Abstract
Purpose
The palatal mucosa is a major donor site for connective tissue in the field of periodontal plastic surgery, since it satisfies both the esthetic and functional demands of patients. The purpose of this study was to use histomorphometric analysis to measure the thicknesses of the palatal mucosa and the lamina propria including the epithelium on cadavers.
Methods
Thirty-four hemimaxillae of cadavers were examined (13 male and 4 female, mean age 57.2 years). Each maxilla was processed for histological sectioning and subsequently for histomorphometric analysis. The thicknesses of the palatal mucosa and the lamina propria including the epithelium were measured at three points starting from the alveolar crest, at intervals of 4 mm, with the aid of Adobe Photoshop.
Results
The thickness of the palatal mucosa at the alveolar crest and at 4 and 8 mm below the alveolar crest were 2.51 ± 0.83 (mean ± SD), 2.92 ± 0.80, and 3.62 ± 0.99 mm, respectively, and thus increasing from the alveolar crest toward the midpalatal suture. Conversely, the thicknesses of the lamina propria including the epithelium at these same positions were 2.06 ± 0.70, 1.54 ± 0.48, and 1.28 ± 0.46 mm, respectively, thus decreasing toward the midpalatal suture.
Conclusions
The present results indicate that clinicians need to be particularly careful when harvesting palatal mucosa that is destined to be used as autogenous donor material for connective tissue in periodontal plastic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal plastic surgery with keratinized mucosa of appropriate thickness is used for root coverage, alveolar ridge augmentation, and for the treatment of exposed areas around implants [4, 7, 16]. In such cases, the palatal mucosa is used widely as a donor site for connective tissue grafts. An appropriate thickness of the donor site palatal mucosa will stimulate revascularization in the recipient site and thus produce esthetically and functionally good results [11]. However, harvested mucosa that is too thin will complicate the graft manipulation and result in shrinkage, while harvested mucosa that is too thick will prolong the revascularization and healing periods [11]. The thickness of the palatal mucosa is thus very important to both the treatment method and the outcome prognosis [17].
Numerous investigators have evaluated the thickness of the palatal mucosa using various methods [1, 6, 8, 12, 17–19, 21, 22], with direct bone sounding, using a periodontal probe frequently being used as a preliminary test. However, there are errors associated with this test due to the increase in tissue volume caused by anesthesia infiltration, the pressure against the palate on probing, and the tissue displacement that occurs during probing [17, 19]. Terakura [21] found a strong correlation between measurements of palatal mucosa thickness made using an ultrasound device and direct bone sounding. He concluded that ultrasound, which does not require anesthesia or periodontal probing, could replace direct bone sounding to measure palatal mucosa thickness. However, although measurement using an ultrasound device is noninvasive and convenient, it also has drawbacks: it is difficult to reapply to identical sites, there is a relatively large measurement error due to the diverse anatomical structures of the palate [12], and it is not reliable in areas where the palatal mucosa is thicker than 0.6 mm [8]. Another alternative is computed tomography (CT), which has been used in this field primarily to measure the oral soft tissues due to it being noninvasive, convenient, and easily standardized, with readily available data storage. However, it has been reported that the resolution of soft tissue is lower with this method due to the low contrast resolution [1, 6, 17].
Most relevant studies have been conducted only on the entire thickness of the palatal mucosa by a quantitative method. Recently, although certain studies measured the thickness of the epithelium or a part of it which was trimmed the grafts obtained from patients [2, 9], few studies have investigated the thickness of the lamina propria including the epithelium which is the more important part when it comes to graft tissue [20]. Therefore, the purpose of the present study was to use histomorphometric analysis to measure the thickness of the palatal mucosa and lamina propria including the epithelium on cadavers, which is very important for the success of connective tissue grafting.
Materials and methods
We examined 34 hemimaxillae obtained from 17 Korean cadavers (13 males, 4 females), which had been donated for educational purposes to the Department of Anatomy, Chosun University School of Medicine. The age at death ranged from 39 to 73 years (mean age 57.2 years). The thickness of the palatal mucosa was measured relative to tooth site by selecting maxilla with dentulous dentition containing all teeth from the canine to the second molar.
All of the specimens were decalcified by soaking them for 2 months in a decalcification solution (8 N formic acid + 1 N sodium formate), after which they were neutralized in distilled water for 12 h. Each maxilla specimen was cut at the proximal surface of each tooth from the canine to the second molar, perpendicular to the midpalatal suture, using a microtome blade (Feather, Osaka, Japan). These tissue blocks were processed for embedding in paraffin by conventional methods, based on the distal surface of the cut block, and then sectioned at a thickness of 7 μm. The sections were mounted on glass slides, stained with hematoxylin-eosin, and then examined using a light microscope (EZ4HD, Leica, Wetzlar, Germany) equipped with an image acquiring system (LAS Basic v4.0, Leica, Wetzlar, Germany).
On each of the histologic images, the long axis of the alveolar bone was set to connect the center point of the alveolar crest with the center point of the alveolar process with reference to the extension line passing through 12 mm below the alveolar crest. The palatal mucosa thickness was then measured at three points starting from the alveolar crest, at intervals of 4 mm vertical to the long axis of the alveolar bone. At these three sites, the thickness of the palatal mucosa was measured from the mucosa surface to the alveolar bone, and the lamina propria including the epithelium was measured in the direction perpendicular to the surface of the palatal mucosa, using Adobe Photoshop CS4 version 11 (Adobe, CA, USA) to an accuracy of 0.01 mm (Fig. 1). All measurements were made in duplicate by two investigators.
Points of measurement of the thickness of palatal mucosa and lamina propria. a Diagram of the interdental section. b Histologic section (H & E stain; bar 500 μm). The unbroken arrow indicates the thickness of the lamina propria of the palatal mucosa including the epithelium, and the broken arrow indicates the thickness of the palatal mucosa. The dashed line indicates a dividing line between the connective tissue and the submucosa. LA long axis of the alveolar bone, AC alveolar crest, LP lamina propria, PM palatal mucosa
All statistical analyses were performed using SPSS 12.0 (SPSS, Chicago, IL, USA). One-way ANOVA was used to analyze the descriptive statistics, interobserver difference, and differences between the right and left sides. Since no significant interobserver differences were found (p = 0.861), the mean of the duplicate measurements was used as the final measurement value. Similarly, there were no significant differences between the right and left sides (p = 0.596), and so the measurements from the two sides at each position were pooled and assigned to a single group. No distinction was made between male and female cadavers. In addition, measurements were analyzed according to tooth site and measurement point (i.e., at the alveolar crest or 4 or 8 mm below it) by one-way ANOVA with a post hoc comparison using Scheffé’s method. The level of statistical significance was set at p < 0.05.
Results
The thickness of the palatal mucosa from its surface to the alveolar bone was smallest at the alveolar crest at the distal surface of the second molar (1.91 ± 1.04 mm, mean ± SD), and greatest at 8 mm below the alveolar crest at the distal surface of the second molar (4.16 ± 1.42 mm). The thicknesses of the palatal mucosa at the alveolar crest and at 4 and 8 mm below it were 2.51 ± 0.83, 2.92 ± 0.80, and 3.62 ± 0.99 mm, respectively. Thus, the thickness of the palatal mucosa increased from the alveolar crest toward the midpalatal suture at all tooth sites (Table 1).
The thickness of the lamina propria including the epithelium was smallest at 8 mm below the alveolar crest at the distal surface of the second molar (0.98 ± 0.36 mm) and greatest at the alveolar crest at the distal surface of the first molar (2.39 ± 0.76 mm). The thicknesses of the lamina propria including the epithelium at the alveolar crest and at 4 and 8 mm below it were 2.06 ± 0.70, 1.54 ± 0.48, and 1.28 ± 0.46 mm, respectively. Thus, in contrast to the entire palatal mucosa, the thickness of this portion of the palatal mucosa decreased from the alveolar crest toward the midpalatal suture at all tooth sites (Table 2).
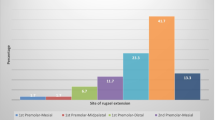
The thickness of the palatal mucosa did not differ significantly between the different tooth sites (p = 0.203). However, the thickness of the lamina propria including the epithelium did differ according to tooth site, being greatest at the distal surface of the first molar (1.92 ± 0.67 mm) and smallest at the distal surface of the second molar (1.32 ± 0.76 mm; Figs. 2, 3).
Histologic section of the palatal mucosa at different tooth sites. The thickness of the lamina propria including the epithelium decreased toward midpalatal suture at all tooth sites, in contrast to that of the palatal mucosa. a Distal surface of the canine. b Distal surface of the first premolar. c Distal surface of the second premolar. d Distal surface of the first molar. e Distal surface of the second molar. AB alveolar bone, Epi epithelium, GT glandular tissue (H & E stain; bar 500 μm)
Discussion
Diverse periodontal plastic surgery procedures have been widely applied to resolve esthetic problems and hypersensitivity caused by gingival recession, and have primarily involved free gingival grafts, subepithelial connective tissue grafts, and guided tissue regeneration. Among these procedures, subepithelial connective tissue grafting using the palatal mucosa as a donor site was shown to have superior restoration outcomes [15].
In periodontal plastic surgery, because it is required the vascularization for the nourishment and the resistance to functional stress, the graft thickness is the primary factor in the graft survival [20]. That is, placing of grafts that are too thin may result in atrophy or necrosis at the recipient site, while placing of grafts that are too thick may lead to severe pain, hemorrhage, and a deep wound at the donor site, and a prolonged treatment period, unesthetic results at the recipient site (e.g., mismatching colors and the formation of a keloid) [11, 22].
It has been shown that the lamina propria of the palatal mucosa at the donor site, which is the connective tissue that supports the oral epithelium, is an important factor in determining the success of a graft. The lamina propria consists of the papillary layer, which is connected to the epithelial ridge close to the epithelium, and the underlying reticular layer [13]. The papillary layer contains numerous capillary loops, and the reticular layer contains thick bundles of collagen fibers which support the epithelium [13, 20]. Also, as connective tissue grafts, they show successful clinical results regardless of whether the epithelium is included or not, and it is unknown whether the critical amount of the epithelium will be acting to tolerate the clinical result [2]. Thus, as a graft tissue, the success of connective tissue graft will be determined by the uniformity of lamina propria including epithelium thickness. However, the histologic makeup of palatal mucosa as an autogenous graft material is shown a wide variation [2], and its thickness varies according to its location. It is therefore clear that a detailed anatomical knowledge regarding the thickness of the palatal mucosa and the lamina propria including epithelium except the submucosa is a prerequisite for the selection of the most appropriate treatment method and determination of potential prognosis, such as the likelihood of revascularization or tissue atrophy during recovery.
Mörmann et al. [11] reported that the ideal thickness of the palatal mucosa for the keratinized mucosa grafting is approximately 0.9 mm, including the epithelium and lamina propria, with a homogeneous thickness. In the present study, the lamina propria including epithelium was thinnest at the distal surface of the second molar (1.32 mm); based on this measurement, it appears that the palatal mucosa at any tooth position could be used as a graft site for connective tissues.
However, in the canine area, the thickness of the lamina propria including epithelium is not homogeneous due to anatomical structures such as the transverse palatine folds, and the palatal neurovascular bundles rapidly come close to the gingival margin in the canine distal area [14]. Therefore, it might be dangerous to obtain connective tissue for autogenous grafts from the canine area. Similarly, in the second molar area, it would be difficult to use this as a donor area. Since the greater palatine foramen is mainly located the palatal side of third molar, but it shows the opening of oval shape in longitudinal length of 4.9 mm at the distal surface of second molar with a high frequency of 23.1 % [10]. The palatal neurovascular bundles passing through this foramen are generally located 7–17 mm below the cementoenamel junction, notwithstanding differences associated with the height of the palatal vault [14, 17].
In the premolar areas, the thickness of the palatal mucosa, which comprises mainly the epithelium and lamina propria, was both homogeneous and sufficient, rendering this area suitable as for autogenous grafting [17, 19, 22]. In the present study, it was found that the thickness of the lamina propria including epithelium composed of the dense connective tissue decreased from the alveolar crest, down to 1.28 mm at 8 mm below the alveolar crest. Therefore, it appears that the palatal mucosa in the premolar area, from the alveolar crest to 8 mm below it, is suitable as a donor area for graft material.
The first molar area is anatomically restrictive regarding graft material because of the root on the palatal side [19], the prominence of this palatal root results in a large, protruding alveolar bone, over which the mucosa is relatively thin and contains only the epithelium [11]. As mentioned above, if only the epithelium is grafted, the grafted epithelium would necrotize and the recipient site would be reformed with the gingival mucosa [3]. Thus, the first molar area, with its characteristically thin mucosa, could have serious limitations as a connective tissue graft.
However, in the present study it was found that the mean thickness of the palatal mucosa was 2.92 mm and the mean thickness of the lamina propria including epithelium was 1.92 mm at the distal surface of the first molar. This means that approximately 1 mm of the submucosa appears to be inserted below the lamina propria. In addition, according to the CT data reported by Song et al. [17], the entire thickness of the central area of the first molar is 3.13 mm. In other words, although the palatal mucosa at the first molar is thin, it does not comprise only epithelium. Thus, with a careful technique and accurate anatomical knowledge, this area could be used successfully as a donor site for connective tissues.
In the present study, the entire thickness of the palatal mucosa increased from the distal surface of the canine to the distal surface of the first premolar (3.28 mm) but decreased toward the distal surface of the second molar. However, these measurements did not differ significantly among the teeth. Such results show a tendency different from previous reports in which the thickness of the palatal mucosa was found to increase from the canine to the premolar area, but decrease at the first molar, and then increase again toward the second molar [17, 22]. These differences in thickness between studies may be due to differences in the measurement methods and measurement sites used.
With regard to measurement method, loosening of the soft tissues during the preparation of samples for qualitative evaluation was prevented in the present study by including the alveolar bone in the sample blocks, and subsequently in the decalcification and paraffin embedding procedures. Nonetheless, problems due to the tissue shrinkage after histologic preparation, presence of inflammation in the palatal mucosa, and insufficient decalcification of samples were still detected. Thus, improvement in the tissue preparation of samples should be a focus of future studies.
Since the thickness of the palatal mucosa increased from the gingival margin to the midpalatal suture, it may be safer to obtain graft materials further from the gingival margin [1, 17, 20]. Conversely, the thickness of the lamina propria including epithelium, which is important for revascularization and resistance to functional stress, decreased from the alveolar crest to the midpalatal suture. And the mean height of greater palatine sulcus rim along the slope of alveolar process of maxilla, in which there was the greater palatine artery to supply the blood in hard palate, was decreased from 7.9 mm the second molar to 5.7 mm the first premolar [5]. Therefore, it was considered that the deeper and further the incision makes to obtain large grafts [2], the more the amount of submucosa contained the fat and gland and the less the amount of lamina propria. Concurrently, the potential for damage to the greater palatine artery was increased. Hence, close attention should be paid during graft harvesting from donor sites deeper and further relative to the alveolar crest.
In conclusion, in contrast to the thickness of the palatal mucosa, the thickness of the lamina propria including the epithelium decreased toward the midpalatal suture. Therefore, more comprehensive attention should be paid to the donor site while using the palatal mucosa as an autogenous donor material for connective tissue in periodontal plastic surgery.
References
Barriviera M, Duarte WR, Januário AL, Faber J, Bezerra AC (2009) A new method to assess and measure palatal masticatory mucosa by cone-beam computerized tomography. J Clin Periodontol 36:564–568
Harris RJ (2003) Histologic evaluation of connective tissue grafts in humans. Int J Periodontics Restorative Dent 16:130–137
Karring T, Cumming BR, Oliver RC, Löe H (1975) The origin of granulation tissue and its impact on postoperative results of mucogingival surgery. J Periodontol 46:577–585
Khoury F, Happe A (2000) The palatal subepithelial connective tissue flap method for soft tissue management to cover maxillary defects: a clinical report. Int J Oral Maxillofac Implants 15:415–418
Klosek SK, Rungruang T (2009) Anatomical study of the greater palatine artery and related structures of the palatal vault: considerations for palate as the subepithelial connective tissue graft donor site. Surg Radiol Anat 31:245–250
Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A (2004) Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants 19:228–231
Langer L, Langer B (1993) The subepithelial connective tissue graft for treatment of gingival recession. Dent Clin North Am 37:243–264
Lawson RB, Jones ML (1998) An evaluation of a noninvasive method of assessing alveolar bone levels in an experimental model of cleft lip and palate. Cleft Palate Craniofac J 35:1–8
Lee YJ, Kwon YH, Park JB, Herr Y, Shin SI, Heo SJ, Chung JH (2010) Epithelial thickness of the palatal mucosa: a histomorphometric study in Koreans. Anat Rec (Hoboken) 293:1966–1970
Methathrathip D, Apinhasmit W, Chompoopong S, Lertsirithong A, Ariyawatkul T, Sangvichien S (2005) Anatomy of greater palatine foramen and canal and pterygopalatine fossa in Thais: considerations for maxillary nerve block. Surg Radiol Anat 27:511–516
Mörmann W, Schaer F, Firestone AR (1981) The relationship between success of free gingival grafts and transplant thickness. Revascularization and shrinkage–a one year clinical study. J Periodontol 52:74–80
Müller HP, Schaller N, Eger T (1999) Ultrasonic determination of thickness of masticatory mucosa: a methodologic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:248–253
Nanci A (2005) Ten cate’s oral histology development, structure, and function. In: Oral Mucosa, 6th edn. Daehan Publishing Co, Seoul, pp 333–376 (in Korean)
Reiser GM, Bruno JF, Mahan PE, Larkin L (1996) The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent 16:130–137
Sedon CL, Breault LG, Covington LL, Bishop BG (2005) The subepithelial connective tissue graft: part II. Histologic healing and clinical root coverage. J Contemp Dent Pract 6:139–150
Seibert JS, Salama H (1996) Alveolar ridge preservation and reconstruction. Periodontol 2000 11:69–84
Song JE, Um YJ, Kim CS, Choi SH, Cho KS, Kim CK, Chai JK, Jung UW (2008) Thickness of posterior palatal masticatory mucosa: the use of computerized tomography. J Periodontol 79:406–412
Stipetić J, Hrala Z, Celebić A (2005) Thickness of masticatory mucosa in the human hard palate and tuberosity dependent on gender and body mass index. Coll Antropol 29:243–247
Studer SP, Allen EP, Rees TC, Kouba A (1997) The thickness of masticatory mucosa in the human hard palate and tuberosity as potential donor sites for ridge augmentation procedures. J Periodontol 68:145–151
Sullivan HC, Atkins JH (1968) Free autogenous gingival grafts. Principles of successful grafting. Periodontics 6:121–129
Terakura T (1986) Non-invasive thickness measurement of the oral soft tissue. J Jpn Prosthodont Soc 30:1402–1411
Wara-aswapati N, Pitiphat W, Chandrapho N, Rattanayatikul C, Karimbux N (2001) Thickness of palatal masticatory mucosa associated with age. J Periodontol 72:1407–1412
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF-2011-0007227).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sun-Kyoung Yu and Baek-Hee Lee have contributed equally.
Rights and permissions
About this article
Cite this article
Yu, SK., Lee, BH., Lee, MH. et al. Histomorphometric analysis of the palatal mucosa associated with periodontal plastic surgery on cadavers. Surg Radiol Anat 35, 463–469 (2013). https://doi.org/10.1007/s00276-012-1066-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-012-1066-0