Abstract
Objectives
The aim of the present study is to provide a detailed macroscopic mapping of the palatal and tuberal blood supply applying anatomical methods and studying specific anastomoses to bridge the gap between basic structural and empirical clinical knowledge.
Materials and methods
Ten cadavers (three dentate, seven edentulous) have been prepared for this study in the Department of Anatomy, Semmelweis University, Budapest, Hungary, and in the Department of Anatomy of the Medical University of Graz. All cadavers were fixed with Thiel’s solution. For the macroscopic analysis of the blood vessels supplying the palatal mucosa, corrosion casting in four cadavers and latex milk injection in other six cadavers were performed.
Results
We recorded major- and secondary branches of the greater palatine artery (GPA) and its relation to the palatine spine, different anastomoses with the nasopalatine artery (NPA), and lesser palatal artery (LPA) as well as with contralateral branches of the GPA. Penetrating intraosseous branches at the premolar-canine area were also detected. In edentulous patients, the GPA developed a curvy pathway in the premolar area. The blood supply around the maxillary tuberosity was also presented.
Conclusion
The combination of different staining methods has shed light to findings with relevance to palatal blood supply, offering a powerful tool for the design and execution of surgical interventions involving the hard palate.
Clinical relevance
The present study provides clinicians with a good basis to understand the anatomical background of palatal and tuberal blood supply. This might enable clinicians to design optimized incision- and flap designs. As a result, the risk of intraoperative bleeding and postoperative wound healing complications related to impaired blood supply can be minimized.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Successful flap designs in daily clinical practice highly depend on the knowledge of blood vessel distribution, which will affect the angiogenesis, circulation, and primary wound healing [1] of surgical interventions in the oral cavity. The blood supply of the oral cavity, and the palate in particular, shows a complex pattern, mainly supplied by branches of the maxillary, facial, and ascending pharyngeal arteries, taking their origins from the external carotid artery. The greater palatine artery (GPA) emerges from the greater palatine foramen located on the hard palate between the second and third maxillary molars. Further behind, there are the lesser palatine foramina where the branches of the lesser palatine artery (LPA) emerge. These arteries will supply the majority of the hard palate together with the soft palate. The branches of GPA travel within the palatal bony groove divided into medial and lateral palatine grooves by the palatine spine [2,3,4]. The medial palatine groove contains the greater palatine nerve whereas the GPA lies in the lateral groove to supply the mucosa, periosteum, and palatal gingiva before entering the incisive foramen to form an anastomosis with the nasopalatine artery (NPA). The NPA enters the incisive canal to supply the anterior region of the hard palate (i.e., intermaxillary segment). Here an anastomotic network is formed between the NPA and the GPA, supplying the majority of the palatal mucosa and periosteum.
Following oral surgical interventions, it is of high importance to be aware of the interrelation between the different anatomical entities to aid the surgeon in flap design to offer the most optimal circumstances for wound healing and revascularization. Information provided by anatomical atlases does not present clinically relevant details of the palatal vascular network (ipsi- and contralateral anastomoses, individual changes of vascular pathways due to loss of dentition). Providing a solid anatomical basis on local characteristics of the hard palate might enable clinicians to avoid intra- and postoperative complications when planning oral surgery interventions by optimized incision- and flap designs. There are several surgery types, concerning maxillofacial/oral surgical or periodontal treatment, where a well-established knowledge of secure incision lines and surgical approaches would be highly beneficial: harvesting of subepithelial connective tissue grafts (SCTG) [5,6,7,8], free gingival grafts (FGG) [9,10,11,12], removal of impacted canines [13, 14], flaps to allow implant placement [15], sinus floor elevation [16], and ridge augmentation procedures [17,18,19]. Although the morphological features of palatal structures have previously been thoroughly investigated [20,21,22], clinicians still frequently face anatomical challenges during surgeries, and there is a growing need for a comprehensive macroscopical mapping of the palatal mucosal blood supply in order to avoid dangerous intraoperative and postoperative complications. According to literature, investigation of the blood flow in oral mucosa can be performed by in vivo angiography, laser Doppler, or laser speckle analysis [23,24,25,26]. These approaches do provide valuable clinical data on functional changes in blood circulation following thermal, mechanical, or chemical stimuli and might as well be used for monitoring postoperative wound healing patterns following oral surgery or periodontal surgery interventions [26]. Nevertheless, these in vivo approaches are only capable of providing indirect information on blood vessel function and structures, thus more definitive ex vivo macro- and microscopical studies are needed to provide a solid anatomical basis for the physiological observations made by blood flow analyzing methods. Several staining methods exist, which might be used to stain the blood vessels of the palate such as latex milk injection [27], corrosion casting [28] used for macroscopical analysis, they all can be used in human cadavers by injecting a substance through the external carotid artery.
Aims
The aim of the present human cadaver study is to provide a detailed macroscopic mapping of the palatal and tuberal blood supply applying anatomical methods and studying specific anastomoses to bridge the gap between basic structural and empirical clinical knowledge. Thus, we aim to provide clinicians with a good basis to understand the anatomical background of intra- and postoperative complications, as well as early wound healing events of palatal surgical interventions.
Materials and methods
Ten cadavers have been prepared for this study; all dissections were performed by trained investigators (A.S and A.G). Six Hungarian cadavers (three males, three females; one dentate, five edentulous) which were 65–84 years of age were donated to the Department of Anatomy for educational and research purposes according to Hungarian approval rules of anatomical donation and they were prepared and dissected in the Department of Anatomy, Semmelweis University, Budapest, Hungary. Further, four cadavers (two males, two females; two dentate, two edentulous) which were 59–90 years of age, were donated to the Department of Anatomy of the Medical University of Graz complying with the Anatomical Donation Program of the Medical University of Graz and in accordance with the Austrian law were investigated bilaterally. All cadavers were of Caucasian origin. Specimens were fixed with Thiel’s solution [29, 30]. For the macroscopic analysis of the blood vessels supplying the palatal mucosa, multiple techniques have been used. Corrosion casting in four cadavers and latex milk injection in other six cadavers were performed. Linear measurements on the distance between alveolar crest and GPA were taken using a standard paper ruler. Descriptive statistical evaluation was performed by presenting mean and standard deviation data. Digital photographs were taken of each specimen from multiple directions with a magnification range of 1:1 to 1:3 using a macro lens mounted to a digital single lens reflex camera equipped with a ring light (Canon 600D, Canon 100 mm 2.8 macro lens, Canon MR-14 EX ring light). Photographs were analyzed by visual inspection on a calibrated monitor in 1:1 magnification.
Macroscopic analysis
Corrosion casting
This method was applied on the cadavers which were donated to the Department of Anatomy, Semmelweis University, Budapest, Hungary, to reveal the complexity of blood vessels in three dimensions in relation to osseous anatomical landmarks as a result of complete maceration of soft tissues. The external carotid arteries (ECA) were flushed with phosphate-buffered saline (PBS) under the pressure of 200 mmHg, subsequently 150 ml of acrylic resin (methyl-methacrylate) was injected (Acrifix 2R0190, Evonik Performance Materials GmbH, Darmstadt, Germany), which contained red color agent (So-Strong red color tint, Smooth-on, Inc. Easton, United States). Maceration was carried out in 2–4% potassium-hydroxide solution for a period of 8–14 days at 60–70 °C. Arteries with a minimum diameter of 200 μm were stained, the course of the blood vessels with their relation to adjacent anatomical structures and anastomosis between greater palatine, lesser palatine, and nasopalatine arteries were evaluated macroscopically.
Latex milk injection
This method was used on the cadavers which were donated to the Department of Anatomy, Semmelweis University, Budapest, Hungary, and Department of Anatomy of the Medical University of Graz, Austria, to study the course of blood vessels in relation to soft tissues, used in combination with a layer-by-layer dissection protocol. The ECAs were rinsed with saline solution/PBS under the pressure of 200 mmHg and then perfusion of Thiel’s solution via the ECA was performed. This procedure was executed without detectable odor and resulted in life-like flexibility of body parts, excellent color preservation of muscle and vasculature, as well as superior antimicrobial preservation of cadavers. Following perfusion with Thiel’s solution, the arteries were subsequently flushed with PBS. As the next step, the vessels were filled with red/orange colored latex (Creato Latexmilch, Zitzmann Zentrale, Baden, Germany) containing red color agent (So-Strong red color tint, Smooth-on, Inc. Easton, USA) through the ECA. In 20–30 min, the latex was solidified, and in order to have a proper embalming, a further 3-month fixation period followed. During this period, the specimens were kept in a container filled with Thiel’s solution. Following the fixation period, dissection was carried out under × 2.5 magnification and using Nr. 15 and Nr. 15C surgical blades, the mucosa was elevated; the stained arteries were dissected in each layer and the course of vessels with their anastomosis were macroscopically studied.
Results
Course of the greater palatine artery was clearly presented by applying corrosion casting and latex milk injection techniques; the previous showing the complete mapping of blood vessels along with osseous surroundings, the latter allowing for layer-by-layer dissection and demonstrating soft tissue environment.
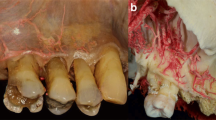
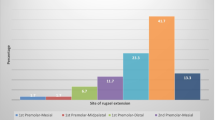
Major- and secondary branches of the GPA and its relation to the palatine spine, different anastomoses with NPA and LPA as well as with contralateral branches of the GPA were recorded (Figs. 1 and 2). Another important record of patients with an edentulous upper jaw revealed that due to the resorption of the bone, the GPA developed a curvy pathway especially at the area of the molars-premolars (Fig. 3). Also, some penetrating intraosseous branches at the premolar-canine area were observed (Fig. 4). The blood supply around the maxillary tuberosity was also presented. As soon as the greater palatine artery emerges out from the greater palatine foramen, it sends one to two branches toward the tuberosity and also the lesser palatine artery sends one to two branches forming anastomoses at this area (Fig. 5). The abovementioned findings are summarized in Fig. 6, which clearly demonstrates the complexity of palatal blood supply.
The course of the greater palatine artery (GPA) and anastomoses between GPA and nasopalatine artery (NPA) shown by corrosion casting. a Overview of palatal blood supply. b Anastomosis between GPA and NPA. c Course of the GPA and major branches. d Course of GPA and anastomosis with NPA. e Course of major- and subbranches of GPA, anastomosis with NPA and between minor branches
Curvy pathway of the greater palatine artery (GPA) in the edentulous areas shown by latex milk injection. a Bilateral view showing curvy pathway of the GPA as well as horizontal shrinkage of the alveolar ridge due to atrophy at an edentulous site. b Normal straight pathway of the GPA. c Curvy pathway of the GPA at the area of the missing upper left molars. d Excessively altered pathway of the GPA in a totally edentulous specimen. e Curvy pathway of the GPA in the upper right premolar area
Intraosseous branches of the greater palatine artery (GPA) shown by latex milk injection. a Intraosseous arteries in the premolar area—bilateral overview. b Intraosseous arteries in the premolar area—left side magnified view. c Intraosseous branch penetrating the palatal cortical bone—right side magnified view
Schematic drawing showing the complexity of palatal blood supply. (a) Curvy greater palatine artery (GPA) pathway in the edentulous area due to the resorption of the bone compared to the dentate side. (b) GPA anastomoses with lesser palatine artery (LPA), nasopalatine artery (NPA) and contralateral GPA subbranches. (c) Penetrating (intraosseous branches) in the premolar area. (d) Tuberal blood supply by GPA and NPA subbranches
At the level of the second molars, the distance of the GPA branches from the level of the crestal bone was 11.3 ± 0.9 mm on average (ranging 10–13 mm). In all the cadavers, high amount of adipose and dense connective tissues were detected together with numerous vessels. In those cadavers showing signs of obesity, increased amount of adipose tissue was observed in the posterior palate compared to cadavers without signs of obesity. Uniform distribution and pathway of anatomical landmarks was observed in all cadavers, no discrepancies were found except for differences related to edentulous/dentate condition of the cadavers.
Discussion
Within the present study, we were able to present comprehensive novel results related to palatal blood supply, which can be integrated into clinical practice when planning and executing palatal surgical interventions. Information available in anatomical literature and textbooks are lacking clinically focused details of the palatal vascular network (intraosseous branches, various anastomoses, which would affect the injection of local anesthetics and incision design; changes in the course of vascular pathways due to loss of dentition and bone resorption). Our study provides a solid anatomical basis on local characteristics of the hard palate and maxillary tuberosity for clinicians who are interested in surgical interventions of the posterior maxilla, such as connective tissue grafting, removal of impacted canines, implant placement, and sinus floor elevation. We demonstrated arterial anastomoses between contralateral and ipsilateral vessels of the palate (Figs. 1 and 2) along with additional vascular mapping of the maxillary tuberosity (Fig. 5). The application of corrosion casting and latex milk injection following Thiel’s fixation simultaneously allowed for blood vessel mapping together with localization of arteries within the palatal mucosa relative to already identified anatomical landmarks. This unique combination of different staining methods has enabled us to demonstrate new types of anastomoses between GPA, NPA, and LPA, or previously unknown intraosseous branches of GPA, alteration of GPA pathway in edentulous sites and tuberal blood supply. Corrosion casting is a widely recognized method in literature for three-dimensional visualization of vascular structures [28]. In the present study, this approach was successfully applied to investigate possible previously unknown pathways of the GPA and its subbranches. Moreover, according to our knowledge, we were the first to utilize latex milk injection [27] to visualize the topographical relation of the GPA branches and subbranches to adjacent tissues within the palatal masticatory mucosa. The palatal mucosa is the most frequently used donor site for connective tissue graft harvesting [8]. Nevertheless, there is only scarce data on the palatal anastomoses possibly influencing intraoperative bleeding and postoperative blood supply of palatal donor sites. SCTGs are usually harvested from an area between the canine and the second molar of the palate by leading a horizontal incision and then the tissue is harvested by either the trapdoor technique [11] or the single incision approach [6]. These approaches, depending on the number, direction, and depth of incisions might afflict a certain risk for arterial damage and a compromised postoperative blood supply. According to our results, several cases of contra- and ipsilateral anastomoses between GPA, NPA, and LPA were demonstrated in the cadavers studied. This might provide an anatomical basis for physiological experiments investigating whether additional submucosal deposition of local anesthetics to contralateral major palatal foramen and/or nasopalatine foramen might be necessary to reduce intraoperative bleeding during palatal surgeries, e.g., SCTG harvesting and sinus floor elevation. Moreover, based on the presence of newly found contralateral anastomoses, we think that in surgeries concerning the palate, also contralateral blood circulation might be affected. Therefore, bilateral connective tissue harvesting may lead to impaired postoperative blood supply and flap necrosis. We too successfully demonstrated the existence of the so far not well-documented intraosseous GPA branches of palatal arteries (Fig. 4). A similar anatomical relation is known in the lower jaw, where nutritive subbranches of the sublingual arteries penetrate the lingual cortical layer of the mandible [31, 32]. Based on anatomical and clinical experiences with lingual intraosseous arteries [32], their palatal counterparts might be responsible for the nutrition of the maxilla and possibly the Schneiderian membrane. Nevertheless, due to their small diameter, they do not pose a significant risk for profuse intraoperative bleeding when compared to lingual nutritive branches. The distribution of the palatal intraosseous branches showed a pattern running parallel to the pathway of GPA.
A study by Reiser et al. [20] suggested that the greater palatine neurovascular bundle lies 17 mm from the gingival margin in patients with high palatal vault, and 12 mm from the gingival margin in patients with medium palatal vault, while in patients with low palatal vault the distance was 7 mm. According to our present findings, in edentulous cadavers due to the resorption of the alveolar ridge, the area for the pathway of the GPA might decrease in apico-coronal and oro-vestibular dimension and the GPA would exhibit a more undulating pathway. We were able to demonstrate that in edentulous cases the GPA with its subbranches became more superficial, which might increase the risk of GPA injury during any type of palatal flap preparation, e.g., connective tissue graft harvesting or during augmentation procedures. Due to this specific curvy outline of arteries, the distance of the GPA from the crest was reduced by 3–4 mm, thus increasing the risk for arterial injury during connective tissue harvesting. Therefore, at edentulous sites, superficial removal of a FGG can be a more secure clinical procedure for connective tissue harvesting as opposed to the single incision or trapdoor techniques.
Apart from the detailed description of the palatal arterial pathways, we were also able to visualize the blood supply of the maxillary tuberosity. The GPA and LPA send one or two minor branches here, which serve for the nutrition of this area. The tuberosity is considered as a possible alternative for the hard palate for SCTG or FGG harvesting applying the distal wedge procedure [33]. The fact that the GPA and LPA branches directed toward the tuberosity are significantly smaller and have lower density compared to palatal arteries might be the reason for prolonged graft revascularization and incorporation, associated with frequent partial, or total necrosis of tuberal FGGs.
Conclusion
In the present study, the pathway and anastomotic pattern of GPA, NPA, and LPA was described and previously unknown intraosseous branches of GPA were also detected. Furthermore, we were able to study the alteration of GPA pathways in edentulous sites, tuberal blood supply, and vertical position of the GPA in relation to the gingival margin. The combination of different staining methods has shed light to findings with relevance to palatal blood supply, offering a powerful tool for the design and execution of surgical interventions involving the hard palate. As a result, the risk of intraoperative bleeding and postoperative wound healing complications related to impaired blood supply can be minimized.
References
Arnold F, West DC (1991) Angiogenesis in wound healing. Pharmacol Ther 52(3):407–422
Klosek SK, Rungruang T (2009) Anatomical study of the greater palatine artery and related structures of the palatal vault: considerations for palate as the subepithelial connective tissue graft donor site. Surg Radiol Anat 31(4):245–250. https://doi.org/10.1007/s00276-008-0432-4
Fu JH, Hasso DG, Yeh CY, Leong DJ, Chan HL, Wang HL (2011) The accuracy of identifying the greater palatine neurovascular bundle: a cadaver study. J Periodontol 82(7):1000–1006. https://doi.org/10.1902/jop.2011.100619
Yu SK, Lee MH, Park BS, Jeon YH, Chung YY, Kim HJ (2014) Topographical relationship of the greater palatine artery and the palatal spine. Significance for periodontal surgery. J Clin Periodontol 41(9):908–913. https://doi.org/10.1111/jcpe.12288
Langer B, Calagna L (1980) The subepithelial connective tissue graft. J Prosthet Dent 44(4):363–367
Hürzeler MB, Weng D. (1999) A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent 19(3):279–87.8)
Benninger B, Andrews K, Carter W (2012) Clinical measurements of hard palate and implications for subepithelial connective tissue grafts with suggestions for palatal nomenclature. J Oral Maxillofac Surg 70(1):149–153. https://doi.org/10.1016/j.joms.2011.03.066
Zuhr O, Bäumer D, Hürzeler M (2014) The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol Suppl 15:S123–S142. https://doi.org/10.1111/jcpe.12185 Review
Sullivan HC, Atkins JH (1968) Free autogenous gingival grafts. 1. Principles of successful grafting. Periodontics 6(1):5–13
Edel A (1974) Clinical evaluation of free connective tissue grafts used to increase the width of keratinised gingiva. J Clin Periodontol 1(4):185–196
Cortellini P, Pini-Prato G, Tonetti M (1995a) Interproximal free gingival grafts after membrane removal in GTR treatment of infrabony defects. A controlled clinical trial indicating improved outcomes. J Periodontol 66:488–493
Tavelli L, Ravidà A, Saleh MHA, Maska B, Del Amo FS, Rasperini G, Wang HL. (2018) Pain perception following epithelialized gingival graft harvesting: a randomized clinical trial. Clin Oral Investig doi: https://doi.org/10.1007/s00784-018-2455-5
Abrams H, Gossett SE, Morgan WJ (1988) A modified flap design in exposing the palatally impacted canine. ASDC J Dent Child 55(4):285–287
Köşger H, Polat HB, Demirer S, Ozdemir H, Ay S (2009) Periodontal healing of marginal flap versus paramarginal flap in palatally impacted canine surgery: a prospective study. J Oral Maxillofac Surg 67(9):1826–1831. https://doi.org/10.1016/j.joms.2009.04.023
Kleinheinz J, Büchter A, Kruse-Lösler B, Weingart D, Joos U (2005) Incision design in implant dentistry based on vascularization of the mucosa. Clin Oral Implants Res 16(5):518–523
Niu L, Wang J, Yu H, Qiu L (2018) New classification of maxillary sinus contours and its relation to sinus floor elevation surgery. Clin Implant Dent Relat Res. https://doi.org/10.1111/cid.12606
Simion M, Fontana F, Rasperini G, Maiorana C (2004) Long-term evaluation of osseointegrated implants placed in sites augmented with sinus floor elevation associated with vertical ridge augmentation: a retrospective study of 38 consecutive implants with 1- to 7-year follow-up. Int J Periodontics Restorative Dent. 24(3):208–221, 2004
Istvan A. Urban, Sascha A. Jovanovic, Jaime L. Lozada (2017) Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Biomed Res Int 2017:4042902. doi: https://doi.org/10.1155/2017/4042902., 2017, 1, 11
Buser D, Chappuis V, Kuchler U, Bornstein MM, Wittneben JG, Buser R, Cavusoglu Y, Belser UC (2013) Long-term stability of early implant placement with contour augmentation. J Dent Res 92(12 Suppl):176S–182S. https://doi.org/10.1177/0022034513504949
Reiser GM, Bruno JF, Mahan PE, Larkin LH (1996) The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 16(2):130–137
Chrcanovic BR, Custódio AL (2010) Anatomical variation in the position of the greater palatine foramen. J Oral Sci 52(1):109–113
Kim DH, Won SY, Bae JH, Jung UW, Park DS, Kim HJ, Hu KS (2014) Topography of the greater palatine artery and the palatal vault for various types of periodontal plastic surgery. Clin Anat 27(4):578–584. https://doi.org/10.1002/ca.22252
Mörmann W, Ciancio SG (1977) Blood supply of human gingiva following periodontal surgery. A fluorescein angiographic study. J Periodontol 48(11):681–692
Hoke JA, Burkes EJ, White JT, Duffy MB, Klitzman B (1994) Blood-flow mapping of oral tissues by laser Doppler flowmetry. Int J Oral Maxillofac Surg 23(5):312–315
Csempesz F, Vág J, Kerémi B, Györfi A, Fazekas A (2000) Blood flow measurements in human oral tissues with laser Doppler flowmetry. Fogorv Sz 93(4):115–120
Molnár E, Molnár B, Lohinai Z, Tóth Z, Benyó Z, Hricisák L, Windisch P, Vág J (2017) Evaluation of laser speckle contrast imaging for the assessment of oral mucosal blood flow following periodontal plastic surgery: an exploratory study. Biomed Res Int 2017:4042902. doi: https://doi.org/10.1155/2017/4042902, 1, 11.
Alvernia JE, Pradilla G, Mertens P, Lanzino G, Tamargo RJ (2010) Latex injection of cadaver heads: technical note. Neurosurgery 67(2 Suppl Operative):362–7. doi: https://doi.org/10.1227/NEU.0b013e3181f8c247
Verli FD, Rossi-Schneider TR, Schneider FL, Yurgel LS, de Souza MA (2007) Vascular corrosion casting technique steps. Scanning 29(3):128–132
Thiel W (1992b) Eine Arterienmasse zur Nachinjektion bei der konservierung ganzer Leichen. Ann Anat 174:197–200
Thiel W (2002) Ergänzung für die Konservierung ganzer Leichen nach W. Thiel. Ann Anat 184:267–269
Liang X, Jacobs R, Lambrichts I, Vandewalle G (2007) Lingual foramina on the mandibular midline revisited: a macroanatomical study. Clin Anat 20(3):246–251
He P, Truong MK, Adeeb N, Tubbs RS, Iwanaga J (2017) Clinical anatomy and surgical significance of the lingual foramina and their canals. Clin Anat 30(2):194–204. https://doi.org/10.1002/ca.22824.
Robinson RE (1966) The distal wedge operation. Periodontics 4(5):256–264
Acknowledgements
The authors would like to express their gratitude to Dr. Gábor Baksa from the Department of Anatomy, Histology and Embryology, Semmelweis University for his precious support. The authors also would like to thank all other co-workers of the Department of Anatomy, Histology and Embryology, and Dr. Ferenc Bartha and Dr. Dániel Palkovics from the Department of Periodontology, Semmelweis University and the Department of Macroscopical and Clinical Anatomy of Graz University for their work and support.
Funding
The work was supported by the Department of Periodontology, Semmelweis University, Budapest, Hungary; Department of Anatomy, Histology and Embryology, Semmelweis University, Budapest, Hungary; Department of Macroscopical and Clinical Anatomy, Medical University of Graz, Graz, Austria.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shahbazi, A., Grimm, A., Feigl, G. et al. Analysis of blood supply in the hard palate and maxillary tuberosity—clinical implications for flap design and soft tissue graft harvesting (a human cadaver study). Clin Oral Invest 23, 1153–1160 (2019). https://doi.org/10.1007/s00784-018-2538-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2538-3