Abstract
During the last 10 years, three European phase II studies were performed to investigate the treatment of elderly patients with myelodysplastic syndrome (MDS) with low-dose 5-aza-2′-deoxycytidine (decitabine, DAC). All these European trial data were reviewed on the basis of the International Prognostic Scoring System (IPSS) risk criteria and the response criteria as recently published by an international working group. To investigate the results in a larger cohort of patients and to determine risk factors, all data were pooled with some observations from the PCH 95-06 US phase II study. The response rate in the 177 patients evaluated (median age 70 years) was 49%. The median response duration was 36 weeks, and the median survival was 15 months. Analysis of the data according to sex, age, French–American–British classification, percentage of blasts in the bone marrow, IPSS risk group, lactate dehydrogenase and cytogenetics did not reveal any factor predictive of response. Overall, 69% of patients benefited, including those with stable disease during therapy. Response duration was significantly shorter with increasing risk (according to the IPSS classification). Haemoglobin level and neutrophil count showed an inverse correlation to the IPSS classification. Univariate analysis showed a significantly inferior survival for elderly patients (>75 years of age) and for those with high levels of serum lactate dehydrogenase (LDH) (more than two times the normal values). Patients with high-risk cytogenetic abnormalities according to the IPSS risk criteria showed better overall survival than those with intermediate-risk abnormalities. When analysed according to the IPSS risk classification, high-risk patients had worse survival prospects following decitabine therapy than those with intermediate risk; however, compared to the originally reported IPPS outcomes for high-risk patients, they probably showed better survival. During the treatment period, 18% of the patients progressed towards acute leukaemia. Decitabine showed a rather low toxicity profile in this elderly patient group. In conclusion, low-dose decitabine is an active drug for the treatment of MDS patients, even for those older than 75 years with bad prognostic characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gene silencing of potential tumour suppressor genes is probably one of the critical events in the development of several forms of cancer [6]. Methylation of a transgene promoter correlates with transcriptional gene silencing, and in many tumours, hypermethylation of promoters of important malignancy-related genes has been described. Aberrant methylation of promoter-associated cytosine–guanine (CpG) islands is an epigenetic modification found in cancer patients. In patients with myelodysplastic syndrome (MDS), hypermethylation of p15 Ink4b has been described [1, 15], which is an inhibitor of the cyclin-dependent kinase-4 and a negative regulator of the G1/S progression of the cell cycle.
DNA hypermethylation of important genes involved in the pathogenesis seems an interesting therapeutic target for the treatment of patients with an MDS. Azanucleosides, after incorporation into the DNA of dividing cells, may modulate differentiation, growth and apoptosis via upregulation of genes that are silenced by DNA methylation. Both 5-azacytidine (azacitidine, Vidaza) and 5-aza-2′-deoxycytidine (decitabine, DAC) are potent inhibitors of DNA methylation [5] and have shown clinical activity in patients with MDS [16–18]. In patients treated with decitabine, demethylation of initially hypermethylated CpG islands of the p15 INK4b gene was measured, and p15 protein expression was found to be reinduced in the myeloid precursors of these patients. In the majority of these patients, this was associated with a clinical response [7].
Since 1991, we have been treating elderly patients with high-risk MDS with low-dose decitabine, and currently, more than 170 patients have been treated in three separate phase II studies using almost the same treatment conditions. The results of the first two phase II studies (PCH 91-1 and PCH 95-11) were published previously [17, 18]. In this paper, we present the data of our third study, PCH 97-19. The data of all three European studies were pooled with the data from a single centre that participated in the US phase II study (PCH 95-06) in order to evaluate the prognostic parameters. We performed this analysis in a group of 177 patients according to the corrected International Prognostic Scoring System (IPSS) risk parameters and the response criteria as defined by an international working group [3].
Patients, materials and methods
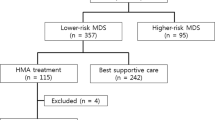
The pooled results of three European phase II studies (PCH 91-1, PCH 95-11 and PCH 97-19; performed between 1992 and 2001) and the data from a single centre that participated in a phase II study performed in the US (PCH 95-06) are analysed in this study. All data from these studies were reanalysed, updated and corrected according to an erratum of the IPSS working group [8, 9]. The results were also re-evaluated according to the newly published response criteria [3]. Furthermore, the findings of 75 new patients from the third phase II study, PCH 97-19, were included in the analysis. Data presented were collected until February 2004.
Patient's characteristics
All protocols were approved by ethical committees, and all patients provided informed consent before enrolling in the study. Patients were eligible if they had a primary MDS of one of the following subtypes [according to the French–American–British (FAB) criteria] [2]: refractory anaemia with excess of blasts (RAEB), RAEB in transformation (RAEB-T), chronic myelomonocytic leukaemia (CMML) and refractory anaemia (RA) or refractory anaemia with ringed sideroblasts (RARS); with a transfusion requirement that exceeded three units of red blood cells (RBCs) or six units of platelets per 6 weeks and had not previously been treated with chemotherapy. In the PCH 91-1 study, two patients with a secondary acute myeloid leukaemia (sAML) slowly progressing from MDS with a blast cell count 30–40% were included. Furthermore, patients with malignancies, in addition to MDS, not treated with chemotherapy were also enrolled. In all studies, normal renal and liver function was required. Only a moderate elevation of liver enzyme levels (maximum 2× normal) was allowed if suspected to be caused by the underlying MDS. Cardiac function was required to be normal. Only patients with an Eastern Cooperative Oncology Group (ECOG) performance status of 0, 1 or 2 were allowed to enter the study.
A total of 177 patients were analysed: 53 women and 124 men, with a median age of 70 years (range 38–89). Table 1 lists the distribution of the patients according to the FAB subtype and the IPSS risk score (measured at the start of the treatment protocol). The majority (72%) of the patients had an intermediate (INT)-2 or high-risk score, indicative of an extremely poor outcome in elderly patients [9]. No IPSS low-risk patients were enrolled.
Cytogenetic baseline analyses were performed in 169/177 (95%) of the patients but were uninformative in 18 cases. The IPSS risk score of these 26 patients without cytogenetic data was based on the other available data; thus, the risk might be underestimated in these patients. Chromosomal abnormalities were found in 52% of the patients. For the cytogenetic abnormalities in the different risk groups, see Table 2.
Therapy
In study PCH 91-1, decitabine was given to the first 21 patients by continuous infusion (50 mg/m2/24 h), and the dose was increased to 65 and 75 mg/m2/24 h if no response was observed. In the remaining eight patients in this study, doses were fixed at 40 mg/m2/24 h. In the other studies, a fixed dose of three times 15 mg/m2/24 h was given (=45 mg/m2/24 h) as 4-h infusions (PCH 95-11 and PCH 97-19) or as 3-h infusions (PCH 95-06). A therapy cycle consisted of the drug administration on 3 consecutive days every 6 weeks provided that haematological recovery had occurred before patients started a new cycle or, in case of a low blood cell count, that the haematological parameters had at least reached pretreatment values. No dose reduction was allowed. The effect of the therapy was first evaluated by bone marrow aspirate after the second cycle. In case of a complete response (CR), two more courses of therapy were given, and therapy was stopped if the CR persisted. When an improvement, partial response (PR) or stable disease was achieved, two more cycles were given, with a maximum of six courses in studies PCH 91-1 and PCH 95-11 and eight in the PCH 97-19 study. The therapy was stopped in case of progressive disease.
Response criteria
Responses were evaluated according the newly described response criteria proposed by an international working group [3]. A CR was scored when less than 5% of blast cells were found in the bone marrow with a normal haemoglobin (Hb) concentration and cell count for neutrophilic granulocytes and platelets. According to the guidelines for CR, “no evidence for dysplasia” should be present [9]. In practice, this is difficult to evaluate since (subtle) dysplastic features are often found during treatment. Cytogenetic responses were observed; these data are published elsewhere [13]. Haematologic improvements were classified as major and minor responses as proposed by an international working group [3].
Response duration (in weeks) was defined as the time from best response to the moment of returning to baseline values for the blood cell counts or the first transfusion to occur after the patients had become transfusion-independent. Toxic death was defined as all deaths during the whole period of the decitabine therapy not occurring due to disease progression.
Statistical methods
Response data are presented on the basis of intention to treat (ITT) (n=177). Response rates were compared using the Chi square test, and trends were analysed by linear-by-linear association analysis. The median response duration with the 95% confidence interval (CI) and the survival were estimated using Kaplan–Meier curves, and subgroups were compared using log rank test. Median survival estimates were provided with 95% CI. For these analyses, the SPSS 11.0 statistical programme was used. Multivariate analyses were performed using Cox regression analysis.
Results
Analyses were performed on the ITT population (n=177) that contained 12 patients not evaluable for response according to the protocol. These 12 patients received only one cycle of therapy without signs of disease progression, three of them because they refused further therapy and nine due to persistent cytopenia, therefore not qualifying for the next cycle. Toxic death was seen in 12 patients (6.8%) and was higher in earlier studies. The cause of death was almost always infection or bleeding due to disease- or therapy-related pancytopenia. At least three patients died of causes not disease-related. Disease progression during therapy, mostly towards an acute leukaemia, was observed in 32 (18%) of the patients. The median number of cycles given to the patients was four for all three studies.
Response rate
The overall response rate was 49% (86/177), with a complete remission rate of 24% (for the results of the individual studies, see Table 3). A substantial number of patients achieved stable disease during the therapy (20%). When patients with stable disease were included, 69% of the patients possibly benefited from decitabine therapy.
No significant differences in response rate were seen between male and female patients (47 vs 53%) (Table 4). Although elderly patients above the age of 75 years had a somewhat lower response rate, the differences seen for each age group were also not significant (Table 4). The response rates were evaluated according to bone marrow blast count, the FAB classification (including CMML) and the IPSS risk groups (Table 4). Patients with a higher risk did not have a lower response rate than patients in the lower risk group. Patients with no cytogenetic abnormalities or low-risk cytogenetic abnormalities (including those where no metaphases could be obtained) showed the same response rate as patients with high-risk abnormalities. Neither high LDH levels nor type or number of cell line deficiencies were prognostic factors. None of all the parameters shown in Table 4 were predictive for a response to therapy.
Response duration
The median response duration was 36 weeks (range 12–147 weeks; 95% CI 32–42 weeks, n=86). When also including those patients with a stable disease (n=122), the median response duration was 33 weeks (range 8–147 weeks; 95% CI 31–41 weeks).
Response duration was analysed according to multiple parameters (Table 5). Most of these parameters had no significant effect on the response duration using univariate analysis. Response rates in CMML patients were not lower than those in other FAB subtypes. When analysing patients according to the FAB classification, excluding CMML, the median response duration was 41, 35 and 37 weeks for RA, RAEB and RAEB-T (p=0.247), respectively. Significant differences in response duration based on the IPSS category were observed; INT-1 patients had a response duration of 50 weeks, compared to 32 weeks for the high-risk group (p=0.043). Platelet count at the start of the therapy was not a predictive factor. However, neutrophil count or haemoglobin concentration showed a very strong inverse relation, meaning that patients with either a neutropenia or anaemia had a longer response duration compared to patients with normal counts. Accordingly, the response duration was longer when three cell lines were deficient.
Survival
Since IPSS risk group and survival were scored for these patients from start of therapy and not from diagnosis, we could not compare the survival of the different IPSS subgroups with the original data of the IPSS publication or with other studies. At the time of evaluation, 154/177 patients had died.
The overall median survival of the whole patient group was 15 months (95% CI 12.5–17.5 months), with 31% of patients alive at 2 years. A significant decrease in survival was seen with age (Table 6). There was a trend towards a decrease in survival time with an increase in bone marrow blast cell percentage, but this did not reach a statistical significance. When CMML patients (with <20% blasts; not recognized by the WHO criteria as “pure” MDS) were excluded, the survival difference for the different FAB subgroups was also not statistically significant (p=0.134). Significant differences were observed for those patients who showed an increased LDH level as well as for the different cytogenetic subgroups. However, patients with intermediate-risk cytogenetic abnormalities had shorter median survival than those with high-risk abnormalities (chromosome 7 abnormalities or multiple abnormalities). When analysed by the IPSS risk score (which takes into account blasts count, cytogenetic abnormalities and cell line deficiencies), high-risk patients showed lower survival than patients with INT-2 and INT-1, respectively (Fig. 1). No differences were seen for different cell lines.
Multivariate analysis
Multivariate analysis for survival according to the defined risk factors was carried out by Cox regression analysis (see Table 7). In contrast with the findings of the group who defined the IPSS risk score, we did not observe a significant contribution of either Hb, absolute neutrophil count (ANC) and platelets alone or in combination. Significant was the contribution of blast cell count and cytogenetics as reflected in the IPSS. LDH and age were additional parameters, with LDH having the strongest predictive weight. The variables in the equation had the following outcome: IPSS p=0.0024; Exp(B) 1.274, LDH p=0.001 Exp(B) of 1.453 and age p=0.007 with an Exp(B) of 1.396.
The effect of time of the diagnosis on survival
For 15 patients, the exact date of diagnosis was not known. Almost half of the patients began treatment 4 or more months after diagnosis. The overall survival from diagnosis was 23 months (95% CI of 19.1–26.9 months). There was a significant difference in the survival for those patients who were treated immediately after the diagnosis of MDS compared with those in whom the diagnosis was made 4 or more months prior to decitabine therapy. Patients who started treatment immediately after diagnosis had a median survival from start of therapy of 13 months (95% CI 9.3–16.6 months, n=76), compared to 18 months (95% CI 12.8–23.2 months, n=79) for late starters (p=0.023). When the cut-off was 1 year, the difference was even more pronounced (Fig. 2), with a median survival of 13 (n=111) and 25 months (n=44) and a 2-year survival of 25 and 50% (p<0.001) for immediate and late starters, respectively. When comparing immediate or delayed treatment for the different IPSS risk groups, we observed a significant difference for the INT-1 and INT-2 subgroups but not for the high-risk subgroup (see Table 8).
Survival for direct or later treatment. Probability of survival from moment of start therapy. Patients treated within 1 year of diagnosis (____) had a median survival of 13 months (95% CI 9.1–16.6), and patients treated more than 1 year after diagnosis (- - -) had a median survival of 25 months (95% CI 12.9–37.1) (p<0.001)
Toxicity
In general, the toxicity was considered to be very mild by the patients. Details of the safety outcome of PCH 91-1 and PCH 95-11 study are published elsewhere [5, 6]. Twelve patients died during therapy. Eight died due to infection, one due to cerebral haemorrhage during a thrombocytopenic phase and three due to cardiovascular complications not considered to be related to therapy.
Table 9 shows the WHO grade 3 and 4 toxicity seen in the PCH 97-19 study with 75 patients. In this study, 43 patients experienced a total of 50 febrile episodes. The mean number of days per fever episode was 9.5. Twenty-three of these infections were classified as WHO grade 3 or 4 toxicity. Most episodes occurred during the first or second cycle of therapy, when a neutropenia due to the therapy and/or disease was present.
Abnormal increases in liver enzymes (WHO grade 1–3) were seen in 12 patients (16%). Eleven of these were scored as WHO grade <2. Twenty patients experienced an increase in LDH, often after the first cycle, possibly due to tumour cell lysis or in combination with a rise in the liver enzymes.
Creatinine levels were raised in five of the 75 patients, with all changes being of WHO grade 1 severity. In the PCH 95-11 study, we observed one grade 3 renal toxicity. No other case of renal toxicity was seen.
Cardiovascular toxicity was very low, mostly considered not related or only possibly related to the study drug. One patient experienced a grade 3 atrial fibrillation (during an anaemic episode with an Hb <7.5 g/dl). Grade 3 cardiovascular problems were observed in six of the 75 patients in PCH 97-19.
Haematotoxicity is difficult to evaluate due to the already low cell counts at the start of the therapy. Therefore, we evaluated those patients who had (near) normal counts and showed a decrease in cell count during treatment. Fifteen patients experienced a drop in cell count during 20 episodes; according to the WHO scale, pancytopenia grade 2 was seen in two patients during three episodes, anaemia grade 2 in two patients, leucopenia in 10 patients during 12 episodes (three grade 3 toxicity and one grade 4) and thrombocytopenia in four patients during five episodes (two grade 3 and two grade 4).
Discussion
In this overview, we pooled the data of three European phase II studies and we added data from a single centre that participated in the US phase II study. Using low-dose decitabine in elderly patients with high-risk MDS, we observed an acceptable response rate of almost 50%. Responses were seen even in those patients with extremely bad prognostic characteristics including high-risk cytogenetic abnormalities. No correlation between the selected prognostic factors and response rate could be found. Only 18% of the patients progressed towards acute leukaemia during the treatment period.
The response duration was rather short at 36 weeks. IPSS risk score was found to be predictive for response duration. Hb level and neutrophil count were found to be (adverse) prognostic parameters. Overall survival of the group was 15 months. Age, LDH, cytogenetic findings and IPSS risk score were predictive of overall survival time. A remarkably good median survival of 15 months was seen in patients with high-risk cytogenetic abnormalities (i.e. abnormalities involving chromosome 7 or complex abnormalities [≥3]).
The IPSS risk score has been generally accepted as an indication of expected survival in an individual patient. In the analysed patient cohort, this risk score correlated with survival in patients treated with decitabine. This was not because more INT-I patients than high-risk patients reached a remission, but rather because the response duration was longer in low-risk than in high-risk patients. The IPSS risk score takes into account three independent risk factors: blast cell count, cytogenetic findings and number of cell line deficiencies. When we examined these parameters separately, none were predictive of response to therapy. There was only a small trend to increased response duration in those patients with a high blast cell count. No correlation was observed between different cytogenetic subgroups, whereas there was an inverse trend in the response duration when we looked at the number of cell line deficiencies.
When we examined the survival times, high bone marrow blast cell counts showed a trend towards inferior survival (p=0.053). Patients with intermediate-risk cytogenetic abnormalities had a shorter median survival than those with high-risk cytogenetic abnormalities. There was no correlation between the number of deficient cell lines and survival time. This suggests that decitabine might have a more pronounced effect on patients with high-risk cytogenetic abnormalities, for reasons as yet unknown. From our observations, it seems that serum LDH levels at the start of therapy are a strong predictor of outcome.
Azanucleotides are drugs successfully used in MDS patients. It is still unclear whether they exert their action by inducing growth inhibition of the pathological clone via an epigenetic pathway, e.g. the demethylation of aberrant hypermethylated proliferation-associated genes. However, CD34-positive myeloid precursors obtained from patients treated with decitabine showed a decrease in the methylation of p15 and subsequently a normalization of the protein expression [7].
At present, two azanucleotides are under investigation for clinical use in MDS patients, i.e. azacitidine and decitabine. The response rates seen with these drugs seem comparable, although the majority of the patients in the study with azacitidine were of low- or INT-1 risk, and in the present study, most patients are of INT-2 and high-risk. In the treatment arm of the azacitidine study, a CR rate of only 7% was seen [16], whereas in patients treated with decitabine reported in this paper, we observed a CR rate of 24%. Several CR patients showed a cytogenetic CR as we reported earlier [13]. In a recent update on the azacitidine phase III data, the overall response rate was corrected by the US Food and Drug Administration to a CR + PR rate of 16%, compared to the originally published 23% [10]. The limited data from studies using farnesyltransferase inhibitors show a low response rate, and this drug showed significant toxicity [12].
Currently, there is no consensus about a standard therapy for elderly patients with high-risk MDS. Low-dose cytosine arabinoside is still used, despite a randomized phase III study that failed to demonstrate survival advantage over supportive care [14]. The response rate and response duration in that study were lower than seen with decitabine. In addition, a meta-analysis concluded that low-dose cytosine arabinoside is not an appropriate standard therapy [4]. Whether azanucleotides are a real alternative for the treatment of elderly MDS patients has yet to be further evaluated in phase III studies. Other questions also remain unanswered, for example the use of alternative decitabine treatment schedules and the use of decitabine in combination to improve remission rate and response duration. With their low toxicity profile and the beneficial effects on quality of life, the azanucleotides may prove to be an interesting treatment option for elderly MDS patients [11].
References
Aoki E, Uchida T, Ohashi H, Murase T, Ichikawa A, Yamao K, Hotta T, Kinoshita T, Saito H, Murate T (2000) Methylation status of the p15ink4b gene in hematopoietic progenitors and peripheral blood cells in myelodysplastic syndrome. Leukemia 14:586–593
Bennet JM, Catovskty D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C (1982) Proposals for the classification of the myelodysplastic syndromes. Br J Haematol 74:395–408
Cheson BD, Bennett JM, Kantarjian H, Pinto A, Schiffer CA, Nimer SD, Lowenberg B, Beran M, de Witte T, Stone RM, Mittelman M, Sanz GF, Wijermans PW, Gore S, Greenberg P (2000) Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood 96:3671–3674
Cheson BD, Jaspern DM, Simon R, Friedman MA (1986) A critical appraisal of low dose cytosine arabinoside in patients with acute non lymphocytic leukaemia and myelodysplastic syndrome. J Clin Oncol 4:1857–1864
Christman JK (2002) 5-azacytidine and 5-aza-2′-deoxycytidine as inhibitors of DNA methylation: mechanistic studies and their implications for cancer therapy. Oncogene 21:5483–5495
Clark SJ, Melki J (2002) DNA methylation and gene silencing in cancer: which is the guilty party? Oncogene 21:5380–5387
Daskalakis M, Nguyen TT, Nguyen C, Goldberg P, Ko G, Wijermaqns P, Jones PA, Lübbert M (2002) Demethylation of a hypermethylated P15/INK4B gene in patients with myelodysplastic syndrome by 5-aza-2′-deoxycytidine (decitabine) treatment. Blood 100:2957–2964
Erratum (1998) Blood 91:1100
Greenberg P, Cox C, Le Bau MM, Fenaux P, Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, Ohyashi K, Toyama K, Aul C, Mufti G, Bennett J (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89:2079–2088
Kaminskas E, Farrell A, Abraham S, Baird A, Hsieh LS, Lee SL, Leighton JK, Patel H, Rahman A, Sridhara R, Wang YC, Pazdur R, FDA (2005) Approval summary: azacitidine for treatment of myelodysplastic syndrome subtypes. Clin Cancer Res 11:3604–3608
Kornblith AB, Herndon JE, Silverman LR, Demakos EP, Odchimar-Reissig R, Holland JF, Powell BL, DeCastro C, Ellerton J, Larson RA, Schiffer CA, Holland JC (2002) Impact of azacytidine on the quality of life of patients with myelodysplastic syndrome treated in a randomized phase III trial: a Cancer and Leukemia Group B Study. J Clin Oncol 15:2441–2452
Kurzrock R, Albitar M, Cortes JE, Estey EH, Faderl SH, Garcia-Manero G, Thomas DA, Giles FJ, Ryback ME, Thibault A, De Porre P, Kantarjian HM (2004) Phase II study of R115777, a farnesyl transferase inhibitor, in myelodysplastic syndrome. J Clin Oncol 22:1287–1292
Lübbert M, Wijermans P, Kunzman R, Verhoef G, Bosly A, Ravoet C, Andre M, Ferrant A (2001) Cytogenetic responses in high risk myelodysplastic syndrome following low dose treatment with the DNA methylation inhibitor 5-aza-2′-deoxycytidine. Br J Haematol 114:1–11
Miller KB, Kim K, Morrison FS, Winter JN, Bennett JM, Neiman RS, Head DR, Cassileth PA, O'Connell MJ, Kyungmann K (1992) The evaluation of low dose cytarabine in the treatment of myelodysplastic syndrome: a phase III intergroup study. Ann Hematol 65:162–168
Quesnel B, Guillerm G, Vereecque R, Wattel E, Preudhomme C, Bauters F, Vanrumbeke M, Fenaux P (1998) Methylation of the p15ink4b gene in myelodysplastic syndrome is frequent and acquired during disease progression. Blood 91:2985–2990
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, Stone RM, Nelson D, Powell BL, DeCastro CM, Ellerton J, Larson RA, Schiffer CA, Holland JM (2002) Randomized controlled trial of azacytidine in patients with the myelodysplastic syndrome: a study of the Cancer and Leukemia Group B. J Clin Oncol 20:2429–2440
Wijermans PW, Krulder JWM, Huijgens PC, Neve P (1997) Continuous infusion of low dose 5-aza-2′-deoxycytidine in elderly patients with high risk myelodysplastic syndrome. Leukemia 11:1–5
Wijermans P, Lübbert M, Verhoef G, Bosly A, Ravoet C, Andre M, Ferrant A (2002) Low dose 5-aza-2′-deoxycytidine, a DNA hypomethylating agent, for the treatment of high risk myelodysplastic syndrome: a multicenter phase II study in elderly patients. J Clin Oncol 18:956–962
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wijermans, P.W., Lübbert, M., Verhoef, G. et al. An epigenetic approach to the treatment of advanced MDS; the experience with the DNA demethylating agent 5-aza-2′-deoxycytidine (decitabine) in 177 patients. Ann Hematol 84 (Suppl 1), 9–17 (2005). https://doi.org/10.1007/s00277-005-0012-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-005-0012-1