Abstract
In the absence of genetic abnormalities, the diagnoses of myelodysplastic syndromes (MDS) is primarily based on the presence of dysplasia in blood and marrow cells. Currently, there is no standardized approach to evaluate dysplasia. International cooperative study groups like the European Working Group on MDS in Childhood (EWOG-MDS) depend, however, on a concordance in diagnoses by their national reference centres for morphology. In EWOG-MDS, the morphological diagnoses of all cases enrolled from Scandinavia, the Netherlands, Germany, the Czech Republic, Austria and Italy are established by five experienced pathologists or hematologists cooperating in a morphology board. To study their concordance in evaluating myelodysplastic disorders, members of the morphology board initiated blinded reviews of smears of blood and bone marrow aspirates of known cases. Four features of dysplasia in granulopoiesis, erythropoiesis and megakaryopoiesis were assessed on May–Grünwald–Giemsa stained smears. In a final review of six blinded cases, good concordance for these features was achieved among the five observers. Accurately defined and restrictively applied cellular features of dysplasia are an important tool to improve and ensure the concordance in the diagnosis of MDS among investigators. For cooperative groups, agreement on the evaluation of the morphological assessment of dysplasia is a prerequisite.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndromes (MDS) are clonal bone marrow disorders which generally present with peripheral blood cytopenia. They are common hematological diseases in the elderly but rarely observed in childhood [10]. In children, dysplastic features of hematopoietic cells are far more common in benign disorders, and the presence of dysplastic features does not necessarily imply MDS. On the other hand, myelodysplasia can be quite subtle in some cases of low-grade MDS. In the absence of markers of clonality, the diagnosis of MDS may be difficult to establish and will depend on the recognition of dysplastic features [11].
The FAB classification of MDS [4] has applied morphological criteria to differentiate five subtypes: refractory anaemia (RA), RA with ring sideroblasts (RARS), RA with excess of blasts (RAEB), RAEB in transformation (RAEB-T) and chronic myelomonocytic leukemia (CMML). The subsequent WHO classification of hematological malignancies incorporated specific genetic abnormalities [8]. It also recognised juvenile myelomonocytic leukemia (JMML) as a separate entity within a new category of myelodysplastic/myeloproliferative disorders. To class the specific disorders observed in childhood, a pediatric approach to the WHO classification has recently been published [11]. The authors also defined minimal diagnostic criteria for MDS in childhood. Here, we report on the efforts of the members of the Morphology Board of the European Working Group of Myelodysplastic Syndrome in Childhood (EWOG-MDS) to standardize their morphological diagnoses.
Materials and methods
A series of bone marrow (BM) and peripheral blood (PB) smears stained with May–Gruenwald Giemsa was selected on the basis of a previous diagnosis of MDS in children or adults (Tab. 1). They were circulated blindly among the members of the Morphology Board (A.C.R., E.W., G.K., I.B. and S.F.) on four different occasions. The aim was to evaluate the degree of concordance among the observers for diagnostic conclusion and recognition of dysplastic features. The first three circulations included four observers, respectively, and the fourth circulation included five observers. No clinical information was provided to the reviewers.
In the first circulation of 18 cases, observers had to decide on the diagnosis (including FAB subtype) and score dysplasia of a given cytological feature qualitatively into absent, slight or strong. Each observer examined at least 400 cells of every case, and the individual results were compared and discussed (Table 2). Subsequently, two further circulations were performed with five and eight cases, respectively. In these circulations, the observers had to report the percentage of dysplastic cells of all three cell lineages. Again, the results were discussed in detail. To measure the agreement achieved with this procedure, a final circulation of six cases was performed. The results are reported here.
Description of dysplastic features
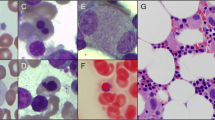
Figure 1 depicts a cartoon of erythroid, granulopoietic and megakaryopoietic cells with the four dysplastic features analysed in each cell lineage. As a general principle, it was decided that a cell was considered dysplastic for a given parameter when the changes were unequivocal.
Erythroid series
Megaloblastoid changes: at least 1.5 times the size of a normal poly- or orthochromatic erythroblast with coarse condensation of chromatin and an increased nuclear-to-cytoplasmic ratio or orthochromatic erythroblasts with decreased nuclear-to-cytoplasmic ratio and at least double the size of a normal erythrocyte of the same maturational state. Nuclear lobulation: presence of erythroblasts with lobulated nuclei (kidney-shaped, bilobulated, multilobulated, bizarre irregular nuclear profile). Multinuclearity: two or more distinctly separated nuclei of the same or of different sizes. Cytoplasmic granules or inclusions: presence of granules or nuclear fragments that can be definitely differentiated from ribosomal RNA.
Myeloid series
Bizarre nuclear shape: abnormal nuclear shape, including irregularly lobulated nuclei of segmented granulocytes with chromatin clumping or large twisted bands, large bands or metamyelocytes, multinuclearity (two distinctly separated neutrophilic bands or segmented nuclei). A- or hypogranularity: this feature must be pronounced to be regarded as abnormal, neutrophil or azurophil granules have to be markedly or completely absent and the cytoplasm of mature neutrophilic granulocytes has to stain pale blue/gray or translucent in the Romanowsky–Giemsa stain. All maturation stages except blast cells should be affected. Nuclear/cytoplasmic (N/C) asynchrony: mature neutrophilic granulocytes and metamyelocytes with basophilic cytoplasm and myelocytes with neutrophilic cytoplasm. Pseudo-Pelger anomaly: mature granulocytes with either a centrally located round to ovoid nucleus (monolobated type) or two round nuclei of similar size connected by a slender chromatin bridge (bilobated type).
Megakaryocytic series
Micromegakaryocyte: mononucleated megakaryocyte with a size comparable to that of a promyelocyte or less, lacking features of a blast cell. Small binucleated megakaryocyte: small megakaryocyte with the size of a micromegakaryocyte or slightly larger, with two round well-separated nuclei. Megakaryocyte with small round separated nuclei: megakaryocytes of any size with multiple, at least three, round separated nuclei. Megakaryocytes with nonlobated round nucleus: megakaryocytes of normal or reduced size with a nonlobated round nucleus and a mature granular cytoplasm.
For the erythroid and myeloid lineage, 100 cells from each lineage were screened for the presence of the dysplastic features described above. For megakaryopoiesis, the number of dysplastic megakaryocytes as well as the total number of megakaryocytes observed was registered. This was necessary because low-risk MDS in childhood is often hypoplastic, and it is not unusual to find a low number, i.e. less than ten megakaryocytes per bone marrow smear.
Evaluation of concordance
To evaluate the concordance among the five observers during the final circulation of slides, the percentage of dysplastic erythroid and myeloid cells was analysed in three categories: 0–10, 11–20 and >20%. For the megakaryocytic series, absolute numbers were evaluated in two groups: zero to ten and greater than ten dysplastic cells. Results were considered concordant when all five observers agreed on the same group or when the highest and lowest percentages recorded by the reviewers were less than ten points apart. Results were considered partially concordant when four observers agreed, and the highest and lowest percentages given were more than ten points apart. All other cases were judged nonconcordant.
Results
In the first circulation of slides, agreement on the diagnoses including FAB subtype among all four observers was noted in nine of the 18 cases. In two cases of refractory anaemia, MDS was excluded by one observer because of a low degree of dysplasia. A case of CMML was judged as RAEB by another observer. In three cases, a diagnosis of AML (M6 in two cases, M7 in one) was suggested by one observer because of a blast percentage above 30%. Similarly, in another three cases, RAEB-t instead of RAEB was favoured by some observers (Table 2). There was little concordance on the evaluation of dysplasia. Megaloblastoid features of red cells, nuclear/cytoplasmic asynchrony in myeloid cells and all features of dysmegakaryopoiesis were discussed most controversially (data not shown).
Features of dysplasia with complete or partial concordance and with no concordance after the fourth and final review of six cases are shown in Fig. 2.
Discussion
Myelodysplastic syndrome comprises a group of stem cell disorders with considerable clinical and morphological heterogeneity. In the absence of chromosomal abnormalities, the diagnosis is based on the morphology of BM and PB cells which is characteristic but not specific for MDS. Criteria to diagnose cytological dysplasia have been laid down by the FAB group and others [2, 4, 6, 12, 16]. For each hematopoietic cell lineage, several dysplastic changes are defined. However, a stringent description of the dysplastic features to introduce reproducibility in the evaluation of dysplasia is missing. In preparation for prospective multicentre trials, the EWOG-MDS Morphology Board started intensive discussions and slide rounds to evaluate myelodysplasia. Cartoons were used for the distinct, unequivocal illustration of the dysplastic cell changes (Fig. 1). It became evident that a clear description of the characteristics as well as detailed images of dysplasia are necessary for a reproducible identification not only of ambiguous features like hypogranularity in granulopoiesis, but also for the seemingly more objective features like multinuclearity or cytoplasmic granulation in erythroid precursors. Furthermore, for some features like hypogranularity, an exact definition is indispensable because variations in the May–Gruenwald Giemsa staining (particularly in the pH of staining solutions) may alter the cytological details [20]. While in the first circulation of slides there was little concordance with respect to the grading of dysplasia, between observers, consensus steadily increased with continuous reviews and discussions. After the last review, full agreement was achieved for nuclear lobulation, multinuclearity and cytoplasmic inclusions in the erythroid series as well as bizarre nuclear shape, nucleus/cytoplasmic asynchrony and pseudo-Pelger anomaly in the myeloid series. The same applied to dysmegakaryopoietic features which had been discussed most controversially at the beginning of the cooperation. The dysplastic features most difficult to achieve consensus on were megaloblastosis in erythropoiesis and hypogranularity in granulopoiesis (Fig. 2).
Several studies have addressed the impact of morphology on prognosis in adulthood MDS [2, 12, 13, 16, 18, 19]. The most significant morphological impact on prognosis is the blast cell count [7]. There is also some indication that lineage dysplasia is relevant for the outcome of the disease [16]. However, these studies are inconsistent with one another. In one study, megaloblastosis was an unfavourable feature, whereas granulopoietic hypogranulation improved prognosis [16]. In two other studies, megaloblastoid changes were correlated with a better prognosis, whereas the presence of pseudo-Pelger cells and granulopoietic hypogranularity had a negative impact on survival [13, 16, 17]. The MDS subtype refractory cytopenia with multilineage dysplasia (RCMD), which was introduced by the WHO classification, is thought to be correlated with a worse prognosis compared to refractory anaemia with single erythroid dysplasia [8]. In a study of Nösslinger et al., the FAB and WHO classification of MDS were compared. In contrast to the WHO classification, the authors did not find evidence for an inferior prognosis of RCMD compared to RA. As the authors stated, one reason for the disagreement might be the lack of an exact definition of dysplasia, especially the percentage of dysplastic cells in each cell lineage [5, 14].
In childhood, the impact of myelodysplasia on the outcome of MDS has not been investigated. Preliminary data from EWOG-MDS demonstrate a relationship between the degree of dysplasia and the FAB subtype [3]. Dysplasia increases from RA towards RAEB and RAEB-t. This result is primarily due to an increased dysgranulopoiesis in RAEB and RAEB-t compared to that observed in RA. Interestingly, the percentage of dyserythropoietic cells did not differ significantly between the different FAB subtypes [3].
Dysplastic cell changes can also occur in congenital bone marrow failure disorders [9]. It is still not settled whether the quality or quantity of dysplasia in these conditions can be distinguished from that observed in MDS. In Fanconi anaemia, an autosomal recessive disorder characterized by bone marrow failure and progression to MDS, some authors claimed that bone marrow morphology, particularly myelodysplasia, was a more important indicator for transition to MDS than standard cytogenetics [1]. Again, this observation confirms the need for a strict definition on myelodysplasia since Fanconi anaemia itself has dysplastic features.
In conclusion, with a precise description and cartoons of dysplastic features as well as a number of slide rounds with intensive discussions, we are able to achieve a considerable concordance for measuring dysplasia among the five observers of the EWOG-MDS Morphology Board. This concordance includes even previously vaguely defined cytological criteria like megaloblastoid changes in erythropoiesis or hypogranulation in granulopoiesis. The agreement on the evaluation of dysplasia will be important for multinational prospective trials in this rare disorder in childhood [15].
References
Alter BP, Caruso JP, Drachtman RA, Uchida T, Velagaleti GV, Elghetany MT (2000) Fanconi anemia: myelodysplasia as a predictor of outcome. Cancer Genet Cytogenet 117(2):125–131
Aul C, Giagounidis A, Germing U, Ganser A (2002) Evaluating the prognosis of patients with myelodysplastic syndromes. Ann Hematol 81(9):485–497
Baumann I, Cantu-Rainoldi A, Kerndrup G, Fenu S, van Wering E, Fischer A, Schmitt-Gräff A, Müller S, Rogge T, Nöllke P, Niemeyer CM (2000) Morphological and histopathological features in childhood MDS and JMML: experience of the EWOG-MDS Morphology Board. Leukemia 14:957
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C (1982) Proposals for the classification of the myelodysplastic syndromes. Br J Haematol 51(2):189–199
Dunkley SM, Manoharan A, Kwan YL (2002) Myelodysplastic syndromes: prognostic significance of multilineage dysplasia in patients with refractory anemia or refractory anemia with ringed sideroblasts. Blood 99(10):3870–3871
Goasguen JE, Bennett JM (1992) Classification and morphologic features of the myelodysplastic syndromes. Semin Oncol 19(1):4–13
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, Ohyashiki K, Toyama K, Aul C, Mufti G, Bennett J (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89(6):2079–2088
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, Lister TA, Bloomfield CD (2000) The World Health Organization classification of neoplastic diseases of the haematopoietic and lymphoid tissues: report of the clinical advisory committee meeting, Airlie House, Virginia, November 1997. Histopathology 36(1):69–86
Hasle H (1994) Myelodysplastic syndromes in childhood-classification, epidemiology, and treatment. Leuk Lymphoma 13(1–2):11–26
Hasle H, Niemeyer CM (2002) Myelodysplastic syndrome and juvenile myelomonocytic leukemia in children. In: Bennett JM (eds) The myelodysplastic syndromes. Marcel Dekker Inc., New York, pp 299–344
Hasle H, Niemeyer CM, Chessells JM, Baumann I, Bennett JM, Kerndrup G, Head DR (2003) A pediatric approach to the WHO classification of myelodysplastic and myeloproliferative diseases. Leukemia 17(2):277–282
Matsuda A, Jinnai I, Yagasaki F, Kusumoto S, Minamihisamatsu M, Honda S, Murohashi I, Bessho M, Hirashima K (1998) Refractory anemia with severe dysplasia: clinical significance of morphological features in refractory anemia. Leukemia 12(4):482–485
Matsuda A, Jinnai I, Yagasaki F, Kusumoto S, Murohashi I, Bessho M, Hirashima K, Honda S, Minamihisamatsu M, Fuchigami K, Matsuo T, Kuriyama K, Tomonaga M (1999) New system for assessing the prognosis of refractory anemia patients. Leukemia 13(11):1727–1734
Nösslinger T, Reisner R, Koller E, Gruner H, Tuchler H, Nowotny H, Pittermann E, Pfeilstocker M (2001) Myelodysplastic syndromes, from French-American-British to World Health Organization: comparison of classifications on 431 unselected patients from a single institution. Blood 98(10):2935–2941
Rogge T, Niemeyer CM (2000) Myelodysplastic syndromes in childhood. Onkologie 23:18–24
Tassin F, Dewe W, Schaaf N, Herens C, Ravoet C, Albert A, Beguin Y, Paulus JM (2000) A four-parameter index of marrow dysplasia has predictive value for survival in myelodysplastic syndromes. Leuk Lymphoma 36(5–6):485–496
Tennant GB, Cavill I, Burnett AK (2004) Long-term survival of myelodysplastic patients with macrocytosis. Br J Haematol 124(6):840–841
Verburgh E, Achten R, Maes B, Hagemeijer A, Boogaerts M, Wolf-Peeters C, Verhoef G (2003) Additional prognostic value of bone marrow histology in patients subclassified according to the international prognostic scoring system for myelodysplastic syndromes. J Clin Oncol 21(2):273–282
Wells DA, Benesch M, Loken MR, Vallejo C, Myerson D, Leisenring WM, Deeg HJ (2003) Myeloid and monocytic dyspoiesis as determined by flow cytometric scoring in myelodysplastic syndrome correlates with the IPSS and with outcome after hematopoietic stem cell transplantation. Blood 102(1):394–403
Baumann I, Gunzer U, Aus HM (1987) Influence of pH, buffer systems and Di-K-EDTA on Standard-Romanowsky-Giemsa staining and the effect in both cellular architecture and color measured in peripheral blood. Cytol Cytometry Suppl 35(1):170
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Cantù Rajnoldi, A., Fenu, S., Kerndrup, G. et al. Evaluation of dysplastic features in myelodysplastic syndromes: experience from the morphology group of the European Working Group of MDS in Childhood (EWOG-MDS). Ann Hematol 84, 429–433 (2005). https://doi.org/10.1007/s00277-005-1034-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-005-1034-4