Abstract
The DNA hypomethylating agents (HMAs) azacitidine and decitabine are currently the most frequently administered disease-modifying therapies for patients with higher-risk myelodysplastic syndromes (MDS). However, azacitidine and decitabine are not curative, the median response duration is 11–15 months, and only 10–20 % of patients experience complete hematologic and cytogenetic response. Moreover, once an HMA fails the patient, the prognosis is poor, with a median survival of less than 6 months unless the patient undergoes hematopoietic stem cell transplantation (HSCT). Recent insights into the genetic basis of MDS have enhanced biological understanding and prognostication accuracy, but these developments have not yet led to regulatory approval of new therapies. While there are multiple potential approaches to patients with MDS for whom HMAs have failed, including supportive care alone, cytotoxic therapy, lenalidomide, histone deacetylase inhibitors, and HSCT, favorable responses to these approaches are limited and new therapies are greatly needed. Here, we review clinical and biological data about the population of patients failed by HMAs, evaluate currently available approaches to patients in this clinical situation, and discuss prospects for development of novel active agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of patients with myelodysplastic syndromes (MDS) has been augmented by development of two clinically active DNA methyltransferase inhibitors, azacitidine (Vidaza; Celgene, Summit, NJ) and decitabine (Dacogen; Eisai, Woodcliff Lake, NJ), sometimes called “hypomethylating agents” (HMAs) because of their effect on global cytosine 5′ methylation. These drugs were approved by the US Food and Drug Administration (FDA) for all French-American-British (FAB) Co-operative Group subtypes of MDS in 2004 and 2006, respectively, and are now recommended by consensus guidelines for treatment of International Prognostic Scoring System (IPSS) intermediate-2- and high-risk MDS and certain populations of IPSS low- and intermediate-1-risk MDS patients [1]. Before the introduction of HMAs, the only treatment approach that could favorably influence the natural history of MDS (i.e., increase overall survival or delay progression to acute myeloid leukemia (AML)) was allogeneic hematopoietic stem cell transplantation (HSCT) [2].
The most compelling evidence of azacitidine’s disease-modifying benefit in MDS comes from the AZA-001 study, an international, multicenter trial that randomized 358 patients to receive either “conventional care” (n = 179) or azacitidine (n = 179) [3]. Conventional care included supportive care alone, low-dose cytarabine, or anthracycline-cytarabine AML induction chemotherapy. In the AZA-001 study, azacitidine was administered subcutaneously at 75 mg/m2 per day for 7 days every 28 days for a minimum of six treatment cycles. The primary endpoint was overall survival (OS), with secondary endpoints including time to AML progression, responses assessed with International Working Group (IWG) 2000 criteria [4], and adverse events. The study met the primary endpoint, as the azacitidine group experienced a median OS of 24 months compared to 15 months in the conventional care group (hazard ratio (HR) 0.58). AML transformation was also delayed, with the azacitidine group diagnosed with AML a median of 18 months after enrollment compared with 12 months for the conventional care group.
Although no survival advantage has been formally demonstrated with decitabine, it remains unclear whether that is because of differences in drug action between decitabine and azacitidine or is instead due to differences in clinical trial design and enrolled populations. Two randomized controlled trials and other prospective studies have demonstrated hematological improvement, cytoreduction of clonal cells, and improved progression-free survival (PFS) with decitabine, which is an established alternative to azacitidine in higher-risk MDS [5–10].
HMAs are now a standard first-line therapy in patients with IPSS intermediate- and high-risk MDS [11–13]. However, HMAs are not curative, and even when a complete remission (CR) is achieved, the median duration of response is only about 1 year [14]. There is no current consensus on management strategies after HMA failure. Here, we review patterns of HMA failure and potential approaches to patients who have been failed by an HMA.
Hypomethylating Agent Failure Patterns and Prognosis
Understanding the nature of HMA response and failure is necessary before planning management after failure. A recent meta-analysis reported a 73 % overall response rate (ORR) during azacitidine treatment; however, most azacitidine responses are hematologic improvement (HI) rather than deeper remission (pooled CR rate of only 12 %, partial response (PR) 12 %, and HI 46 %, based on IWG 2000 and 2006 or similar custom response criteria, depending on the specific trial). Similar CR rates but lower ORR are suggested when pooling decitabine MDS trial data: an ORR of 42 % with CR 13 %, PR 5 %, and HI 23 % [15]. The median number of treatment cycles until any IWG qualifying response has been reported to be 2–4 with HMAs, with 75 % of patients who will achieve response to decitabine doing so by cycle 3 and the median time to response with azacitidine about one cycle longer (i.e., 4 cycles). In a few cases, initial responses have been described only after more than 1 year of azacitidine therapy [16].
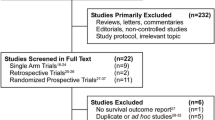
Failure of HMAs can be categorized as “primary” (i.e., no response seen) or “secondary” (i.e., loss of response or disease progression after a period of improvement). A third category of failure occurs if the HMA is stopped before a full course of therapy due to intolerable adverse events, regardless of clinical response. Data on failure patterns and prognosis of such patients comes primarily from two retrospective studies: a multicenter study from Johns Hopkins University and the Groupe Francophone des Myélodysplasies (GFM) and a single-center study from the MD Anderson Cancer Center [17, 18].
Prebet from the GFM and his colleagues retrospectively assessed 435 patients from three clinical trials of azacitidine (J9950, J0443, AZA-001) and the French azacitidine compassionate use program. Twenty percent of patients received combination therapy, most commonly with a histone deacetylase inhibitor (HDACi). Primary failure in this analysis was defined as either IWG-defined progressive or stable disease [4, 18]. Secondary failures included those patients who achieved IWG 2000 qualifying response during azacitidine therapy but then lost response or experienced disease progression. Primary failure, secondary failure, and intolerance were observed in 55 % (n = 229), 36 % (n = 164), and 9 % (n = 42) of patients, respectively. Thirteen of the 42 patients intolerant to azacitidine experienced their adverse effect during a period of response. OS for the cohort was 5.6 months. Predictors of better OS included female gender, younger age, favorable cytogenetics, lower bone marrow blast count before azacitidine treatment, and response to azacitidine.
The best subsequent outcomes in this cohort were in patients who underwent HSCT (median OS 19.5 months), who were likely the group with fewest comorbid conditions and destined to live longer anyway, while those who received only palliative or supportive care did the most poorly (median OS 3 to 4 months). Poor outcomes were also seen with low-dose chemotherapy (e.g., hydroxyurea, mercaptopurine, cytarabine, melphalan) with no patients in this group achieving IWG qualifying response and median OS of 7.3 months. Intensive AML-like chemotherapy was associated with a median OS of 8.9 months, while investigational therapies, which included HDAC inhibitors, thalidomide derivatives, and various nonregistered drugs, did slightly better with median OS of 13.2 months—again, likely due to a selection bias for healthier or younger patients. Similar poor results after azacitidine failure were also demonstrated in a single institution retrospective review of 59 patients, with a median OS of 5.8 months and 12-month survival of 17 % [47].
In an analogous paper, Jabbour and colleagues reviewed outcomes in 87 patients with intermediate- or high-risk MDS or chronic myelomonocytic leukemia (CMML) evaluated at MD Anderson Cancer Center after decitabine failure [17]. In contrast to the study of Prebet et al., patients who discontinued decitabine therapy due to adverse events were not included in this analysis, and IWG 2006 criteria were applied for response [48]. Forty-three percent (n = 37) of the 87 evaluable patients had primary failure while 57 % (n = 50) had secondary failure [17]. The median OS was 4.3 months, with 1-year survival of 28 %. At the time of treatment failure, 25 % had transformed into AML and 75 % had persistent MDS. Among the 65 patients with MDS rather than AML, 10 received idarubicin and cytarabine, with 2 patients achieving decrease in blasts to <5 % (i.e., marrow CR), 30 patients were put on a clinical trial with an ORR of 20 % (most of the trial patient responses were with clofarabine), 4 patients received HSCT with 2 patients achieving a CR lasting over 24 months, 6 patients received unknown therapies, and 15 elected not to receive further treatment beyond supportive care. Comparative survival data were not reported for these subgroups.
Molecular and Clinical Predictors of Hypomethylating Agent Response and Failure
The mechanism of the clinical activity of HMAs in MDS is unclear. Proposed mechanisms include alteration of DNA methylation and, consequently, change in gene expression (either leading to cellular apoptosis or triggering an immunological response) or cytotoxicity akin to other DNA nucleoside analogues such as cytarabine. Aberrant DNA methylation has been described recurrently in MDS, though whether methylation is a pathophysiologic driving mechanism or epiphenomenon remains unclear, and methylation status of specific genes does not predict HMA response [49, 50]. Nonetheless, both clinical and more recently specific molecular genetic markers have been able to predict the likelihood of HMA response with modest success.
Clinical Predictors of Hypomethylating Agent Response
Clinical predictors of HMA response are best described by Itzykson and colleagues in an analysis of 282 IPSS intermediate-2- or high-risk MDS patients from the French compassionate use program [51]. In this series, prior treatment with low-dose cytarabine, bone marrow blasts >15 %, and abnormal karyotype were all associated with decreased HMA response rate. A complex karyotype was associated with a decreased response duration on multivariate analysis. Prognostic factors for decreased OS were Eastern Cooperative Oncology Group performance status (ECOG PS) ≥2, unfavorable IPSS cytogenetic risk, heavy transfusion dependence (defined ≥4 RBC units/8 weeks), and presence of peripheral blasts. Additionally, for patients who failed to achieve CR or PR, achieving HI with erythroid-predominant response predicted a better OS.
A scoring system was developed consisting of these factors and validated using patient data from the AZA-001 trial. Patients could be placed into low-, intermediate-, and high-risk groups with a median OS of not reached, 6.1 months, and 15 months, respectively [52]. This scheme has been validated retrospectively in two smaller cohorts but has not yet undergone prospective validation [53].
Factors that predicted a lower likelihood of achieving response with decitabine in another series were longer duration of MDS and previous MDS therapy [54]. OS was negatively impacted by chromosome 5 or 7 abnormalities, older age, and prior MDS therapy (excluding growth factors). However, a large pooled analysis of 177 patients, mostly from European trials, did not reveal any predictive factors for decitabine response [55]. Predictive factors for OS in decitabine-treated patients in that analysis included an inferior survival in elderly patients (over 75) and those with elevated serum lactate dehydrogenase (LDH), while, surprisingly, high-risk cytogenetics conferred better OS when compared to lower-risk karyotypes. Lastly, response duration was inversely correlated with increasing IPSS risk. Chromosome 5 or 7 abnormalities (specifically isolated monosomy 7) have been linked to a better likelihood or response to decitabine treatment in several studies, but other analyses have not shown a predictive value of chromosome 7 abnormalities [56–58].
Molecular Predictors of Response
Somatic point mutations are detectable in more than 90 % of patients with MDS, and among the ≥40 recurrently mutated genes are several influencing DNA methylation patterns or chromatin conformation, including TET2, DNMT3A, ASXL1, EZH2, and IDH1/IDH2. As a class, this group of “epigenetic” mutations is second in frequency only to those in genes encoding RNA splicing factors (e.g., SF3B1, SRSF2, ZRSR2, U2AF1) [59–61]. There has been wide interest in linking epigenetic abnormalities to specific genetic mutations for therapeutic targets, and several investigative groups have also explored whether mutation results predict HMA response and OS [62••, 63].
TET2 mutations have most consistently been associated with HMA response. TET2 encodes an enzyme that converts 5-methyl-cytosine to 5-hydroxy-methyl-cytosine. A subset of other mutations listed above has been linked to poorer OS and worse prognosis in MDS but has not clearly shown a specific predictive value for HMA response rate, depth, or duration [53].
Recently, Bejar and colleagues published results on 40 sequenced genes in primary cell DNA from 213 MDS patients collected prior to treatment with either azacitidine or decitabine. The cohort demonstrated ORR (41 %) similar to previous HMA trials. A TET2 mutation with at least 10 % allelic burden predicted a higher likelihood of response to HMA (adjusted odds ratio 1.98); this effect was more pronounced if ASXL1 mutations were absent (adjusted odds ratio 3.64). The presence of other mutations (TP53, PTPN11, and others) was associated with shorter OS, but not HMA ORR.
To investigate these results mechanistically, Bejar and colleagues introduced TET2 knockout or wild-type donor marrow into murine recipients, which were then treated either with azacitidine or control. An engraftment advantage in the TET2-null cells over TET2 wild-type cells was observed by chimerism studies [62••]. A previous French study of 86 patients treated with azacitidine supported these findings; investigators observed a higher likelihood of response in TET2-mutated patients (82 % ORR in mutant vs. 45 % for WT) [63]. While TET2 mutation status is likely a reliable marker of response to HMAs, this difference is still not striking enough to influence prescribing patterns.
At this time, no mutation is known to predict lack of response to HMA or impending treatment failure, and no other mutation besides TET2 is known to be related to HMA monotherapy response rate or duration. In a phase 2 study of azacitidine and lenalidomide combination therapy in higher-risk MDS, patients with TET2, DNMT3A, or IDH1/2 mutations appeared to achieve a higher response rate than those without these mutations, although the sample size did not reach statistical significance [34]. Detailed information on the genetic mutations involved in the pathogenesis and influencing prognosis of MDS outside the HMA context is beyond the scope of this article and has been recently reviewed elsewhere [59, 64, 65].
Treatment Options After Hypomethylating Agent Failures
Best Supportive Care
Data from the analysis by Prebet and colleagues described above indicate that patients treated with supportive care alone after HMA have a poor overall prognosis, with a median OS of 4.1 months [18] (Table 1). However, this is the default strategy for patients who are too sick or choose not to receive other therapies.
Low-Dose Cytarabine and Other Cytotoxic Agents
Low-dose cytarabine (LDAC) has modest efficacy in MDS and was the most commonly used cytoreductive agent for MDS patients with excess blasts before HMAs were developed. In a phase III trial conducted in the 1980s by ECOG and the Southwest Oncology Group (SWOG), which evaluated LDAC administered at a dose of 10 mg/m2 twice daily versus best supportive care alone, LDAC was associated with an ORR of 32 % (trial-specific response criteria), but there was no difference in time to leukemic transformation or OS between the two groups [19]. LDAC has not been studied systematically for post-HMA therapy. Although there have been several attempts to use LDAC in combination therapies in higher-risk MDS, these strategies have not yet proven benefit [66, 67].
Intensive AML-like induction chemotherapy for untreated higher-risk MDS is often poorly tolerated, with a high likelihood of early disease recurrence, poor hematopoietic recovery, and treatment-related mortality, despite blast reduction rates of up to 50 % in some series [1, 68, 69]. In the AZA-001 study, while HMA treatment was superior to intensive chemotherapy in higher-risk MDS, only a small number of patients (n = 25) in the control arm chose to receive intensive therapy. To our knowledge, just as for LDAC, there are no studies that prospectively assess the outcomes of intensive therapy after HMA failure, and the Prebet et al. reported relatively poor outcomes in people treated with this approach [18]. One study suggested that in patients with AML arising from MDS in whom azacitidine had failed, cladribine, cytarabine, filgrastim, and mitoxantrone (CLAG-M) were superior to the standard “7 + 3” with cytarabine plus daunorubicin or idarubicin, but this has not been validated in other trials [70].
Switching to Another Hypomethylating Agent or Lenalidomide
A few small retrospective studies have examined the effects of switching to decitabine after azacitidine failure; none has yet reported cohorts of azacitidine after initial loss of response to decitabine therapy (SGI-110, a novel HMA not yet approved by the FDA, is described below). In one analysis of 25 patients with MDS, AML, or MDS/myeloproliferative neoplasms treated with decitabine after primary or secondary azacitidine failure, the results were discouraging, with no patients achieving CR, PR, or HI; five patients achieved stable disease. Median OS was 5.9 months and most patients discontinued decitabine after 1 or 2 cycles [23].
Slightly more favorable results with switching were reported in a 2008 study, where 14 patients for whom azacitidine had failed or not been tolerated were treated with decitabine and the ORR was 28 % (3 CR, 1 HI) [22]. One of the four responding patients had stopped azacitidine for side effects, rather than lack of response. Similarly, investigators at the Moffitt Cancer Center reviewed 21 patients who received decitabine for a median of 4 cycles after azacitidine failure; 19 % of these patients had stopped azacitidine for adverse events, while the rest did not respond. The ORR was 19 % (5 % CR, 14 % HI), but there was a small subgroup within the cohort (n = 10) who restarted azacitidine after discontinuation of decitabine for a drug holiday, and these patients achieved 40 % ORR (20 % CR, 20 % HI) with a median OS of 22 months from azacitidine initiation [21].
Finally, a cohort of ten patients received single-agent lenalidomide for a median of 3 cycles after azacitidine failure. ORR was 40 % (3 CRs, 1 HI), the median response duration was 6 months, and median OS was 20 months. Half of this cohort harbored del(5q) at baseline [71].
Combination Strategies
Addition of a Histone Deacetylase Inhibitor
Understanding of potential gene expression regulation synergy between histone modification and cytosine methylation has prompted clinical interest in HDACi—which also inhibits deacetylation of other cellular proteins—in MDS and other diseases. HCADi that has recently been investigated or is currently undergoing trials in MDS includes entinostat (SNDX275), vorinostat (SAHA), belinostat (PDX101), panobinostat (LBH589), mocetinostat (MGCD0103), and pracinostat (SB939). These agents collectively have had limited activity as single agents in myeloid neoplasms. For instance, belinostat monotherapy induced an ORR of 5 % and was poorly tolerated [27].
Results with HDACi monotherapy in patients for whom HMAs have failed, or adding HDACi to an incompletely effective HMA as an “add-on” strategy, have not been systematically reported. However, up-front combinations of HMA plus HDACi have not shown superiority to HMA alone, suggesting that there may be limited clinical efficacy with this combination approach despite the in vitro synergy.
A randomized phase II comparison of entinostat with entinostat plus azacitidine, E1905, was disappointing, failing to reach the primary objective of improved hematological normalization (monotherapy 32 %, combination therapy 27 %). Adverse events including fatigue and thrombocytopenia, which are HDACi class effects, were more common in the combination arm. Additionally, the combination arm exhibited less treatment-associated demethylation, suggesting an antagonistic effect of entinostat, which is a cell cycle inhibitor (azacitidine requires cells to undergo cycle to have an effect) [29••].
Similarly, the randomized US/Canadian intergroup S1117 trial (NCT01522976) compared azacitidine monotherapy with two combination approaches: azacitidine plus vorinostat, and azacitidine plus lenalidomide, for patients with higher-risk MDS or CMML. The study did not meet its primary endpoint of superior ORR with combination therapy compared to monotherapy, but the combination arms did have longer PFS at the cost of greater toxicity.
Other agents are at an earlier stage of development. Panobinostat was evaluated in a phase Ib/II study assessing 39 patients with AML (n = 29) or MDS (n = 10) in combination with azacitidine, with ORR 50 % in the 10 MDS patients [31]. Pracinostat plus azacitidine combination was associated with a striking 89 % ORR in a small number of patients [30]. Randomized data with pracinostat, however, showed no benefit (http://investor.meipharma.com/2015-03-23-MEI-Pharma-Announces-Top-Line-Data-From-Randomized-Phase-II-Clinical-Study-Of-Pracinostat-In-Front-Line-Myelodysplastic-Syndrome).
Vorinostat was evaluated with decitabine in a phase 1 dose escalation study in 34 patients with relapsed/refractory AML, newly diagnosed AML, or intermediate to HR-MDS; 11 of the patients had MDS. Decitabine was given at 20 mg/m2 for 5 days plus vorinostat 400 mg daily for 14 days. Responses were observed in those who received the drugs in a “concurrent” schedule with 60 % of MDS patients responding in this group (n = 5). Only one patient had dose-limiting toxicity—an individual enrolled in the “sequential” schedule arm [28].
Addition of Lenalidomide
Lenalidomide, the cereblon/ubiquitin ligase modulator that is a standard first-line therapy for lower-risk MDS patients with anemia and deletion of chromosome 5q, has been examined in several studies in combination with HMAs, but not as a post-HMA strategy. In a phase 1 and an extension phase 2 trial conducted by the now-defunct Bone Marrow Failure Consortium, 36 HMA-naïve patients received azacitidine at 75 mg/m2/day and oral lenalidomide 5–10 mg daily in 4-week cycles. Results were encouraging with a median OS of over 37 months, with ORR of 72 %, and with CRR 42 % [33, 34]. However, this combination was not superior to azacitidine monotherapy in the S1117 trial described above. [32].
Clofarabine
Clofarabine, a second-generation nucleoside analog active in AML and MDS, is sometimes used as post-HMA salvage therapy [35, 72]. Clofarabine’s use in the specific population of HMA failures was described in abstract form in 2014 [37]. Fifty-two patients with higher-risk MDS who had received at least 4 cycles of azacitidine or decitabine were given clofarabine 15 mg/m2 IV daily × 5 days in combination with LDAC 20 mg SC twice daily × 7 days, followed by consolidation therapy with the same regimen if an initial response was achieved. An ORR of 48 % was obtained, with a CRR of 17 %, and HI/stable disease of 12 %. Median OS was only 4.8 months, with febrile neutropenia rates of 38 % and 4-week morality of 12 %. Oral clofarabine was tested in 32 MDS patients, 20 of whom had prior failure with an HMA. Using nonstandard response criteria, ORR was reported as 43 % (25 % CR, 9 % HI, 9 % “clinical benefit”). Median OS for the cohort that had received prior HMA therapy was 7.8 months, with 50 % of patients in the entire group experiencing at least one infectious episode [36].
We recently published results from 84 patients with AML (n = 81) and MDS (n = 3) receiving clofarabine either as monotherapy or in combination with cytarabine in the relapsed/refractory setting. The ORR was 21 %, which was lower than previous published studies of clofarabine’s activity in this setting. Median OS was 3 months for the entire cohort, with a small subgroup taken to transplant that had a median OS of 18 months. Unfortunately, the 30-day mortality or induction death rate was equally as high as the response rate at 21 % with 70–80 % experiencing a documented infection or febrile neutropenia, respectively [38]. The ORR for the 30 patients that had previously received HMAs was poor: only 4 patients responded to clofarabine (ORR 17 %); most patients who had received HMAs were given clofarabine alone (n = 19) as opposed to combination therapy with cytarabine.
Hematopoietic Stem Cell Transplant
The topic of HSCT in MDS is complex, with many patient-specific variables to consider, including which patients are suitable transplant candidates, the best timing of transplant in the disease course, the optimal conditioning regimen, and post-HSCT management [73, 74]. Nevertheless, HSCT remains the only possible cure for patients with MDS and should be considered in all potentially transplant-eligible patients after failure of HMAs [13, 75].
Lim and colleagues reviewed 1333 MDS patients undergoing HSCT and observed a 4-year OS of 31 %, with the most important predictor of relapse and nonrelapse mortality being “advanced disease state,” defined as >5 % marrow blasts at the time of conditioning [76]. These and other data showing poorer outcomes in patients going into transplant with excess blasts have argued in favor of pretransplant cytoreduction with HMAs or, if HMAs have already failed, cytotoxic drugs such as clofarabine or induction chemotherapy. Even though patients with MDS without excess blasts have a high clonal burden, this seems to be less of a consideration in transplant outcomes than blast proportion or other disease characteristics such as karyotype. Patients who have been failed by azacitidine can be reassured that should they undergo a transplant; their prognosis is similar to untreated patients undergoing transplant as long as their blast proportion is low, which has been demonstrated in multiple studies [77–79].
Given that most patients with MDS are at least age 70, additional data are needed regarding transplant outcomes and mortality in the elderly population [20]. Comorbid conditions are especially important in transplant decisions in this group, as numerous studies indicate that a higher hematopoietic cell transplant-comorbidity index (HCT-CI) is associated with inferior nonrelapse mortality and survival [24–26].
Most recently, genetic mutations have been shown to influence prognosis after an allogeneic stem cell transplant. Bejar and colleagues reported HSCT outcomes on 87 patients in whom 40 recurrently mutated genes were sequenced by massive parallel sequencing before HSCT. The median age was 58, 71 % of patients underwent reduced intensity conditioning, and prior HMA therapy did not influence results. On univariate analysis, only TP53 mutations conferred a worse median OS and PFS. However, after adjustment of clinical factors associated with these endpoints, TET2 and DNMT3A were additionally associated with poor OS. Three-year OS in patients with one of these mutations was 19 versus 59 % in patients without the mutations [80••]. Furthermore, outcomes with TP53 mutations were particularly grim; all 18 TP53 mutants died before 5 years, with a median OS of 4.6 months, and 83 % had active disease at time of death. It is questionable whether the enormous resource expenditure, risks, and patient lifestyle changes required for transplant are justified in such patients, unless they are part of a clinical trial of a novel approach. Efforts at preventing or aborting relapse with post-HSCT azacitidine and other drugs, donor lymphocyte infusion (DLI), and adaptive immunotherapy vaccines are all being explored [81–85].
Novel Therapeutics
A recent review outlining new developments for MDS highlights the broad range of approaches currently being explored in clinical trials [86]. As new recurrently mutated genes are discovered, yielding additional insight into the pathophysiology of MDS, additional investigational agents targeting these mechanisms will be tested. Below, we highlight several recent developmental programs of special interest for the HMA failure space in MDS.
Rigosertib (ON 01910.Na)
Rigosertib is a multikinase inhibitor with myeloblast-reducing activity in MDS, including in the post-HMA setting [40]. Unfortunately, this agent did not show an OS benefit in a randomized controlled trial versus best supportive care (BSC) in higher-risk MDS patients who had previously been failed by an HMA: OS was 8.2 in the rigosertib arm versus 5.8 months in the BSC arm (not statistically significant) [39•]. Specific subgroups, including primary HMA failures, may have experienced greater benefit with rigosertib [87]. A phase I study evaluating oral rigosertib has been completed. Oral rigosertib demonstrated efficacy in terms of marrow response, hematological improvement, and transfusion independence in a subset of patients, but minor adverse events such as dysuria were common [41].
Sapacitabine
Sapacitabine is a nucleoside analog that generates a small single-stranded break in DNA, which, on subsequent rounds of DNA replication, leads to double-stranded breaks and cell death; additionally, a palmitoyl side chain allows oral absorption and protects the molecule from inactivation. A phase II study of 63 patients with MDS for whom HMAs had failed randomized enrolled subjects to three dose regimens (200 mg BID × 7 days, 300 mg QD × 7 days, or 100 mg QD × 5 days per week for 2 weeks). Responses were seen in 14 % (two CRs, two CRp, and five HI), with 21 patients achieving stable disease lasting longer than 16 weeks; clinical activity was noted in all three schedules. Median OS was 8.6 months with 30-day mortality rate of 5 % in each arm [42].
SGI-110
SGI-110 is a novel dinucleotide HMA that complexes decitabine with deoxyguanosine, inducing resistance to degradation by cytidine deaminase and providing a longer in vivo half-life than decitabine. In a phase I/II study, subcutaneous SGI-110 was administered to 78 patients with AML (n = 64) or MDS (n = 14); phase II schedules included 60 mg/m2/day or 90 mg/m2/day × 5 days. Twenty of 45 patients who were previously treated with HMAs had at least 10 % long interspersed nuclear element demethylation, with over 20 % demethylation in 11/45; more clinical responses (4/11) were seen in the latter group. The ORR, which was not dose-dependent, was 25 %, with eight CRs in 50 relapsed/refractory AML and eight CRs in 17 treatment-naïve AML patients. Febrile neutropenia, thrombocytopenia, anemia, and leukopenia were the most common adverse events and were more frequent with the 90 mg/m2 dose [43••, 44].
AG-221
A primary goal of current cancer genetics efforts is to distinguish biologic subtypes of disease in order to apply more narrowly targeted therapeutics to the subset of patients most likely to benefit. AG-221, an oral, reversible, selective IDH2 inhibitor, which is an exciting new compound with activity in AML, is an example of genotype-directed therapy. In a phase I study, AG-221 was delivered orally at doses ranging from 30 to 100 mg BID in continuous 28-day cycles to 18 AML patients and 1 MDS patient harboring an IDH2 mutation. Pharmacodynamic studies showed sustained reduction in levels of the oncometabolite generated by IDH1 or IDH2 mutations, 2-hydroxyglutarate. At the time of release of preliminary data, ten AML patients were evaluable for response and six had objective responses, including two CRs. There were no dose-limiting toxicities reported, but severe adverse events included hyperleukocytosis, confusion, and death from sepsis [45••]. An inhibitor of IDH1 is in an earlier phase of development.
ARRY-614
ARRY-614 is a dual inhibitor of both p38 and Tie2 kinases that has showed activity in a phase 1 trial enrolling patients with MDS who met criteria for IPSS low- or intermediate-1-risk disease (although the IPSS was meant to apply only at diagnosis and not subsequent in the disease course). Sixty-two patients were treated at escalating doses for a median of 13 weeks, and the most common treatment-related adverse events were rash, nausea, atrial fibrillation, decreased appetite, fatigue, and vomiting. The rate of HI was 22 % (12/54) across all cell lines, and several patients achieved platelet transfusion independence. Curiously, all of the responding patients had been treated with a HMA [46•].
Other Agents
Several kinase inhibitors approved for other malignancies, such as erlotinib and dasatinib, have been studied in MDS populations including patients for whom HMAs failed but had limited efficacy [88, 89]. An oral formulation of azacitidine (CC-486) has activity in both untreated and previously treated patients with MDS; diarrhea and febrile neutropenia were observed in up to 20 % [90]. Further studies with CC-486 are underway. Newer drugs such as INCB024360, an oral inhibitor of indoleamine 2,3-dioxygenase, and birinapant, a second mitochondrial activator of caspases (SMAC) peptidomimetic, are in early stages of investigation (NCT01822691 and NCT01828346).
Conclusion
Although HMAs have improved MDS care, the high failure rate and uncertainty about how to best proceed once an HMA has failed the patient remain major challenges. For now, patients for whom HSCT remains a feasible option should be offered transplantation, but it is unclear how to proceed with other patients. Improved understanding of the molecular pathophysiology underlying MDS may eventually yield novel targeted agents that will move treatment forward.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Greenberg PL, Attar E, Bennett JM, Bloomfield CD, Borate U, De Castro CM, et al. Myelodysplastic syndromes: clinical practice guidelines in oncology. J Natl Compr Cancer Netw: JNCCN. 2013;11(7):838–74.
Runde V, de Witte T, Arnold R, Gratwohl A, Hermans J, van Biezen A, et al. Bone marrow transplantation from HLA-identical siblings as first-line treatment in patients with myelodysplastic syndromes: early transplantation is associated with improved outcome. Chronic Leukemia working party of the European Group for blood and marrow transplantation. Bone Marrow Transplant. 1998;21(3):255–61. doi:10.1038/sj.bmt.1701084.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009;10(3):223–32. doi:10.1016/s1470-2045(09)70003-8.
Cheson BD, Bennett JM, Kantarjian H, Pinto A, Schiffer CA, Nimer SD, et al. Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood. 2000;96(12):3671–4.
Kantarjian H, Issa JP, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106(8):1794–803. doi:10.1002/cncr.21792.
Lubbert M, Suciu S, Baila L, Ruter BH, Platzbecker U, Giagounidis A, et al. Low-dose decitabine versus best supportive care in elderly patients with intermediate- or high-risk myelodysplastic syndrome (MDS) ineligible for intensive chemotherapy: final results of the randomized phase III study of the European Organisation for Research and Treatment of Cancer Leukemia Group and the German MDS Study Group. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29(15):1987–96. doi:10.1200/jco.2010.30.9245.
Steensma DP, Baer MR, Slack JL, Buckstein R, Godley LA, Garcia-Manero G, et al. Multicenter study of decitabine administered daily for 5 days every 4 weeks to adults with myelodysplastic syndromes: the alternative dosing for outpatient treatment (ADOPT) trial. J Clin Oncol: Off J Am Soc Clin Oncol. 2009;27(23):3842–8. doi:10.1200/jco.2008.19.6550.
Lee JH, Jang JH, Park J, Park S, Joo YD, Kim YK, et al. A prospective multicenter observational study of decitabine treatment in Korean patients with myelodysplastic syndrome. Haematologica. 2011;96(10):1441–7. doi:10.3324/haematol.2011.046078.
Oki Y, Kondo Y, Yamamoto K, Ogura M, Kasai M, Kobayashi Y, et al. Phase I/II study of decitabine in patients with myelodysplastic syndrome: a multi-center study in Japan. Cancer Sci. 2012;103(10):1839–47. doi:10.1111/j.1349-7006.2012.02386.x.
Wijermans P, Lubbert M, Verhoef G, Bosly A, Ravoet C, Andre M, et al. Low-dose 5-aza-2′-deoxycytidine, a DNA hypomethylating agent, for the treatment of high-risk myelodysplastic syndrome: a multicenter phase II study in elderly patients. J Clin Oncol: Off J Am Soc Clin Oncol. 2000;18(5):956–62.
Gergis U, Wissa U. High-risk myelodysplastic syndromes: chemotherapy, transplantation, and beyond. Curr Hematol Malig Rep. 2010;5(1):1–8. doi:10.1007/s11899-009-0035-0.
Sekeres MA, Cutler C. How we treat higher-risk myelodysplastic syndromes. Blood. 2014;123(6):829–36. doi:10.1182/blood-2013-08-496935.
Zeidan AM, Linhares Y, Gore SD. Current therapy of myelodysplastic syndromes. Blood Rev. 2013;27(5):243–59. doi:10.1016/j.blre.2013.07.003.
Steensma DP. Can hypomethylating agents provide a platform for curative therapy in myelodysplastic syndromes? Best Pract Res Clin Haematol. 2012;25(4):443–51. doi:10.1016/j.beha.2012.10.007.
Xie M, Jiang Q, Xie Y. Comparison between decitabine and azacitidine for the treatment of myelodysplastic syndrome: a meta-analysis with 1392 participants. Clin Lymphoma Myeloma Leuk. 2014. doi:10.1016/j.clml.2014.04.010.
Silverman LR, McKenzie DR, Peterson BL, Holland JF, Backstrom JT, Beach CL, et al. Further analysis of trials with azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921, and 9221 by the Cancer and Leukemia Group B. J Clin Oncol: Off J Am Soc Clin Oncol. 2006;24(24):3895–903. doi:10.1200/jco.2005.05.4346.
Jabbour E, Garcia-Manero G, Batty N, Shan J, O’Brien S, Cortes J, et al. Outcome of patients with myelodysplastic syndrome after failure of decitabine therapy. Cancer. 2010;116(16):3830–4. doi:10.1002/cncr.25247.
Prebet T, Gore SD, Esterni B, Gardin C, Itzykson R, Thepot S, et al. Outcome of high-risk myelodysplastic syndrome after azacitidine treatment failure. J Clin Oncol: Off J Am Soc Clin Oncol. 2011;29(24):3322–7. doi:10.1200/jco.2011.35.8135.
Miller KB, Kim K, Morrison FS, Winter JN, Bennett JM, Neiman RS, et al. The evaluation of low-dose cytarabine in the treatment of myelodysplastic syndromes: a phase-III intergroup study. Ann Hematol. 1992;65(4):162–8.
Sekeres MA. Epidemiology, natural history, and practice patterns of patients with myelodysplastic syndromes in 2010. J Natl Compr Cancer Netw: JNCCN. 2011;9(1):57–63.
Apuri S, Lancet JE, Ali NHA, Padron E, Ho VQ, Pinilla-Ibarz J, et al. Evidence for selective benefit of sequential treatment with azanucleosides in patients with myelodysplastic syndromes (MDS). ASH Ann Meet Abstr. 2012;120(21):4937.
Borthakur G, Ahdab SE, Ravandi F, Faderl S, Ferrajoli A, Newman B, et al. Activity of decitabine in patients with myelodysplastic syndrome previously treated with azacitidine. Leuk Lymphoma. 2008;49(4):690–5. doi:10.1080/10428190701882146.
Duong VH, Bhatnagar B, Zandberg DP, Vannorsdall EJ, Tidwell ML, Chen Q et al. Lack of objective response of myelodysplastic syndromes and acute myeloid leukemia to decitabine after failure of azacitidine. Leukemia & lymphoma. 2014:1–22. doi:10.3109/10428194.2014.966708
Boehm A, Sperr WR, Leitner G, Worel N, Oehler L, Jaeger E, et al. Comorbidity predicts survival in myelodysplastic syndromes or secondary acute myeloid leukaemia after allogeneic stem cell transplantation. Eur J Clin Investig. 2008;38(12):945–52. doi:10.1111/j.1365-2362.2008.02041.x.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912–9. doi:10.1182/blood-2005-05-2004.
Sorror ML, Sandmaier BM, Storer BE, Maris MB, Baron F, Maloney DG, et al. Comorbidity and disease status based risk stratification of outcomes among patients with acute myeloid leukemia or myelodysplasia receiving allogeneic hematopoietic cell transplantation. J Clin Oncol: Off J Am Soc Clin Oncol. 2007;25(27):4246–54. doi:10.1200/jco.2006.09.7865.
Cashen A, Juckett M, Jumonville A, Litzow M, Flynn PJ, Eckardt J, et al. Phase II study of the histone deacetylase inhibitor belinostat (PXD101) for the treatment of myelodysplastic syndrome (MDS). Ann Hematol. 2012;91(1):33–8. doi:10.1007/s00277-011-1240-1.
Kirschbaum M, Gojo I, Goldberg SL, Bredeson C, Kujawski LA, Yang A, et al. A phase 1 clinical trial of vorinostat in combination with decitabine in patients with acute myeloid leukaemia or myelodysplastic syndrome. Br J Haematol. 2014. doi:10.1111/bjh.13016.
Prebet T, Sun Z, Figueroa ME, Ketterling R, Melnick A, Greenberg PL, et al. Prolonged administration of azacitidine with or without entinostat for myelodysplastic syndrome and acute myeloid leukemia with myelodysplasia-related changes: results of the US Leukemia Intergroup trial E1905. J Clin Oncol: Off J Am Soc Clin Oncol. 2014;32(12):1242–8. doi:10.1200/jco.2013.50.3102. This study showed disappointing results with the HDACI entinostat, which should caution practitioners to use this class of therapy in combination with azacitidine.
Quintas-Cardama AKH, Ravandi F, Foudray C, Pemmaraju N, Kadia TM, et al. Very high rates of clinical and cytogenetic response with the combination of the histone deacetylase inhibitor pracinostat (SB939) and 5-azacitidine in high-risk myelodysplastic syndrome. Blood (ASH Ann Meet Abstr). 2012;120:3821.
Tan P, Wei A, Mithraprabhu S, Cummings N, Liu HB, Perugini M, et al. Dual epigenetic targeting with panobinostat and azacitidine in acute myeloid leukemia and high-risk myelodysplastic syndrome. Blood Cancer J. 2014;4:e170. doi:10.1038/bcj.2013.68.
Finelli C CC, Follo MY, Stanzani M, Avanzini P, Bosi C, Castagnari B et al. Addition of lenalidomide (LEN) to azacitidine (AZA) (combined vs sequential treatment) in high-risk myelodysplastic syndromes (MDS): a randomized phase II multicenter study. Blood Abstract 4648 ASH 2014 Annual Meeting. 2014.
Sekeres MA, List AF, Cuthbertson D, Paquette R, Ganetzky R, Latham D, et al. Phase I combination trial of lenalidomide and azacitidine in patients with higher-risk myelodysplastic syndromes. J Clin Oncol: Off J Am Soc Clin Oncol. 2010;28(13):2253–8. doi:10.1200/jco.2009.26.0745.
Sekeres MA, Tiu RV, Komrokji R, Lancet J, Advani AS, Afable M, et al. Phase 2 study of the lenalidomide and azacitidine combination in patients with higher-risk myelodysplastic syndromes. Blood. 2012;120(25):4945–51. doi:10.1182/blood-2012-06-434639.
Bryan J, Kantarjian H, Prescott H, Jabbour E. Clofarabine in the treatment of myelodysplastic syndromes. Expert Opin Invest Drugs. 2014;23(2):255–63. doi:10.1517/13543784.2014.877887.
Faderl S, Garcia-Manero G, Estrov Z, Ravandi F, Borthakur G, Cortes JE, et al. Oral clofarabine in the treatment of patients with higher-risk myelodysplastic syndrome. J Clin Oncol: Off J Am Soc Clin Oncol. 2010;28(16):2755–60. doi:10.1200/jco.2009.26.3509.
Jabbour E SK, Daver N, Pemmaraju N, Jain N, Kadia TP, DiNardo CD et al. Clofarabine plus low-dose cytarabine for the treatment of patients with higher-risk myelodysplastic syndromes (MDS) who have relapsed or are refractory to hypomethylating agent (HMA) therapy. Blood Abstract 534 ASH 2014 Annual Meeting. 2014.
Roberts DA, Wadleigh M, McDonnell AM, DeAngelo DJ, Stone RM, Steensma DP. Low efficacy and high mortality associated with clofarabine treatment of relapsed/refractory acute myeloid leukemia and myelodysplastic syndromes. Leuk Res. 2014. doi:10.1016/j.leukres.2014.11.031.
Garcia-Manero G FP, Al-Kali A, et al. Randomized phase 3 study of intravenous rigosertib vs best supportive care (B) in higher-risk myelodysplastic syndrome (HR-MDS) patients (pts) after hypomethylating agent (HMA) failure—topline results. Journal of Clinical Oncology (ASCO Annual Meeting Abstracts), 2014 Abstract LBA:. 2014. These results showed that overall survival was not significantly affected by rigosertib in this large, phase III randomized trial in patients after HMA failure .
Raza AGP, Olnes MJ, Silverman LR, Wilhelm F. Final phase I/II results of rigosertib (ON 01910.Na) hematological effects in patients with myelodysplastic syndrome and correlation with overall survival. Blood (ASH Ann Meet Abstr). 2011;118:3822.
Komrokji RS, Raza A, Lancet JE, Ren C, Taft D, Maniar M, et al. Phase I clinical trial of oral rigosertib in patients with myelodysplastic syndromes. Br J Haematol. 2013;162(4):517–24. doi:10.1111/bjh.12436.
Garcia-Manero G LS, Goldberg S, Altman JK, Arellano M, Wetzler M, Seiter K et al. A randomized phase II study of sapacitabine In MDS refractory to hypomethylating agents Blood Abstract 2752 ASH 2013 Annual Meeting. 2013.
Kantarjian HM EJ YK, Kropf P, O’Connell C, Stock W, Tibes R, Rizzieri D, et al. First clinical results of a randomized phase 2 study of SGI-110, a novel subcutaneous (SQ) hypomethylating agent (HMA), in adult patients with acute myeloid leukemia (AML). Blood. 2013;122(21):497. These are the first results showing that an alternative hypomethylating agent has efficacy in MDS and AML (the phase 1 component included MDS patients).
Kantarjian HM RG, Rizzieri DA, Stock W, O’Connell CL, Griffiths EA, Yee K et al. Results from the dose escalation phase of a randomized phase 1-2 First-in-Human (FIH) Study of SGI-110, a novel low volume stable subcutaneous (SQ) second generation hypomethylating agent (HMA) in patients with relapsed/refractory MDS and AML Blood Annual Meeting Abstracts. 2012.
Eytan Stein MT, Daniel A. Pollyea, Ian W. Flinn, Amir T. Fathi, Richard M. Stone, Ross L. Levine, Samuel Agresta, David Schenkein, Hua Yang, Bin Fan, Kate Yen, Stephane De Botton. Clinical safety and activity in a phase I trial of AG-221, a first in class, potent inhibitor of the IDH2-mutant protein, in patients with IDH2 mutant positive advanced hematologic malignancies Proceedings of the 105th Annual Meeting of the American Association for Cancer Research; 2014 Apr 5-9; San Diego, CA Philadelphia (PA): AACR; 2014 Abstract CT103 The first data showing that a therapy targeted at a mutation involved in the epigenetic pathophysiology of MDS has clinical efficacy.
Garcia-Manero G SM, List AF, Khoury HJ, Advani A, Jabbour E, Kantarjian HM et al. Phase I dose-escalation/expansion study of ARRY-614 in patients with IPSS low/Int-1 risk myelodysplastic syndromes. Blood 2013 ASH Annual Meeting Abstract 387. This data showed that ARRY-614, a dual inhibitor of p38 and Tie2, has clinical efficacy in low- to intermediate-1-risk MDS.
Duong VH, Lin K, Reljic T, Kumar A, Al Ali NH, Lancet JE, et al. Poor outcome of patients with myelodysplastic syndrome after azacitidine treatment failure. Clin Lymphoma Myeloma Leuk. 2013;13(6):711–5. doi:10.1016/j.clml.2013.07.007.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108(2):419–25. doi:10.1182/blood-2005-10-4149.
Figueroa ME, Skrabanek L, Li Y, Jiemjit A, Fandy TE, Paietta E, et al. MDS and secondary AML display unique patterns and abundance of aberrant DNA methylation. Blood. 2009;114(16):3448–58. doi:10.1182/blood-2009-01-200519.
Jiang Y, Dunbar A, Gondek LP, Mohan S, Rataul M, O’Keefe C, et al. Aberrant DNA methylation is a dominant mechanism in MDS progression to AML. Blood. 2009;113(6):1315–25. doi:10.1182/blood-2008-06-163246.
Itzykson R, Thepot S, Quesnel B, Dreyfus F, Beyne-Rauzy O, Turlure P, et al. Prognostic factors for response and overall survival in 282 patients with higher-risk myelodysplastic syndromes treated with azacitidine. Blood. 2011;117(2):403–11. doi:10.1182/blood-2010-06-289280.
Itzykson R, Thepot S, Quesnel B, Dreyfus F, Recher C, Wattel E, et al. Long-term outcome of higher-risk MDS patients treated with azacitidine: an update of the GFM compassionate program cohort. Blood. 2012;119(25):6172–3. doi:10.1182/blood-2012-04-422204.
Zeidan AM, Komrokji RS. There’s risk, and then there’s risk: the latest clinical prognostic risk stratification models in myelodysplastic syndromes. Curr hematol Malig Rep. 2013;8(4):351–60. doi:10.1007/s11899-013-0172-3.
Kantarjian HM, O’Brien S, Shan J, Aribi A, Garcia-Manero G, Jabbour E, et al. Update of the decitabine experience in higher risk myelodysplastic syndrome and analysis of prognostic factors associated with outcome. Cancer. 2007;109(2):265–73. doi:10.1002/cncr.22376.
Wijermans PW, Lubbert M, Verhoef G, Klimek V, Bosly A. An epigenetic approach to the treatment of advanced MDS; the experience with the DNA demethylating agent 5-aza-2′-deoxycytidine (decitabine) in 177 patients. Ann Hematol. 2005;84 Suppl 1:9–17. doi:10.1007/s00277-005-0012-1.
Raj K, John A, Ho A, Chronis C, Khan S, Samuel J, et al. CDKN2B methylation status and isolated chromosome 7 abnormalities predict responses to treatment with 5-azacytidine. Leukemia. 2007;21(9):1937–44. doi:10.1038/sj.leu.2404796.
Ravandi F, Issa JP, Garcia-Manero G, O’Brien S, Pierce S, Shan J, et al. Superior outcome with hypomethylating therapy in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome and chromosome 5 and 7 abnormalities. Cancer. 2009;115(24):5746–51. doi:10.1002/cncr.24661.
Ruter B, Wijermans P, Claus R, Kunzmann R, Lubbert M. Preferential cytogenetic response to continuous intravenous low-dose decitabine (DAC) administration in myelodysplastic syndrome with monosomy 7. Blood. 2007;110(3):1080–2. doi:10.1182/blood-2007-03-080630. author reply 3.
Abdel-Wahab O, Figueroa ME. Interpreting new molecular genetics in myelodysplastic syndromes. Hematol Educ Program Am Soc Hematol Am Soc Hematol Educ Prog. 2012;2012:56–64. doi:10.1182/asheducation-2012.1.56.
Haferlach T, Nagata Y, Grossmann V, Okuno Y, Bacher U, Nagae G, et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28(2):241–7. doi:10.1038/leu.2013.336.
Itzykson R, Kosmider O, Fenaux P. Somatic mutations and epigenetic abnormalities in myelodysplastic syndromes. Best Pract Res Clin Haematol. 2013;26(4):355–64. doi:10.1016/j.beha.2014.01.001.
Bejar R, Lord A, Stevenson K, Bar-Natan M, Perez-Ladaga A, Zaneveld J, et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood. 2014. doi:10.1182/blood-2014-06-582809. This study shows TET2 mutational status as a strong association with response patterns to hypomethylating agents.
Itzykson R, Kosmider O, Cluzeau T, Mansat-De Mas V, Dreyfus F, Beyne-Rauzy O, et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia. 2011;25(7):1147–52. doi:10.1038/leu.2011.71.
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364(26):2496–506. doi:10.1056/NEJMoa1013343.
Vigna E, Recchia AG, Madeo A, Gentile M, Bossio S, Mazzone C, et al. Epigenetic regulation in myelodysplastic syndromes: implications for therapy. Expert Opin Invest Drugs. 2011;20(4):465–93. doi:10.1517/13543784.2011.559164.
Macdonald DA, Assouline SE, Brandwein J, Kamel-Reid S, Eisenhauer EA, Couban S, et al. A phase I/II study of sorafenib in combination with low dose cytarabine in elderly patients with acute myeloid leukemia or high-risk myelodysplastic syndrome from the National Cancer Institute of Canada Clinical Trials Group: trial IND.186. Leuk Lymphoma. 2013;54(4):760–6. doi:10.3109/10428194.2012.737917.
Prebet T, Braun T, Beyne-Rauzy O, Dreyfus F, Stammatoullas A, Wattel E, et al. Combination of vorinostat and low dose cytarabine for patients with azacitidine-refractory/relapsed high risk myelodysplastic syndromes. Leuk Res. 2014;38(1):29–33. doi:10.1016/j.leukres.2013.07.023.
Knipp S, Hildebrand B, Kundgen A, Giagounidis A, Kobbe G, Haas R, et al. Intensive chemotherapy is not recommended for patients aged >60 years who have myelodysplastic syndromes or acute myeloid leukemia with high-risk karyotypes. Cancer. 2007;110(2):345–52. doi:10.1002/cncr.22779.
Pollyea DA, Gutman JA. Stopping higher-risk myelodysplastic syndrome in its tracks. Curr Hematol Malig Rep. 2014. doi:10.1007/s11899-014-0234-1.
Jaglal MV, Duong VH, Bello CM, Al Ali NH, Padron E, Fernandez HF, et al. Cladribine, cytarabine, filgrastim, and mitoxantrone (CLAG-M) compared to standard induction in acute myeloid leukemia from myelodysplastic syndrome after azanucleoside failure. Leuk Res. 2014;38(4):443–6. doi:10.1016/j.leukres.2013.12.010.
Prebet T, Charbonnier A, Gelsi-Boyer V, Mozziconacci MJ, Blaise D, Vey N. Lenalidomide treatment for patients with myelodysplastic syndrome and low blast count acute myeloid leukemia after azacitidine failure. Leuk Lymphoma. 2013;54(7):1538–40. doi:10.3109/10428194.2012.744455.
Ghanem H, Kantarjian H, Ohanian M, Jabbour E. The role of clofarabine in acute myeloid leukemia. Leuk Lymphoma. 2013;54(4):688–98. doi:10.3109/10428194.2012.726722.
Bart-Smith E, Mufti GJ. Allogeneic haematopoietic stem cell transplantation in myelodysplastic syndromes. Curr Opin Oncol. 2014;26(6):642–9. doi:10.1097/cco.0000000000000137.
Zeidan AM, Kharfan-Dabaja MA, Komrokji RS. Beyond hypomethylating agents failure in patients with myelodysplastic syndromes. Curr Opin Hematol. 2014;21(2):123–30. doi:10.1097/moh.0000000000000016.
Kadia TM, Jabbour E, Kantarjian H. Failure of hypomethylating agent-based therapy in myelodysplastic syndromes. Semin Oncol. 2011;38(5):682–92. doi:10.1053/j.seminoncol.2011.04.011.
Lim Z, Brand R, Martino R, van Biezen A, Finke J, Bacigalupo A, et al. Allogeneic hematopoietic stem-cell transplantation for patients 50 years or older with myelodysplastic syndromes or secondary acute myeloid leukemia. J Clin Oncol: Off J Am Soc Clin Oncol. 2010;28(3):405–11. doi:10.1200/jco.2009.21.8073.
Damaj G, Duhamel A, Robin M, Beguin Y, Michallet M, Mohty M, et al. Impact of azacitidine before allogeneic stem-cell transplantation for myelodysplastic syndromes: a study by the Societe Francaise de Greffe de Moelle et de Therapie-Cellulaire and the Groupe-Francophone des Myelodysplasies. J Clin Oncol: Off J Am Soc Clin Oncol. 2012;30(36):4533–40. doi:10.1200/jco.2012.44.3499.
Field T, Perkins J, Huang Y, Kharfan-Dabaja MA, Alsina M, Ayala E, et al. 5-Azacitidine for myelodysplasia before allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2010;45(2):255–60. doi:10.1038/bmt.2009.134.
Gerds AT, Gooley TA, Estey EH, Appelbaum FR, Deeg HJ, Scott BL. Pretransplantation therapy with azacitidine vs induction chemotherapy and posttransplantation outcome in patients with MDS. Biology Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2012;18(8):1211–8. doi:10.1016/j.bbmt.2012.01.009.
Bejar R, Stevenson KE, Caughey B, Lindsley RC, Mar BG, Stojanov P, et al. Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem-cell transplantation. J Clin Oncol: Off J Am Soc Clin Oncol. 2014;32(25):2691–8. doi:10.1200/jco.2013.52.3381. This is the first paper to demonstrate a prognostic significance of genetic mutations after hematopoietic stem cell transplantation.
de Lima M, Giralt S, Thall PF, de Padua SL, Jones RB, Komanduri K, et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer. 2010;116(23):5420–31. doi:10.1002/cncr.25500.
Ho VT, Vanneman M, Kim H, Sasada T, Kang YJ, Pasek M, et al. Biologic activity of irradiated, autologous, GM-CSF-secreting leukemia cell vaccines early after allogeneic stem cell transplantation. Proc Natl Acad Sci U S A. 2009;106(37):15825–30. doi:10.1073/pnas.0908358106.
Krishnamurthy P, Potter VT, Barber LD, Kulasekararaj AG, Lim ZY, Pearce RM, et al. Outcome of donor lymphocyte infusion after T cell-depleted allogeneic hematopoietic stem cell transplantation for acute myelogenous leukemia and myelodysplastic syndromes. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2013;19(4):562–8. doi:10.1016/j.bbmt.2012.12.013.
Marks DI, Lush R, Cavenagh J, Milligan DW, Schey S, Parker A, et al. The toxicity and efficacy of donor lymphocyte infusions given after reduced-intensity conditioning allogeneic stem cell transplantation. Blood. 2002;100(9):3108–14. doi:10.1182/blood-2002-02-0506.
Platzbecker U, Wermke M, Radke J, Oelschlaegel U, Seltmann F, Kiani A, et al. Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: results of the RELAZA trial. Leukemia. 2012;26(3):381–9. doi:10.1038/leu.2011.234.
Bejar R, Steensma DP. Recent developments in myelodysplastic syndromes. Blood. 2014. doi:10.1182/blood-2014-04-522136.
Garcia-Manero G FP, Al-Kali A, Baer MR, Sekeres MA, Roboz GJ, Gaidano G et al. Overall survival and subgroup analysis from a randomized phase III study of intravenous rigosertib versus best supportive care (BSC) in patients (pts) with higher-risk myelodysplastic syndrome (HR-MDS) after failure of hypomethylating agents (HMAs). Blood Abstract 163 ASH 2014 Annual Meeting. 2014.
Duong VH, Jaglal MV, Zhang L, Kale V, Lancet JE, Komrokji RS, et al. Phase II pilot study of oral dasatinib in patients with higher-risk myelodysplastic syndrome (MDS) who failed conventional therapy. Leuk Res. 2013;37(3):300–4. doi:10.1016/j.leukres.2012.11.001.
Komrokji RS, Padron E, Yu D, Fulp WJ, Rodriguez Y, Tinsley S, et al. Phase II clinical study of erlotinib for treatment of myelodysplastic syndromes. Am J Hematol. 2014;89(8):809–12. doi:10.1002/ajh.23749.
Garcia-Manero G, Gore SD, Cogle C, Ward R, Shi T, Macbeth KJ, et al. Phase I study of oral azacitidine in myelodysplastic syndromes, chronic myelomonocytic leukemia, and acute myeloid leukemia. J Clin Oncol: Off J Am Soc Clin Oncol. 2011;29(18):2521–7. doi:10.1200/jco.2010.34.4226.
Compliance with Ethics Guidelines
Conflict of Interest
Daniel A. Roberts declares no potential conflicts of interest.
David P. Steensma is a section editor for Current Hematologic Malignancy Reports. He has served as a consultant to Onconova, Novartis, and MEI Pharma.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Funding Source
None
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Myelodysplastic Syndromes
Rights and permissions
About this article
Cite this article
Roberts, D.A., Steensma, D.P. Outlook and Management of Patients with Myelodysplastic Syndromes Failed by Hypomethylating Agents. Curr Hematol Malig Rep 10, 318–328 (2015). https://doi.org/10.1007/s11899-015-0273-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-015-0273-2