaemia of lower risk myelodysplastic syndrome results of a phase II study. Br J Haematol. 2006;133(5):513–9.
Stasi R, Abruzzese E, Lanzetta G, Terzoli E, Amadori S. Darbepoetin alfa for the treatment of anemic patients with low- and intermediate-1-risk myelodysplastic syndromes. Ann Oncol. 2005;16(12):1921–7.
Mundle S, Lefebvre P, Vekeman F, Duh MS, Rastogi R, Moyo V. An assessment of erythroid response to epoetin alpha as a single agent versus in combination with granulocyte- or granulocyte-macrophage-colony-stimulating factor in myelodysplastic syndromes using a meta-analysis approach. Cancer. 2009;115(4):706–15.
Hellstrom-Lindberg E, Robert KH, Gahrton G, Lindberg G, Forsblom AM, Kock Y, Ost A. A predictive model for the clinical response to low dose ara-C: a study of 102 patients with myelodysplastic syndromes or acute leukaemia. Br J Haematol. 1992;81(4):503–11.
Howe RB, Porwit-MacDonald A, Wanat R, Tehranchi R, Hellstrom-Lindberg E. The WHO classification of MDS does make a difference. Blood. 2004;103(9):3265–70.
Kelaidi C, Park S, Brechignac S, Mannone L, Vey N, Dombret H, Aljassem L, Stamatoullas A, Ades L, Giraudier S, de Botton S, Raynaud S, Lepelley P, Picard F, Leroux G, Daniel MT, Bouscary D, Dreyfus F, Fenaux P. Treatment of myelodysplastic syndromes with 5q deletion before the lenalidomide era; the GFM experience with EPO and thalidomide. Leuk Res. 2008;32(7):1049–53.
Santini V, Schemenau J, Levis A, Balleari E, Sapena R, Ades L, Guerci A, Beyne-Rauzy O, Gourin MP, Cheze S, Stamatoullas A, Sanna A, Gioia D, Cametti G, Ferrero D, Raffoux E, Rose C, Poloni A, Prebet T, Legros L, Natarajan-Ame S, Fenaux P, Germing U, Dreyfus F, Park S. Can the revised IPSS predict response to erythropoietic-stimulating agents in patients with classical IPSS low or intermediate-1 MDS? Blood. 2013;122(13):2286–8.
Frisan E, Pawlikowska P, Pierre-Eugene C, Viallon V, Gibault L, Park S, Mayeux P, Dreyfus F, Porteu F, Fontenay M. p-ERK1/2 is a predictive factor of response to erythropoiesis-stimulating agents in low/int-1 myelodysplastic syndromes. Haematologica. 2010;95(11):1964–8.
Spinelli E, Caporale R, Buchi F, Masala E, Gozzini A, Sanna A, Sassolini F, Valencia A, Bosi A, Santini V. Distinct signal transduction abnormalities and erythropoietin response in bone marrow hematopoietic cell subpopulations of myelodysplastic syndrome patients. Clin Cancer Res. 2012;18(11):3079–89.
Kosmider O, Passet M, Santini V, Platzbecker U, Andrieu V, Zini G, Beyne-Rauzy O, Guerci A, Masala E, Balleari E, Bulycheva E, Dreyfus F, Fenaux P, Fontenay M, Park S, Gfm F, M. D. S. D. Are somatic mutations predictive of response to erythropoiesis stimulating agents in lower risk myelodysplastic syndromes? Haematologica. 2016;101(7):e280–3.
Hellström-Lindberg E. Efficacy of erythropoietin in the myelodysplastic syndromes: a meta-analysis of 205 patients from 17 studies. Br J Haematol. 1995;89(1):67–71.
Italian Cooperative Study Group for rHuEpo in Myelodysplastic Syndromes, Ferrini PR, Grossi A, Vannucchi AM, Barosi G, Guarnone R, Piva N, Musto P, Balleari E. A randomized double-blind placebo-controlled study with subcutaneous recombinant human erythropoietin in patients with low-risk myelodysplastic syndromes. Br J Haematol. 1998;103(4):1070–4.
Stasi R, Brunetti M, Bussa S, Conforti M, Di Giulio C, Crescenzi A, Terzoli E, Vecchione A, Pagano A. Response to recombinant human erythropoietin in patients with myelodysplastic syndromes. Clin Cancer Res. 1997;3(5):733–9.
Stasi R, Brunetti M, Terzoli E, Abruzzese E, Amadori S. Once-weekly dosing of recombinant human erythropoietin alpha in patients with myelodysplastic syndromes unresponsive to conventional dosing. Ann Oncol. 2004;15(11):1684–90.
Mantovani L, Lentini G, Hentschel B, Wickramanayake PD, Loeffler M, Diehl V, Tesch H. Treatment of anaemia in myelodysplastic syndromes with prolonged administration of recombinant human granulocyte colony-stimulating factor and erythropoietin. Br J Haematol. 2000;109(2):367–75.
Clavio M, Nobili F, Balleari E, Girtler N, Ballerini F, Vitali P, Rosati P, Venturino C, Varaldo R, Gobbi M, Ghio R, Rodriguez G. Quality of life and brain function following high-dose recombinant human erythropoietin in low-risk myelodysplastic syndromes: a preliminary report. Eur J Haematol. 2004;72(2):113–20.
Spiriti MA, Latagliata R, Niscola P, Cortelezzi A, Francesconi M, Ferrari D, Volpe E, Clavio M, Grossi A, Reyes MT, Musto P, Mitra ME, Azzara A, Pagnini D, D’Arena G, Spadano A, Balleari E, Pecorari P, Capochiani E, De Biasi E, Perego D, Monarca B, Pisani F, Scaramella G, Petti MC. Impact of a new dosing regimen of epoetin alfa on quality of life and anemia in patients with low-risk myelodysplastic syndrome. Ann Hematol. 2005;84(3):167–76.
Hellstrom-Lindberg E. Approach to anemia associated with myelodysplastic syndromes. Curr Hematol Rep. 2003;2(2):122–9.
Jansen AJ, Essink-Bot ML, Beckers EA, Hop WC, Schipperus MR, Van Rhenen DJ. Quality of life measurement in patients with transfusion-dependent myelodysplastic syndromes. Br J Haematol. 2003;121(2):270–4.
Platzbecker U, Hofbauer LC, Ehninger G, Holig K. The clinical, quality of life, and economic consequences of chronic anemia and transfusion support in patients with myelodysplastic syndromes. Leuk Res. 2012;36(5):525–36.
Oliva EN, Nobile F, Alimena G, Specchia G, Danova M, Rovati B, Ronco F, Impera S, Risitano A, Alati C, Breccia M, Carmosino I, Vincelli I, Latagliata R. Darbepoetin alfa for the treatment of anemia associated with myelodysplastic syndromes: efficacy and quality of life. Leuk Lymphoma. 2010;51(6):1007–14.
Villegas A, Arrizabalaga B, Fernandez-Lago C, Castro M, Mayans JR, Gonzalez-Porras JR, Duarte RF, Remacha AF, Luno E, Gasquet JA. Darbepoetin alfa for anemia in patients with low or intermediate-1 risk myelodysplastic syndromes and positive predictive factors of response. Curr Med Res Opin. 2011;27(5):951–60.
Oliva EN, Finelli C, Santini V, Poloni A, Liso V, Cilloni D, Impera S, Terenzi A, Levis A, Cortelezzi A, Ghio R, Musto P, Semenzato G, Clissa C, Lunghi T, Trappolini S, Gaidano V, Salvi F, Reda G, Villani O, Binotto G, Cufari P, Cavalieri E, Spiriti MA. Quality of life and physicians’ perception in myelodysplastic syndromes. Am J Blood Res. 2012;2(2):136–47.
Hellstrom-Lindberg E, Gulbrandsen N, Lindberg G, Ahlgren T, Dahl IM, Dybedal I, Grimfors G, Hesse-Sundin E, Hjorth M, Kanter-Lewensohn L, Linder O, Luthman M, Lofvenberg E, Oberg G, Porwit A, MacDonald AR, Samuelsson J, Tangen JM, Winquist I, Wisloff F. A validated decision model for treating the anaemia of myelodysplastic syndromes with erythropoietin + granulocyte colony-stimulating factor: significant effects on quality of life. Br J Haematol. 2003;120(6):1037–46.
Kelaidi C, Beyne-Rauzy O, Braun T, Sapena R, Cougoul P, Ades L, Pillard F, Lamberto C, Charniot JC, Guerci A, Choufi B, Stamatoullas A, Slama B, De Renzis B, Ame S, Damaj G, Boyer F, Chaury MP, Legros L, Cheze S, Testu A, Gyan E, Bene MC, Rose C, Dreyfus F, Fenaux P. High response rate and improved exercise capacity and quality of life with a new regimen of darbepoetin alfa with or without filgrastim in lower-risk myelodysplastic syndromes: a phase II study by the GFM. Ann Hematol. 2013a;92(5):621–31.
Kelaidi C, Park S, Sapena R, Beyne-Rauzy O, Coiteux V, Vey N, Stamatoullas A, Choufi B, Delaunay J, Gourin MP, Cheze S, Ravoet C, Ferrant A, Escoffre-Barbe M, Aljassem L, Raffoux E, Itzykson R, Ades L, Dreyfus F, Fenaux P. Long-term outcome of anemic lower-risk myelodysplastic syndromes without 5q deletion refractory to or relapsing after erythropoiesis-stimulating agents. Leukemia. 2013b;27(6):1283–90.
Toma A, Kosmider O, Chevret S, Delaunay J, Stamatoullas A, Rose C, Beyne-Rauzy O, Banos A, Guerci-Bresler A, Wickenhauser S, Caillot D, Laribi K, De Renzis B, Bordessoule D, Gardin C, Slama B, Sanhes L, Gruson B, Cony-Makhoul P, Chouffi B, Salanoubat C, Benramdane R, Legros L, Wattel E, Tertian G, Bouabdallah K, Guilhot F, Taksin AL, Cheze S, Maloum K, Nimuboma S, Soussain C, Isnard F, Gyan E, Petit R, Lejeune J, Sardnal V, Renneville A, Preudhomme C, Fontenay M, Fenaux P, Dreyfus F. Lenalidomide with or without erythropoietin in transfusion-dependent erythropoiesis-stimulating agent-refractory lower-risk MDS without 5q deletion. Leukemia. 2016;30(4):897–905.
Macdougall IC, Casadevall N, Locatelli F, Combe C, London GM, Di Paolo S, Kribben A, Fliser D, Messner H, McNeil J, Stevens P, Santoro A, De Francisco AL, Percheson P, Potamianou A, Foucher A, Fife D, Merit V, Vercammen E, P. S. Group. Incidence of erythropoietin antibody-mediated pure red cell aplasia: the Prospective Immunogenicity Surveillance Registry (PRIMS). Nephrol Dial Transplant. 2015;30(3):451–60.
Park S, Hamel JF, Toma A, Kelaidi C, Thépot S, Campelo MD, Santini V, Sekeres MA, Balleari E, Kaivers J, Sapena R, Götze K, Müller-Thomas C, Beyne-Rauzy O, Stamatoullas A, Kotsianidis I, Komrokji R, Steensma DP, Fensterl J, Roboz GJ, Bernal T, Ramos F, Calabuig M, Guerci-Bresler A, Bordessoule D, Cony-Makhoul P, Cheze S, Wattel E, Rose C, Vey N, Gioia D, Ferrero D, Gaidano G, Cametti G, Pane F, Sanna A, Germing U, Sanz GF, Dreyfus F, Fenaux P. Outcome of lower-risk patients with myelodysplastic syndromes without 5q deletion after failure of erythropoiesis-stimulating agents. J Clin Oncol. 2017;35(14):1591–7. https://doi.org/10.1200/JCO.2016.71.3271. Epub 2017 Mar 28.
Moyo V, Lefebvre P, Duh MS, Yektashenas B, Mundle S. Erythropoiesis-stimulating agents in the treatment of anemia in myelodysplastic syndromes: a meta-analysis. Ann Hematol. 2008;87(7):527–36.
Itzykson R, Ayari S, Vassilief D, Berger E, Slama B, Vey N, Suarez F, Beyne-Rauzy O, Guerci A, Cheze S, Thomas X, Stamatoullas A, Gardembas M, Bauduer F, Kolb A, Chaury MC, Legros L, Damaj G, Chermat F, Dreyfus F, Fenaux P, Ades L. Is there a role for all-trans retinoic acid in combination with recombinant erythropoietin in myelodysplastic syndromes? A report on 59 cases. Leukemia. 2009;23(4):673–8.
Ferrero D, Darbesio A, Giai V, Genuardi M, Dellacasa CM, Sorasio R, Bertini M, Boccadoro M. Efficacy of a combination of human recombinant erythropoietin + 13-cis-retinoic acid and dihydroxylated vitamin D3 to improve moderate to severe anaemia in low/intermediate risk myelodysplastic syndromes. Br J Haematol. 2009;144(3):342–9.
Gianelli U, Fracchiolla NS, Bucciarelli P, Ferla V, Boiocchi L, Savi F, Moro A, Reda G, Bosari S, Cortelezzi A. High levels of vascular endothelial growth factor protein expression are associated with an increased risk of transfusion dependence in myelodysplastic syndromes. Am J Clin Pathol. 2013;139(3):380–7.
Legros L, Slama B, Karsenti JM, Vey N, Natarajan-Ame S, Watel E, Richard B, Bouabdallah K, Mannone L, Benchetrit M, Touitou I, Huault S, Durivault J, Ambroseti D, Hueber AO, Fenaux P, Dreyfus F, M. Groupe Francophone des. Treatment of myelodysplastic syndromes with excess of blasts by bevacizumab is well tolerated and is associated with a decrease of VEGF plasma level. Ann Hematol. 2012;91(1):39–46.
Bouscary D, Legros L, Tulliez M, Dubois S, Mahe B, Beyne-Rauzy O, Quarre MC, Vassilief D, Varet B, Aouba A, Gardembas M, Giraudier S, Guerci A, Rousselot P, Gaillard F, Moreau A, Rousselet MC, Ifrah N, Fenaux P, Dreyfus F. A non-randomised dose-escalating phase II study of thalidomide for the treatment of patients with low-risk myelodysplastic syndromes: the Thal-SMD-2000 trial of the Groupe Francais des Myelodysplasies. Br J Haematol. 2005;131(5):609–18.
Tamburini J, Elie C, Park S, Beyne-Rauzy O, Gardembas M, Berthou C, Mahe B, Sanhes L, Stamatoullas A, Vey N, Aouba A, Slama B, Quesnel B, Vekhoff A, Sotto JJ, Vassilief D, Al-Nawakil C, Fenaux P, Dreyfus F, Bouscary D. Effectiveness and tolerance of low to very low dose thalidomide in low-risk myelodysplastic syndromes. Leuk Res. 2009;33(4):547–50.
Raza A, Reeves JA, Feldman EJ, Dewald GW, Bennett JM, Deeg HJ, Dreisbach L, Schiffer CA, Stone RM, Greenberg PL, Curtin PT, Klimek VM, Shammo JM, Thomas D, Knight RD, Schmidt M, Wride K, Zeldis JB, List AF. Phase 2 study of lenalidomide in transfusion-dependent, low-risk, and intermediate-1 risk myelodysplastic syndromes with karyotypes other than deletion 5q. Blood. 2008;111(1):86–93.
Komrokji RS, Lancet JE, Swern AS, Chen N, Paleveda J, Lush R, Saba HI, List AF. Combined treatment with lenalidomide and epoetin alfa in lower-risk patients with myelodysplastic syndrome. Blood. 2012;120(17):3419–24.
McGraw KL, Basiorka AA, Johnson JO, Clark J, Caceres G, Padron E, Heaton R, Ozawa Y, Wei S, Sokol L, List AF. Lenalidomide induces lipid raft assembly to enhance erythropoietin receptor signaling in myelodysplastic syndrome progenitors. PLoS One. 2014;9(12):e114249.
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, Stone RM, Nelson D, Powell BL, DeCastro CM, Ellerton J, Larson RA, Schiffer CA, Holland JF. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol. 2002;20(10):2429–40.
Garcia-Manero G, Gore SD, Kambhampati S, Scott B, Tefferi A, Cogle CR, Edenfield WJ, Hetzer J, Kumar K, Laille E, Shi T, MacBeth KJ, Skikne B. Efficacy and safety of extended dosing schedules of CC-486 (oral azacitidine) in patients with lower-risk myelodysplastic syndromes. Leukemia. 2016;30(4):889–96.
Thepot S, Ben Abdelali R, Chevret S, Renneville A, Beyne-Rauzy O, Prebet T, Park S, Stamatoullas A, Guerci-Bresler A, Cheze S, Tertian G, Choufi B, Legros L, Bastie JN, Delaunay J, Chaury MP, Sanhes L, Wattel E, Dreyfus F, Vey N, Chermat F, Preudhomme C, Fenaux P, Gardin C, M. Groupe Francophone des. A randomized phase II trial of azacitidine +/- epoetin-beta in lower-risk myelodysplastic syndromes resistant to erythropoietic stimulating agents. Haematologica. 2016;101(8):918–25.
Arlet JB, Guillem F, Lamarque M, Dussiot M, Maciel T, Moura I, Hermine O, Courtois G. Protein-based therapeutic for anemia caused by dyserythropoiesis. Expert Rev Proteomics. 2016;6:1–10.
Mies A, Hermine O, Platzbecker U. Activin receptor II ligand traps and their therapeutic potential in myelodysplastic syndromes with ring sideroblasts. Curr Hematol Malig Rep. 2016;11(6):416–24.
Platzbecker U, Germing U, Götze KS, Kiewe P, Mayer K, Chromik J, Radsak M, Wolff T, Zhang X, Laadem A, Sherman ML, Attie KM, Giagounidis A. Luspatercept for the treatment of anaemia in patients with lower-risk myelodysplastic syndromes (PACE-MDS): a multicentre, open-label phase 2 dose-finding study with long-term extension study. Lancet Oncol. 2017;18(10):1338–47. https://doi.org/10.1016/S1470-2045(17)30615-0. Epub 2017 Sep 1.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Park, S., Götze, K. (2018). Erythropoiesis-Stimulating Agents in Low-Risk MDS. In: Platzbecker, U., Fenaux, P. (eds) Myelodysplastic Syndromes . Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-319-76879-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-76879-3_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-76878-6
Online ISBN: 978-3-319-76879-3
eBook Packages: MedicineMedicine (R0)