Abstract
Purpose
The study highlights azygos vein (AV) topography, arrangement and confluence morphometry in dyspnoea and tachycardia patients of extrapulmonary and extracardiac aetiology.
Method
Computed-tomography angiography of 25 male and 26 female patients (mean age 66.5 years) were studied for: thoracic vertebral (T) height of AV- superior vena cava-SVC confluence, AV course and deviations from vertebral column (VC) midline, AV and SVC diameters, distance (AV arch- lower border of carina) and gender and age impact.
Results
Commonest heights of the AV-SVC confluence were T5 (56.9%), T4 (31.4%), T6 (9.8%) and T3 (2%). The AV terminated into SVC after crossing the left side of VC midline in 56.9%, slightly deviated right of the midline in 37.3% and coursed right of VC in 5.9%. Mean AV and SVC diameters were 0.96 ± 0.18 cm and 1.86 ± 0.27 cm. Male predominance in AV and SVC diameters and a slight AV diameter significant increase with the age were found. The (AV highest point—lower border of carina) mean distance was 2.05 ± 0.44 cm and male predominance existed.
Conclusion
The commonest termination height of the AV was T5, while T3 was the rarest one. Aging induces the AV leftward displacement, while gender had no impact. AV and SVC diameters had higher significant values in males, while ageing had a significant impact only in AV diameter. The AV higher diameters will be used as predictors for higher values of SVC diameter and mediastinum pathology. Such findings can be useful in mediastinal surgery, mediastinoscopy and surgery of VC deformations, neurovascular surgery of retroperitoneal organs, disc herniation and T fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The azygos vein (AV) typically ascends posterior mediastinum along thoracic vertebrae (T) anterolateral surface, after coursing through the diaphragm and terminates at T4, arching anteriorly (the so-called AV arch) to superior vena cava (SVC) [30], close to the 2nd costal cartilage (± 16.3 mm rightward) of vertebral column (VC) midline [21]. Rarely, the AV drains into the right brachiocephalic vein, the right subclavian vein, the intrapericardial SVC and the right atrium [5, 8]. The AV via its imperfect valves allows bi-directional collateral circulation, functioning as an alternative heart pathway, in cases of SVC thrombosis. Communication with vertebral venous plexuses also assists in collateral circulation [35]. The AV may also act as a metastatic pathway to the lungs. Moreover, it contributes to delineating the anatomical contours of the right paratracheal space and azygo-oesophageal recess [25].
The AV displays a high topographic and morphological variability and particularly its deviation warrants further systematic investigation in larger cadaveric and imaging samples.
Modern imaging modalities (computed tomography angiography-CTA and magnetic resonance imaging- MRI) help the accurate depiction and in a deep understanding of thoracic regional anatomy and particularly vessels’ morphology [5]. CTA is considered the gold standard for pulmonary embolism diagnosis [37] and could be used as an alternative tool instead of cadavers’ dissection to investigate thoracic vessels’ anatomy.
The current study highlights AVs topography and arrangement, as well as AV-SVC confluence morphometry by using chest CTAs of male and female patients of different ages (1st age group, 18–52 years) and (2nd, 53 years and above) with dyspnoea and tachycardia symptoms of extrapulmonary and extracardiac aetiology. T projection height of the AV drainage into SVC (veins confluence) was recorded scanning T to the upper, middle and lower thirds. The AV course was recorded in relation to VC midline and emphasis was given to leftward and rightward deviations. AV and SVC diameters, as well as T height, in which AV joins SVC and the (AV arch-carina) distance, were measured. Gender and age impact were further investigated and discussed.
Material and methods
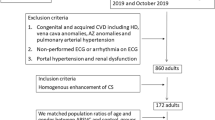
Thoracic CTAs of 51 (25 male of mean age 67.8 and 26 female of mean age 65.35 years) Greek patients were investigated, between September 2018 and April 2019. Patients gave a written informed consent for retrospective data analysis in accordance to Helsinki Declaration. Patients’ sample (mean age 66.5 ± 17.2 years) was divided into 2 age groups: 1) 18–52 years (9 patients) and 2) 53 years and above (42 patients) to better examine age impact on measured parameters. Ethics Committees of the Aristotle University and the General Hospital “G. Gennimatas” of Thessaloniki waived ethical approval. CTA images were acquired with a Toshiba Aquilion CXL CT scanner (128-slice). Imaging was obtained before and after a bolus injection of 120 mL (4–5 mL/s) of non-ionic contrast material (Iopromide, Ultravist 300, Bayer Schering Pharma, Berlin, Germany) in arterial and portal phases with 5 mm slice thickness, a pitch 2, 3 mm reconstruction interval and 1 s scan time. All measurements were performed by using the Radiant Dicom Viewer software after multiplanar reconstruction in coronal, axial, sagittal and oblique views. To accurately determine the exact T level of the AV-SVC confluence projection; vertebrae were divided into upper, middle and lower thirds. Each T covered the distance from the middle of the superior until the middle of the inferior intervertebral disks. The AV course was recorded in relation to VC midline (right of VC midline, VC midline, crossing to the left side of the midline and back to the right side into SVC termination). The AV and SVC diameters at the AV-SVC confluence (Fig. 1) and the distance (highest point of AV arch—lower margin of carina) were also calculated (Fig. 2).
Inclusion criteria
51 out of 103 (49.51%) CTAs of patients, who have visited the Emergency Department with dyspnoea and tachycardia symptoms due to extrapulmonary and extracardiac conditions without alterations of mediastinal structures topography, were included. Only mental and thyroid disorders, anxiety and anemia cases constituted our sample.
Exclusion criteria
52 CTAs with pathological signs (congestive heart failure, acute coronary syndrome, pneumonia, chronic obstructive pulmonary disease and pulmonary embolism), alterations in mediastinal anatomy (tumors or previous surgery), technical errors, severe artifacts, inadequate vascular enhancement or incomplete datasets and cases with lack of signed consent from patients.
Statistical analysis was performed using IBM SPSS statistical package (version 22). Descriptive statistics are displayed as mean ± standard deviation (SD) for continuous variables and number (%) for categorical variables.Distributions’ normality was checked using the Kolmogorov–Smirnov test (observations ≥ 50). In cases of variables that did not follow the normal distribution, non-parametric tests were used. Gender dimorphism was investigated with Independent Sample T test and Mann–Whitney U test and age impact with Kruskal–Wallis and one-way ANOVA tests. For all analyses, p values ≤ 0.05 were accepted as significant. A Pearson correlation was applied to detect any possible correlation in variables followed normal distribution; otherwise Spearman correlation was used.
Results
The AV-SVC confluence projected at T5 in 56.9% (29 cases, 14 males and 15 females), T4 in 31.4% (16, 8 males and 8 females), T6 in 9.8% (5, 3 males and 2 females) and T3 in 2% (1 female). The commonest heights were the middle (43.1%, 8 males and 22 females), lower (33.3%, 11 males and 6 females) and upper (23.5%, 6 males and 6 females) T thirds, particularly T5 middle third in 27.45% (14 cases) (Fig. 3), T4 lower third in 21.56% (11 cases), T5 upper third in 17.64% (9 cases) and T5 lower third in 11.76% (6 cases) (Table 1). Rare heights were T3 (middle) and T4 (upper) third. The AV course in relation to VC midline was classified into 3 types: 1st type (AV crossed left side of midline and back to right side into SVC) in 56.9% (29 cases, 15 males and 14 females). Among them, in 96.5% (28 cases), this course was recorded in individuals older than 53 years of age (2nd group) (Fig. 4); 2nd type (AV ascended mediastinum, slightly right of VC midline, before ending into SVC) in 37.3% (19 cases, 10 males and 9 females). Among them, in 68.4% (13 cases), this course was recorded in elder individuals (2nd group) (Fig. 5) and 3rd type (AV coursed right of VC and terminated directly into SVC) in 5.9% (3 female cases) (Fig. 6). Among them, only 1 case was identified in the 2nd group (33.3%). Mean AV and SVC diameters were 0.96 ± 0.18 cm (min 0.59, max 1.58) and 1.86 ± 0.27 cm (1.27, 2.55). Gender dimorphism was found in AV (p = 0.036) and SVC (p = 0.003) diameters (male predominance in AV and SVC diameters with mean values 1.02 ± 0.12 cm and 1.97 ± 0.27 cm) compared to females (0.91 ± 0.22 cm and 1.76 ± 0.22 cm, respectively). A slight significant increase of the AV diameter with the age (1st 0.86 ± 0.15 cm and 2nd 0.99 ± 0.18 cm) was found (p = 0.056), while SVC diameter did not influence by the age (1st 1.80 ± 0.27 cm and 2nd 1.88 ± 0.27 cm). AV and SVC diameters were positively strong correlated (**) (p = 0.001 and r = 0.467**). The (AV highest point—lower border of carina) mean distance was 2.05 ± 0.44 cm (1.11–3.58 cm). Gender dimorphism (p = 0.025) with male predominance (2.19 ± 0.46 cm) compared to females (1.91 ± 0.38 cm) was found. No age impact was detected, although a slight increase of the distance was observed in between two age groups (1st group, 1.93 ± 0.45 cm and 2nd 2.07 ± 0.44 cm). The distance AV-carina is positively correlated (*) and strong correlated (**) to AV diameter (p = 0.034, r = 0.298*) and to SVC diameter (p = 0.001, r = 0.496**), respectively.
Discussion
Diversity in the azygos vein termination height into SVC
T5 height
In the present study (patients of mean age 66.5 years), the commonest height of the AV termination into SVC was T5 (56.9%), similar to Kanchana latha et al. [15] (70%) in a sample of fetuses.
After intra-comparison of the present CTA study (51 CTAs in a Greek population) with Tatar et al. [32] study (103 CTAs in a Turkish population) a similar frequency (56.9% in Greeks and 55% in Turks) of the same height (T5) was identified.
T4 height
Krakowiak-Sarnowska et al. [16] found T4 height of termination with a high frequency of 81.4% in Polish fetuses, similar to Kanchana latha et al. [15] in a mixed cadaveric sample (91.46% of adult and 100% of children cadavers). Raghavendra and Bhosale [26] found a frequency of 53%. In Tatar et al. [32] CTA study the frequency was found in 40% and in the current CTA study in 31.4%.
T3 height
Kutoglu et al. [17], Patra et al. [24] and Dahran and Soames [8] found T3 height of termination in 66.7% [17], in 53.3% [24] and in 46.66% [8], contrariwise to the present study which concluded to this level in 2% and Raghavendra and Bhosale [26] study who found this level very rarely. Kanchana latha et al. [15] found T3 height of termination in lower frequencies (10% in fetuses and 8.54% adult cadavers).
Other heights
Raghavendra and Bhosale [26] identified T3-T4 junction in 14% and very rarely the level above T3. Possible explanations of the different frequencies in AV-SVC confluence heights may be the age impact (samples with different mean ages) and the different methods of measurements. In the current study, the mean age of patients was rather high (66.5 years), thus a lot of subjects displayed significant age-related degenerative alterations of the typical spinal anatomy. Also the present study was based on CTAs, while other studies on cadavers’ dissection. In the current study, no gender dimorphism was found, while the age impact was not investigated due to the low number of subjects (9) in the first age group.
Deviations of the AV mediastinal course and age impact
Regarding AV mediastinal course, we believe that the vessel is moving to VC midline and then passes leftward for a certain distance before came back (rightward) and terminate into SVC. Reviewing published data on AV mediastinal course, the vessel follows this displacement with ageing (Table 2, Fig. 7).
The left-sided AV and age impact
Krakowiak-Sarnowska et al. [16] (fetuses) and Kagami and Sakai [14] (newborns) found no case of left-sided AV, while Rokutannda [27] and Nathan [23] (newborns) recorded frequencies 2% and 15%, respectively. Fokutome [11] (mean age 42 years) and Tatar et al. (mean age 43 years) [32] identified the AV leftward course in 4% and 22.3%, respectively. Tateshi [33] in his cadaveric study (mean age at death 55 years) found a left-sided AV in 18%, while the present study (mean age 66.5 years) resulted in 56.9%. The present study highlights the vast majority (28 out of 29) of cases found in the ages of 49 years and above. Kagami and Sakai [14] (79 years) and Saito et al. [28] (85 years) investigating populations of higher mean age identified a left-sided AV in the higher frequencies of 85% and 94%, respectively. The above course comes in agreement only with Standing’s classic anatomical textbook [30] since in the majority of textbooks, the AV typical course is the rightward one [1, 20], found in the current study only in 5.9% (3 female cases). In such books, no further details about the age impact are provided.
Aging affects AV arrangement, altering vessel’s position from rightward to leftward of VC, before its termination into SVC. Possible explanations for such displacement could be the existence of asymmetric osteophytes on the anterior surface of T bodies, which induce mechanical pressure to vein forcing to the leftward displacement [23]. Bales [3] attributed the displacement to crossover veins, which gradually over time transpose the vessel from its regular course. Another explanation is the degenerative changes during ageing that lead to aorta elongation and cause AV deviation, as both vessels, located parallel to each other, are surrounded by dense connective tissue [14]. Normal aging induces several alterations to vessels’ morphology (luminal diameter, segment length, and local curvature) and physiology. Arteries, due to calcium deposition lose their elasticity and a slight elongation of them takes place, leading to tortuosity. Tortuosity and curvature of descending thoracic aorta increases significantly with age [4], thus we can hypothesize that the dislocated aorta drifts the adjacent AV leftward of VC. The AV arc leftward maximum extent is most often just to the left of the midline but may reach to the extreme left side of T [3]. The AV deviation was not influenced by the gender in the current study.
AV and SVC morphometry in normal and pathological subjects. The gender and age impact
In the current CTA study, the mean AV diameter was 0.96 ± 0.18 cm with higher values in males, while Tatar et al. [32] identified a lower mean value (0.81 cm) in Turks. In cadaveric studies, Dahran and Soames [8] found the lowest mean value (0.621 ± 0.136 cm) in a Scottish population and Patra et al. [24] the highest mean value (1.22 ± 0.158 cm) in Indians. Kutoglu et al. [17] found a mean value of 0.85 ± 0.125 cm in Turks and Fleischner a mean value of 0.9 cm [10].
The vein enlargement was described by Milne [18] and Milne et al. [19] in the supine position or in overhydration and renal failure cases or in mid-trimester pregnancy. In a CTA study of 82 pulmonary embolism patients, Ghuysen et al. [12] suggested that the AV and SVC diameters could be used as indicators of both severity and increased risk of mortality. Recognition of a dilated (aneurismal) AV is a key point to diagnose SVC thrombosis and should always be taken into consideration in patients with central venous catheters, and neoplasms. In an obstructed SVC due to neoplasm, the AV dilatation may occur either by direct invasion, thrombosis or extrinsic vein compression and may pose a high risk of rupture.
The current study found mean SVC diameter 1.867 ± 0.27 cm with higher values in males and the AV and SVC diameters are positively strong correlated, finding that comes in agreement with Ghuysen et al. [12] view. The current study points out that the AV higher diameters will be used as predictors for higher values of SVC diameter and mediastinum pathology.
Ageing affected significantly the AV diameter (higher statistical significant values in the 2nd age group), while the SVC diameter had higher values in individual elder than 53 years.
AV arch location in relation to carina and possible clinical implication
In the current study, the mean distance (AV arch highest point-lower margin of carina) was 2.05 ± 0.44 cm and male predominance was found (2.19 ± 0.46 cm) compared to females 1.91 ± 0.38 cm. No age impact was detected, although a slight increase of the distance was observed with ageing (1st group, 1.93 ± 0.45 cm and 2nd 2.07 ± 0.44 cm). Tatar et al. [32] found the mean value in 1.6 mm. The difference between the two CTA studies in Greek and Turk populations is very increased. Due to lack of information, we hypothesized that Tatar and co-authors [32] calculated the minimum distance (AV-inferior border of carina) and not the distance (AV arch- inferior border of carina). In the current study, positive correlations between AV diameter, SVC diameter and AV-carina distance were found. The above results are probably confirmed in pathological cases (congestive heart failure), in which, the increase of the AV and SVC diameters is obvious. For that reason, we believe that the (AV arch-lower margin of carina) distance has application in thoracic surgery, in cases of right upper lobectomy, in which exceptional accuracy and in-depth knowledge of the surgical field is fundamental to avoid severe intraoperative complications. The meticulous knowledge of SVC topography and morphometry and its distance from carina is of paramount importance for surgeons performing right sleeve pneumonectomy or right upper sleeve lobectomy, usually followed by SVC resection and reconstruction [22]. The AV course until its termination, as well as its morphometry (diameter and distance from carina) and possible variants is an essential knowledge for clinicians before addressing conditions such as aneurysms, mediastinal tumors or enlarged lymph nodes [6], as well as for surgeons planning thans-thoracic esophagectomy for esophageal cancer [34]. In such cases, the AV preoperative imaging by CTA is essential to appreciate the occurrence and grade of mediastinal metastasis from tumors of esophagus proximal or distal third [7]. Additionally, the AV CTA is a fundamental step in vein’s preservation during surgery for esophageal atresia with tracheoesophageal fistula. In such cases, the AV maintenance allows mediastinum proper drainage and decreases postoperative chest congestion and pneumonitis. It may also help in better healing of esophageal anastomosis forming an additional protective factor against anastomotic leaks [29]. The detailed preoperative imaging may also help the diagnostic process, as many pathological conditions, such as thoracic aorta aneurysms, posterior mediastinum tumors and enlarged lymph nodes mimic variant AV morphology [6]. Taking into consideration the typical range of AV diameters may be helpful in interpretation cases of vein dilatation and retroaortic anastomoses (collateral pathways) due to SVC or inferior vena cava occlusion [31] or of the azygos venous system pathological cases (non-neoplastic conditions, fibrosing mediastinitis or tuberculous adenitis) [7]. AV diameter may also serve as a predictor of mortality in patients with severe pulmonary embolism [12].
Study limitations
The low number of patients in the total sample and particularly in the younger age group, as well as the lack of investigation of pathological cases of the mediastinum. Moreover, the lack of measurements concerning the height of each vertebra (T3-T6) did not allow the comparison of the AV-SVC confluence height with vertebral body height according to age.
Conclusion
In the present study, the commonest height of the AV termination was T5, while a plethora of studies concluded to T4 level (53–100%). T3 height was also found (46.6–66.7%) by other authors. T3-T4 junction and level above T3 are rarer terminations. Safe conclusions cannot be exported in relevance to the impact of the age in AV termination, due to the fact that the current study is based on a limited sample, thus additional studies, both radiological and cadaveric should be conducted.
The AV is moving to VC midline and then passes leftward for a certain distance, before its termination into SVC, rightward. The leftward displacement is age but not gender-related, as it was concluded by the current research, based on a limited sample, similarly to other studies. The rightward deviation was identified less commonly.
AV and SVC diameters had higher significant values in males than females, while the advance age had a significant impact only in AV diameter and a positive one with higher values on SVC diameter. A positively strong correlation existed between AV and SVC diameters, indicating that higher AV diameters lead to higher SVC diameters and vice versa. The AV higher diameters will be used as predictors for higher values of SVC diameter and mediastinum pathology. In males, the AV highest point was significantly longer from the lower border of carina compared to females, while in elder subjects the distance did not differ significantly, although longer distances were recorded in elder patients compared to the younger ones. Current findings can be useful in mediastinal oncological surgery, mediastinoscopy and surgery of VC deformations, neurovascular surgery of retroperitoneal organs, disc herniation and T fractures. The CTA imaging of AV, preoperatively, is a fundamental step of investigation of its topography, morphology, morphometry and possible alterations of its arrangement in relation to VC, either in cases of ageing or in pathological cases.
References
Anson MV (1984) Surgical anatomy, 6th edn. Saunders Company, Chicago
Arey LB (1954) Developmental Anatomy, 6th ed. Philadelphia: W.B. Saunders Company; 1954.
Bales G (2014) A semi-quantitative approach to variation of the azygos vein course. Clin Anat 27:1030–1037
Belvroy VM, de Beaufort H, van Herwaarden JA, Bismuth J, Moll FL, Trimarchi S (2019) Tortuosity of the descending thoracic aorta: normal values by age. PLoS ONE 14(4):e0215549. https://doi.org/10.1371/journal.pone.0215549
Bergman RA, Thompson SA, Afifi AK. 1988. Compendium of Human Anatomic Variation. Text, Atlas, and World Literature. Baltimore: Urban & Schwarzenberg. 593 p.
Celik HH, Sargon MF, Aldur MM, Cumhur M (1996) An anomalous course of the interazygos vein. Surg Radiol Anat 18(1):61–62
Crummy AB, Wegner GP, Flaherty TT, Benfield JR, Brunette KW, Francyk WP (1968) Azygos venography: an aid in the evaluation of esophageal carcinoma. Ann Thorac Surg 6(6):522–527
Dahran N, Soames R (2016) Anatomical variations of the azygos venous system: classification and clinical relevance. Int J Morphol 4(3):1128–1136
Dudiak CM, Olson MC, Posniak HV (1991) CT evaluation of congenital and acquired abnormalities of the azygos system. Radiographics 11:233–246
Fleischner FG, Udis SW (1952) Dilatation of the azygos vein: a roentgen sign of venous engorgement. Am J Roentgenol 67:569–575
Fukutome M (1951) Vv. thoracica longitudinales observed in Japanese in Kyushu. Kumamoto Daigaku Igakubu Daini Kaibougaku Kyoshitsu Ronbun Shu 2:71–84 (in Japanese)
Ghuysen A, Ghaye B, Willems V, Lambermont B, Gerard P, Dondelinger R, D’Orio V (2005) Computed tomographic pulmonary angiography and prognostic significance in patients with acute pulmonary embolism. Thorax 60:956–961
Hollinshead WH (1971) Anatomy For Surgeons. New York: Harper & Row; 2nd Edition.
Kagami H, Sakai H (1990) The problems in the arrangement of the azygos vein. Okajimaslia Anat 67(2–3):111–114
Kanchana Latha G, Sugavasi R (2013) Study of the Azygos system of veins in human cadaver. Int J Cur Res Rev 05(08):115–117
Krakowiak- Sarnowska E, Wisniewski M, Szpinda M, Krakowiak H (2003) Variability of the azygos vein system in human fetuses. Folia Morphol 62(4):427–430
Kutoglu T, Turut M, Kocabiyik N, Ozan H, Yildirim M (2012) Anatomical analysis of azygos vein system in human cadavers. Rom J Morphol Embryol 53(4):1051–1056
Milne ENC (1973) Some new concepts of pulmonary blood flow and volume. Radiol Clin N Am 16:515–536
Milne ENC, Pistolesi M, Miniati M, Giuntini C (1984) The vascular pedicle of the heart and the vena azygos. Part I: the normal subject Radiology 152:1–8
Moore KL, Dalley AF (1999) Clinically Oriented Anatomy, 4th edn. Lippincott Williams and Wilkins, Philadelphia
Nadesan T, Keough N, Suleman FE, Lockhat Z, van Schoor AN (2019) Appraisal of the surface anatomy of the Thorax in an adolescent population. Clin Anat 32(6):762–769. https://doi.org/10.1002/ca.23351
Nakahara K, Ohno K, Mastumura A, Hirose H, Mastuda H, Nakano R, Shirakura R, Kawashima Y (1989) Extended operation for lung cancer invading the aortic arch and superior vena cava. The Journal of Thoracic and Cardiovascular Surgery 97(3):428–433
Nathan H (1960) Anatomical observations on the course of the azygos vein (vena azygos major). Thorax 15:229–232
Patra A, Singla RK, Kaur H, Malhotra V (2019) Analysis of multiple variations in azygos venous system anatomy with its classification: a cadaveric study. Eur J Anat 23(1):9–15
Piciucchi S, Barone D, Sanna S, Dubini A, Goodman LR, Oboldi D, Bertocco M, Ciccotosto C, Gavelli G, Carloni A, Poletti V (2014) The azygos vein pathway: an overview from anatomical variations to pathological changes. Insights into imaging 5(5):619–628. https://doi.org/10.1007/s13244-014-0351-3
Raghavendra AY, Bhosale SM (2017) Variations of arch of azygos vein: an anatomical overview with clinical importance. Int J Anat Res 5(32):4251–4256
Rokutanda T (1959) Nihonjin taiji ni okeru kijomyaku oyobi hannkijomyaku no jinsyu kaibogakuteki kenkyu. Kumamoto Igakukaishi 33:2168–2175 (in Japanese)
Saito A, Murakami H, Tomioka K, Ezure H, Moriyama H, Mori R, Nakajima K, Nakamura M, Otsuka N (2015) The impact of aging on the course of the azygos vein. Okajimas Folia Anat Jin 92:7–10
Sharma S, Sinha SK, Rawat JD, Wakhlu A, Kureel SN, Tandon R (2007) Azygos vein preservation in primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int 23(12):1215–1218. https://doi.org/10.1007/s00383-007-2008-5
Strandring S (2008) Gray’s Anatomy. The Anatomical Basis of Clinical Practice. 40th Ed. Edinburgh: Elsevier Churchill Livingston, p 940.
Takasugi JE, Godwin JD (1990) CT appearance of the retroaortic anastomoses of the azygos system. AJR Am J Roentgenol 154(1):41–44
Tatar I, Denk C, Celik H, Oto A, Karaosmanoglu D, Ozdemir B, Surucu S (2008) Anatomy of the azygos vein examined by computerized tomography imaging. Saudi Med J 29(11):1585–1588
Tateshi S (1939) Uber die Typen der V. azygos und V. hemiazygos. Nagasaki Igakkwai Zassi 17:2448–2455 (in Japanese)
Weijs TJ, Ruurda JP, Luyer MDP, Cuesta MA, van Hillegersberg R, Bleys RLAW (2017) New insights into the surgical anatomy of the esophagus. J Thorac Dis 9(Suppl 8):S675–S680
Williams PL, Warwick R, Dyson M, Bannister LH (1989) Gray’s anatomy, 37th Edition, 754–755. Churchill Livingstone, London
Winer-Muram HT, Rydberg J, Johnson MS, Tarver RD, Williams MD, Shah H, Namyslowski J, Conces D, Jennings SG, Ying J, Trerotola SO, Kopecky KK (2004) Suspected acute pulmonary embolism: evaluation with multi-detector row CT versus digital subtraction pulmonary arteriography. Radiology 233(3):806–815
Funding
None.
Author information
Authors and Affiliations
Contributions
KN made the project of the study, revised the paper contributed to the statistical analysis and made the proofs correction, KK and MP searched the data literature, wrote and edited the paper and made the statistical analysis, GD performed the vessels’ measurements and collected all data patients, CC and GP have edited the paper. All authors have approved the submitted draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was taken from each patient (written informed consent).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koutsouflianiotis, K., Daniil, G., Paraskevas, G. et al. Computed tomography angiography study of the azygos vein course and termination into superior vena cava: gender and age impact. Surg Radiol Anat 43, 353–361 (2021). https://doi.org/10.1007/s00276-020-02583-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-020-02583-8