Abstract
Objectives
To investigate the angulations and length of the styloid process (SP) on three-dimensional computed tomography (3D-CT) images between the patients having elongated SP complaints and those without any stylalgia symptoms.
Patients and methods
One hundred patients underwent 3D-CT evaluation of the bilateral temporomandibular joints to investigate for symptomatic elongated styloid process (ESP) at our institution. The differences between the mean angulations and lengths of the SP and comparisons between patient and control groups were analyzed by student t test.
Results
In study group, mean length of styloid processes was 40.7 ± 10.8 mm on the right and 40.3 ± 10.9 mm on the left. Mean medial angles of SP were measured as 22.60 ± 4.0 on the right side and 22.60 ± 4.5 on the left side. In the same group, mean anterior angles of SP were 16.10 ± 6.9 on the right and 16.70 ± 7.1 on the left side. The “in-group” comparisons of lengths, medial and anterior angles did not produce statistically significant results. The comparison of medial angulations between the symptomatic and asymptomatic patients was the only statistically meaningful result in our study.
Conclusion
3D-CT has several advantages according to conventional tomography for visualization of head and neck anatomy. The increase of medial angulation of SP may be responsible for the development of complaints in ESP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Styloid process (SP) is derived from the Greek word ‘Stylos’ meaning a pillar. The structure is a long, cylindrical cartilaginous bone located on the inferior aspect of temporal bone, posterior to the mastoid apex, antero-medial to the stylomastoid foramen and lateral to the jugular foramen and carotid canal [1, 8]. Medial to the SP is internal jugular vein along with 7th, 9th, 10th, 11th and 12th cranial nerves [13]. The tip of styloid process is close to the external carotid artery laterally, while medially, it is in close proximity to the internal carotid artery and accompanying sympathetic chain [4, 13]. The stylohyoid complex (SHC) consists of the SP and the stylohyoid ligament. Although the reason for its variable development characteristics is not clear, elongation of the SP is currently recognized as one of the leading causes of pain in the craniocervical region.
The Eagle’s syndrome is characterized by a series of symptoms believed to be due to an elongated styloid process and/or ossification of part or the entire stylohyoid ligament. Eagle in 1937 was the first author to define stylalgia as an autonomous entity related to abnormal length of the styloid process or stylohyoid ligament [6].
The ossified SHC can be determined through the palpation of the SP in the tonsillar fossa and induction of pain during pressure to this level [13]. Plain radiography of the neck, panoramic radiography and computed tomography of temporal bone are imaging modalities to identify elongated SP. Superposition of different structures and asymmetrical visualization of the head are major disadvantages of plain radiographs. Computed tomography (CT) is the imaging method of choice for the evaluation of the SHC anatomy. Especially, three-dimensional computed tomography (3D-CT) has several advantages according to conventional CT for visualization of head and neck anatomy [5]. Today, 3D-CT evaluation of SHC is accepted to be best method to investigate the size and morphology of the SHC [3, 7].
The purpose of this study was to measure and compare the angulations and length of the styloid processes on 3D-CT images between symptomatic and asymptomatic patients.
Materials and methods
Between December 2011 and August 2012, 200 styloid processes in 100 patients whose age ranged from 21 to 63 years (mean 40.15 ± 13.7 years) underwent CT imaging of the styloid process for complaints such as otalgia, odynophagia, tickling sensation in the throat and pain in the face were included to the study. After length of SP was measured on CT, the patients and controls whose SP had >30 mm were included in study.
All the patients underwent multislice computed tomography (MSCT) imaging of the bilateral temporomandibular joint that was to appear on the styloid process. Those patients with a history of general arthritis or other connective tissue diseases, having systemic infections, and those being treated with immunosuppressive drugs and stylohyoid ligament calcification were excluded from the study.
The control group was comprised of 100 patients (55 women, 45 men), age ranged from 18 to 60 years (mean 40.89 ± 12.9 years), who underwent computerized tomographic evaluation of paranasal sinuses, temporomandibular joints and cervical vertebraes for various reasons such as sinusitis, minor trauma. None of them had characteristic symptoms of the elongated styloid process (ESP).
All patients were informed and provided written consent according to the principles presented in the Declaration of Helsinki. The study was approved by the Ethics Committee of Bozok University Medical Faculty.
The images were acquired with a 64 slice CT (Philips Medical System, Brillance 64, Best, The Netherlands) in the supine position. After lateral scanogram examinations consisted of 120 kV, 110 mA and 0.625 mm thickness and images with bone algorithms. Axial images were obtained for the ESP and were constituted reformatted three-dimensional CT images. SP was evaluated on axial, coronal and sagittal planes. The length, medial and anterior angulations of each ESP and control group were measured on both sides. The length of an SP was measured between the attachment point of the temporal bone and tip of the SP on coronal reformat images (Fig. 1). A vertical line was passed from of the midline of odontoid process and another vertical line was passed from end point of the SP on coronal images. Then, the angle between two lines was measured as medial angle (Fig. 2). A vertical line was passed from the cranial base of the process, and then a horizontal line was drawn between 90° perpendicular to this line and end point of SP. Anterior angulation was defined as between two lines which were perpendicular to each other passed from cranial base of the SP and body of the SP (Fig. 3).
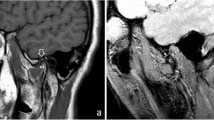
The relation between neighboring structures and ESP was shown in asymptomatic and symptomatic patients on CT images (Figs. 4a, b, 5a, b).
Coronal MIP image (a) showed that the tip of SP is close to the internal carotid artery (arrow) in symptomatic patient who had medial angulation of SP. Coronal MIP image (b) showed no proximity to the pharyngeal wall and internal carotid artery (arrow) of the SP in asymptomatic patient who did not had medial angulation of SP
Statistical analysis
Data analysis and all statistical tests were performed using SPSS 15.0 for Windows (SPSS, Inc, Chicago, IL, USA). All data were presented as means and standard errors. Differences between the patient and control groups were assessed by analysis student t test. Pearson correlation test was used to evaluate between length and angulation of SP relationship. Statistical significance was considered at p < 0.05.
Results
Sixty-six of the patients were female and 34 were male. The mean age was 40.3 ± 11 years old for female and 40 ± 15 years old for male. Fifty-five of controls were female and 45 were male. The mean age was 42 ± 14 years old for female and 39 ± 13 years old for male. All of the patients and controls had elongated SP (>30 mm).
In the study group, mean length of styloid processes was 40.7 ± 10.8 mm on the right and 40.3 ± 10.9 mm on the left. Mean medial angles of SP were measured as 22.6° ± 4.0° on the right side and 22.6° ± 4.5° on the left side. In the same group, mean anterior angles of SP were 16.10° ± 6.9° on the right and 16.7° ± 7.1° on the left side. In the control group, mean length of styloid processes was 38.8 ± 6.5 mm on the right and 39.4 ± 8.9 mm on the left side. Mean medial angles of SP were 20.6° ± 4.9° on the right and 21.3° ± 3.8° on the left. Mean anterior angles of SP were 14.7° ± 5.9° on the right and 15.4° ± 6.2° on the left. Mean length and mean medial and anterior angle of SP in the study and control groups are shown in Table 1. There was no statistical difference between the patient and control group for the length of the SP on the both sides (p > 0.05). No differences were noted between the patient and control group for the anterior angulation of the SP on the right and left side. For the medial angulation of SP, there was a statistically significant difference between the patient and control groups (p = 0.003). There was no statistical correlation between the length and medial angulation of SP. The correlation between length and anterior angulation of SP was limited (r 0.2, p < 0.05). The correlation between anterior and medial angulation of SP was moderate (r 0.3, p < 0.001). There was no statistical concordance between length and angles values in different sex and age groups (Table 2).
Discussion
Symptoms related to an elongated styloid process were first described by Weinlecher in 1872. Eagle (in 1937 and 1949) defined stylalgia as an autonomous entity related to abnormal length of the styloid process or to mineralization of the stylohyoid ligament complex [6]. The term stylalgia defines an SP that is longer than normal (25–30 mm) associated with advanced calcification of the process and its ligaments. Eagle syndrome is an aggregate of symptoms that includes recurrent throat pain, foreign body sensation, dysphagia, and/or facial pain as a direct result of an ESP or calcified stylohyoid ligament [10]. The patients with ESP seek treatment in several different clinics such as otolaryngology, family practice, neurology, neurosurgery, psychiatry and dentistry due to nonspecific clinical findings [9].
Approximately, 4 % of the population is thought to have an ESP, only a small percentage (between 4 and 10.3 %) of this group is thought to be actually symptomatic [9]. It is more common in women than men in radiography (male/female ratio was 1/9) [9, 10]. Although Eagle syndrome is thought to be caused by an ESP or calcified stylohyoid ligament, the presence of an ESP is not pathognomonic for Eagle syndrome because many patients with incidental findings of an ESP are asymptomatic.
The etiology and pathogenesis of this syndrome are controversial. The SP is normally composed of dense connective tissue in adults but may retain its embryonic cartilage and the potential for ossification [9].
A thorough medical history and physical examination is the mainstay for the diagnosis of ESP. Occasionally, it is possible to feel an ESP by careful intraoral palpation. SP with a normal length is usually not palpable [11]. Several imaging modalities such as lateral head and neck radiography, panoramic radiography, lateral-oblique mandible radiography, etc. can be used for the diagnosis of this entity. However, it may be difficult to determine the length and orientation of the ESP by plain radiography because of superposition of different radio-opaque structures [11]. The length and morphology of the SP and its relationships to surrounding structures are best assessable on multislice CT, 3D-CT, multiplanar reconstruction (MPR) and maximum intensity projection (MIP) [13]. ESP was not demonstrable by standard coronal and sagittal reformatted images at full length due to its antero-medial extension. Three-dimensional CT technique was used in our study to visualize SP at full length. The antero-medial angulation of SP was readily demonstrated by this technique.
There are different reports about the normal length of the SP. Generally, an SP measuring 2.5 cm in length is considered as normal. An SP >3 cm is defined as ESP [14]. In this study, if an SP is >3 cm, it was defined as ESP in all groups and the longest SP that we have measured was 74 mm. Mean length of SP was 40.7 mm in patients and 40 mm in controls. It seems that the length is not enough to explain these complaints. It was reported that the length of SP age and sex groups was not significantly different, that is parallel to our results [12–15]. The prevalence of symptomatic ESP is not precisely known [3, 16]. It was reported that incidence of the ESP was 0.4–50 % in population and only half of these (or less) were symptomatic [2]. Many patients with incidental findings of ESP are asymptomatic. It was proposed that abnormal angulations rather than elongation of SP may be responsible for the complaints.
In this study, the mean angles were 22.6° and 16.4° for the medial and anterior, respectively. Yavuz et al. [15] reported that mean angles were 15.5° and 35.1° for the medial and anterior, respectively. They concluded that anterior angulation of SP was an important factor on symptoms. Our results suggest that angulation of SP may cause the symptoms due to compression of adjacent structures. Contrarily, we could not show any positive correlation between the chief complaints and increased anterior angulations of ESP. On the other hand, we demonstrated a strongly positive correlation between the complaints and medial angulations. Explanation for this correlation may be that increase of medial angle lead closer contact between the SP tip and internal carotid artery which may be responsible for development of the symptoms (Fig. 4a). In addition, the irritation of adjacent structures such as lateral pharyngeal wall (Fig. 5a, b) and/or, sympathetic chain may also contribute to the clinical picture. No correlation between the medial angle and the length of SP, and only minimal correlation between the anterior angle and the length were noted. The increase in medial and anterior angles was concomitant to each other. With regard to gender and age groups the differences between these two angles were not significant.
The main problem of patients with ESP will not be described clearly because these symptoms can be related to several diseases. Therefore, structural measurements of SHC may be quite important and this situation should consider the patients with clinical symptoms like cervicofacial pain.
In conclusion, our study results revealed that rather than the anterior angulation or the length of SP, the increased medial angulations of SP might be responsible for stylalgia complaints in these patients. Reformatted 3D-CT images give detailed and reliable information about styloid length and angles.
References
Alpoz E, Akar GC, Celik S, Govsa F, Lomcali G (2013) Prevalence and pattern of stylohyoid chain complex patterns detected by panoramic radiographs among Turkish population. Surg Radiol Anat. doi:10.1007/s00276-013-1137-x
Başekim CC, Mutlu H, Güngör A, Silit E, Pekkafali Z, Kutlay M et al (2005) Evaluation of styloid process by three-dimensional computed tomography. Eur Radiol 15:134–139
Cağlayan F, Tozoğlu U (2012) Incidental findings in the maxillofacial region detected by cone beam CT. Diagn Interv Radiol 18:159–163
Camarda J, Forest D II (1989) Stylohyoid chain ossification: a discussion of etiology. Oral Surg Oral Med Oral Pathol 67:515–520
Degirmenci B, Yılmaz O (2013) Variations of transverse foramens of cervical vertebrae: a 3-dimensional multidetector CT study. Turk J Med Sci 43:711–717
Eagle WW (1937) Elongated styloid process: report of two cases. Arch Otolaryngol 25:584–586
Kaplanoglu H, Kaplanoglu V, Toprak U, Hekimoglu B (2013) Surgical measurement of the sphenoid sinus on sagittal reformatted CT in the Turkish population. EAJM 45:7–15
Keur JJ, Campbell JP, McCarthy JF, Ralph WJ (1986) The clinical significance of the elongated styloid process. Oral Surg Oral Med Oral Pathol 61:399–404
Khandelwal S, Hada YS, Harsh A (2011) Eagle’s syndrome—a case report and review of the literature. Saudi Den J 23:211–215
Krmpotić Nemanić J, Vinter I, Ehrenfreund T, Marusić A (2009) Postnatal changes in the styloid process, vagina processus styloidei, and stylomastoid foramen in relation to the function of muscles originating from the styloid process. Surg Radiol Anat 31:343–348
Montalbetti L, Ferrandi D, Pergami P, Savoldi F (1995) Elongated styloid process and Eagle’s syndrome. Cephalalgia 15:80–93
Onbas O, Kantarci M, Murat Karasen R, Durur I, Cinar Basekim C, Alper F et al (2005) Angulation, length, and morphology of the styloid process of the temporal bone analyzed by multidetector computed tomography. Acta Radiol 46:881–886
Ozgur Z, Govsa F, Celik S, Ozgur T (2010) An unreported anatomical finding: unusual insertions of the stylohyoid and digastric muscles. Surg Radiol Anat 32:513–517
Palesy P, Murray GM, De Boever J, Klineberg I (2000) The involvement of the styloid process in head and neck pain—a preliminary study. J Oral Rehabil 27:275–287
Yavuz H, Caylakli F, Yildirim T, Ozluoglu LN (2008) Angulation of the styloid process in Eagle’s syndrome. Eur Arch Otorhinolaryngol 265:1393–1396
Yetiser S, Gerek M, Ozkaptan Y (1997) Elongated styloid process: diagnostic problems related to symptomatology. Cranio 15:236–241
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okur, A., Özkırış, M., Serin, H.İ. et al. Is there a relationship between symptoms of patients and tomographic characteristics of styloid process?. Surg Radiol Anat 36, 627–632 (2014). https://doi.org/10.1007/s00276-013-1213-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-013-1213-2