Abstract
Purpose
The aim of the study was to examine the different morphometric variations of the supraorbital and infraorbital foramina of the facial skeleton on human skulls.
Methods
Eighty adult human dry skulls were studied. Measurements were made to analyze the degree of variability in the location of the supraorbital and infraorbital foramina. All measurements were done bilaterally. Variations were evaluated according to gender and side.
Results
There were 54 female and 26 male crania. Almost all mean measurements were longer in males than in females. A statistically significant difference was observed between the left and the right sides in 4 of 10 measurements. When comparing the morphometric measurements between left and right sides of male and female crania, 6 of 22 measurements were statistically higher in men than in women.
Conclusions
The findings suggest that gender should be taken into account when the foramina studied here are to be located. The mean location of the infraorbital nerve was about 6.5 mm inferior to the inferior orbital rim (at the point where one can palpate the zygomatico-maxillary suture), about 25 mm from the midline, and about 43 mm below the supraorbital foramen in the same vertical line. Extra care should be taken during surgical dissection in the superior orbital region especially in the middle aspect of the superior orbital rim. In general, there were changes in measurements between the genders, but the ratios of these measurements with the horizontal and vertical measurements chosen remained the same between the genders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Precise knowledge of the location of reference points in the oral and maxillofacial area provides important data in local anesthesia and maxillofacial and plastic surgical operations [3, 18]. The most certain way to avoid damage to these structures is to know their location. Among the important maxillofacial anatomic entities are the neurovascular bundles of the supraorbital and infraorbital foramina. The cutaneous nerve supply of the maxillofacial region is largely contributed by these nerves. They are frequently encountered in a host of maxillofacial procedures, such as closure of facial wounds, biopsies, scar revisions, cosmetic cutaneous procedures, and also necessary during various endoscopic procedures, which are increasingly being used for cosmetic facial surgery [12, 31]. Excessive dissection and retraction close to such neurovascular bundles can cause scarring, which may lead to entrapment neuropathies and painful neuralgias [9]. Unless the surgeon is aware of the most probable site of exit of regional nerves, injury can occur resulting in bleeding and loss of sensation in corresponding regions of the face [15, 31, 33].
The supraorbital foramen (SOF) is a passage in the frontal bone for the supraorbital artery and nerve; often present as a notch bridged only by fibrous tissue at the junction of the medial and intermediate thirds of the supraorbital margin. It supplies sensation to a large region of the forehead and scalp.
The human infraorbital nerve, the continuation of the maxillary nerve, exits through the infraorbital foramen (IOF). It then breaks into branches that supply the skin of the upper cheek, the mucosa of the maxillary sinus, the maxillary incisor, canine, and premolar teeth and adjacent upper gingivae, the skin and conjunctiva of the inferior eyelid, part of the nose, and the skin and mucosa of the upper lip [27]. It is totally a sensory nerve that requires anesthetizing for operations in dentistry, plastic surgery, and ophthalmology. To apply an infraorbital nerve block, the surgeon needs to palpate the infraorbital rim to identify the IOF and then insert the needle upward to inject local anesthetic [24, 30].
The IOF is situated bilaterally on the maxillary bone, down to the infraorbital border, close to 10 mm, varying from 4 to 12 mm [5]. This foramen is directed inferior medial and in it passes the nerve and vessels which have the same name. It has a relatively big diameter compared to the SOF and can vary on the form and location [4]. This foramen has been used from various reference points, e.g. to determine the morphometric variations of the orbit [20] and variations in size and symmetry [4], as well as, to report the presence of accessory foramens [3, 5, 6]. The location and the possibility of multiplicity of the IOF are important during periorbital surgery.
In this study, several measurements were made on cadaveric skulls to analyze the degree of variability in the location of the SOF and IOF. The locations of the foramina were analyzed relative to the frequently encountered surgical landmarks and according to gender and side.
Materials and methods
Eighty adult human dry skulls of the Laboratory of Dental Anatomy, Department of Morphology, Institute of Biological Sciences, Universidade Federeal de Minas Gerais, Belo Horizonte, Brazil were studied. The collections of crania without mandibles and mandibles were unrelated. As a result, matching between these two collections could not be done, and the data of crania were, therefore, analyzed separately from those of mandibles. The sample consists of urban and rural individuals from the region of the Brazilian state of Minas Gerais who lived in the twentieth century. There was no data about the death age of the humans.
According to Ferembach et al. [13], the determination of gender using the skull is based on 17 primarily morphological characteristics. Five traits could be attributed with a probability of 70–80% [14] and were regarded as sufficiently reliable: the glabella, arcus superciliaris, processus mastoideus, crista supramastoidea, and the overall impression of the mandible. By combining these five traits in the analysis, the gender of approximately 91% of the skulls could be correctly determined [14]. These traits are usually more pronounced and robust in males. According to other authors [1], robust supraorbital ridge and occipital protuberance with a long and broad mastoid process suggest male cranium. The gender determination of the crania in the present study was performed according to these criteria observed by these authors [1, 14], except for the mandible, that is not the purpose of the present study. To avoid bias from one observer, two investigators examined all the crania separately in the first step. A meeting was then arranged between the investigators to make a decision on conflicting data.
All measurements were done bilaterally and performed with a stainless steel metric digital caliper with 0.01 mm precision. Millimeter rulers and specimeter (0.1 mm precision) were also utilized.
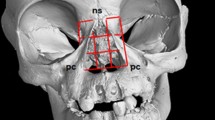
The relative position of the SOF was analyzed with measurements made from his medial wall to the nasal skeletal midline (SOF-NSM), from his lateral wall to the temporal crest of the frontal bone (SOF-TCFB) (both perpendicular to the midline of the face), and from his superior wall to the superior wall of the IOF (SOF-IOF) (parallel to the midline of the face). The identification between supraorbital foramen and notch (SON) was made (Fig. 1).
ANS anterior nasal spine, ANS–IOF–HP angle between the line passing the anterior nasal spine and the infraorbital foramen and the horizontal plane, IOF infraorbital foramen, IOR inferior orbital rim, MSM maxillary skeletal midline, NSM nasal skeletal midline, PA piriformis aperture, SOF supraorbital foramen, SON supraorbital notch, TCFB temporal crest of the frontal bone, ZMS zygomaticomaxillary suture at the level of the inferior orbital rim
The relative position of the IOF was analyzed with measurements made from his superior wall to the inferior orbital rim (IOF-IOR), from his medial wall to the maxillary skeletal midline (IOF-MSM) (both parallel to the midline of the face), from his medial wall to the lateral rim of the piriformis aperture (IOF-PA) (perpendicular to the facial midline), from his medial-inferior wall to the anterior nasal spine (IOF-ANS), and from his superior wall to the zygomaticomaxillary suture at the level of the inferior orbital rim (IOF-ZMS). His medial–lateral width was also measured. The relative vertical position of the IOF in relation with the SOF was analyzed (medial, lateral, coincident).
The angle between the line passing the anterior nasal spine and the infraorbital foramen and the horizontal plane (ANS–IOF–HP) was evaluated, and calculated on digital photographs using the VistaMetrix® software (SkillCrest, Version 1.36.0, 2009). The middle facial third height (MFTH) (distance from the anterior nasal spine to the Nasion) and the largest width of the piriformis aperture (PA width) were measured.
A ratio was made between six measurements (IOF-PA, IOF-MSM, IOF-ANS, SOF-NSM, SOF-TCFB, and PA width) and a chosen standard horizontal measurement (distance between the left and right frontozygomatic sutures, in the medial face of the orbital wall—FZS-FZS). Similarly, a ratio was made between four measures (IOF-ANS, IOF-IOR, SOF-IOF, and ANS-IOF-HP) and a chosen standard vertical measurement (MFTH). These ratios were made considering the right and left sides separately. A total of 38 ratios were analyzed. The aim was to determine whether the possible variations of measurements between genders could have been just a ratio variation.
All measurements were carried out by B.R.C. The information was tabulated and from these measurements means and standard deviations (mean ± SD) were calculated. Basic descriptive statistics were employed to analyze the data obtained using standard software (Excel®, Microsoft Corp.). The mean, standard deviation, minimum and maximum for each of the measurements were assessed. Variations were evaluated according to gender and side. Kolmogorov–Smirnov test was performed to evaluate the normal distribution of the morphometric variables. Paired t test and Wilcoxon test, when indicated, were performed to compare each of the morphometric variables between the left and right side of the skull. Student’s t test and Mann–Whitney test, when indicated, were performed to compare the morphometric variables in relation to gender. Statistical differences were considered when the P value was less than 0.05. All analysis was performed using SPSS version 17.0.
Results
There were 54 female and 26 male crania according to the standard criteria used in forensic medicine. When measurements of the foramina of both sides are considered, there are 160 SOF and 160 IOF (52 foramina in male and 108 in female crania). The data concerning these measurements are in Table 1. All mean values except one (the angle ANS–IOF–HP) were higher in male than in female skulls.
The comparison between the measurements of the right and left foramina are summarized in Table 2. A statistically significant difference was observed between the left and the right sides of the distances SOF-NSM (P = 0.012), SOF-TCFB (P < 0.001), IOF-MSM (P = 0.003), and the angle ANS–IOF–HP (P < 0.001). No significant difference was found between the left and right sides in the other measurements.
The comparison between the measurements of right and left side of male and female crania are summarized in Table 3. The measurements SOF-NSM right side (P = 0.012), IOF-MSM right (P = 0.007) and left side (P = 0.001), IOF-PA left side (P = 0.011), IOF-ANS right (P = 0.001) and left side (P < 0.001) were statistically higher in male crania than in female crania.
The IOF was on the sagittal plane passing through the SOF in 52.50% (n = 84) of the cases, lateral to the plane in 28.75% (n = 46), and medial in 18.75% (n = 30). The SOF was present in 52.50% (n = 84) and the SON in 47.50% (n = 76). IOF was found in all crania. Single IOF was seen in all cases. There were 29 cases of double SOF (18.13%) and 2 cases of triple SOF (1.25%).
The study of proportions showed statistically significant differences in only three ratios between male and female crania: right (P = 0.027) and left IOF-ANS/MFTH (P = 0.008), and left ANS-IOF-HP/MFTH (P = 0.010).
Discussion
The frequency of occurrence of SOF or SON varies in different populations. In the present study, 47.50% of the supraorbital foramina were in fact notches, not foramen. This is inconsistent with the previous reports that demonstrated the higher incidence of the supraorbital notch than foramen, ranging from 69.9 to 92.5% [3, 7, 11, 12, 23, 31]. Other studies have reported that North East Asians and North Americans from an Arctic region [16], Mexicans [6] and Chinese [10] showed a higher frequency of SOF than other populations. The presence of a foramen rather than a notch implies that the supraorbital neurovascular bundle is relatively fixed in position and therefore at a greater risk during surgical dissection, as during retraction it is more likely to be stretched. Therefore, in populations with a greater incidence of supraorbital foramina, extra care has to be exercised during reflection of scalp flaps [10].
Comparison of the mean distances of the SOF from the midline in studies across various ethnic groups showed that the difference in measurement of this parameter was within 2–4 mm [2, 3, 11, 12, 15]. The comparison of the mean distances of the IOF from the midline in these same series yielded similar results. From a surgical viewpoint, this degree of variation may not be significant. However, the distances SOF-NSM and SOF-TCFB showed greater variation than the IOF-MSM in the present study, showing that the location of SOF is more subject to variations in position than the IOF (Table 1).
Our results showed that the mean distances from the SOF to midline were 26.98 ± 4.29 mm. Furthermore, we also observed that this distance of female crania (26.45 ± 3.66 mm) appeared to be smaller relative to those of male crania (28.06 ± 5.24 mm). The similar finding that this distance in females was shorter has been previously reported [12]. Previous studies have shown poor symmetry between sides [33]. Examples of sexual and racial osteologic differences are fairly common [17]. Thus, it is worth noting that gender and side can significantly affect these parameters. Other mean distances were also higher in male than in female crania, as the mean distances SOF-IOF, IOF-MSM, IOF-PA, and the IOF-ANS. The mean distances SOF-TCFB, IOF-IOR, IOF-ZMS, and IOF width were almost equal between the genders, although always showing a little higher distance in male crania (Table 1). Thus, the present findings suggest that gender should be taken into account when the SOF and the IOF are to be located, as the distances may be longer in males than in females. However, when considering mean measurements statistically different between men and women (Table 3), it was identified that only the measures left IOF-PA (P = 0.011), right (P = 0.007) and left IOF-MSM (P = 0.001), right (P = 0.001) and left IOF-ANS (P < 0.001), and right SOF-NSM (P = 0.012) were higher in men than in women. Sexual dimorphism is a well-known phenomenon in human crania, being estimated by Pfitzner in 1901 [25] that the head breadth of female subjects was 96% of that in male subjects. This may partially explain these observed larger distances. Only the angle between the line passing the ANS and the IOF and the HP had the mean value a little higher in female crania in comparison with male crania (31.98 vs. 30.57). However, only 3 of 38 ratios were statistically significant between male and female skulls in the present study, meaning that in general there were changes in measurements between the genders, but the ratios of these measurements with the horizontal and vertical measurements chosen remained the same between the genders. It is noteworthy that both the left and right IOF-ANS/MFTH proportions showed statistically significant differences between the genders, meaning that the measurement IOF-ANS is actually greater in male than in female skulls.
Palpating the SON alone is not sufficient in locating the supraorbital neurovascular bundles in all cases, and it is difficult intraoperatively to exactly identify the midline of the skull [12, 15]. The temporal crest may be a better landmark for intraoperative localization of the supraorbital nerve [12] and therapeutic blockade of supraorbital nerves in migraine patients [9]. Therefore, the use of the 23.57 mm measurement from the temporal crest of the frontal bone may be a better landmark for performing a coronal approach in Brazilians (Table 1).
The IOF was observed in every specimen from our collection. A number of review articles on the surgical anatomy of the orbit describe the IOF as lying 4–5 mm below the inferior margin of the orbit [17, 29, 35], whereas others describe this distance as being greater than 10 mm [32, 35]. Such disparity may be partially explained by the use of information obtained from old anatomy texts [17, 32, 35] or studies of dried human skulls [29], which often did not provide a description of which reference point on the inferior orbital rim was used to determine the distance between it and the IOF. Furthermore, the objectives of the prior studies were not focused on the infraorbital anatomy, but rather on the anatomy of the orbit. There was also no significant difference between the sexes and the sides for this measurement (IOF-IOR) in the present study, and the mean distance found was 6.41 (±1.69).
The closest estimation of the location of the IOF should be used when planning regional nerve blockade. One study suggested a technique that involves infiltrating an anesthetic solution in an area defined by dropping a vertical line from the palpable supraorbital notch to about 10–15 mm below the inferior orbital rim [24]. In another transcutaneous approach, a point of injection medial to the upper nasolabial groove, a few millimeters lateral to the alar groove and 4–7 mm below the inferior orbital rim, was described [36]. According to the results of Aziz et al. [3], it may be more effective to infiltrate an anesthetic solution in the area that is (1) 24–29 mm lateral to the facial midline and in a line perpendicular to the facial midline, (2) about 8 mm below the infraorbital rim, and (3) in the same vertical plane as the first premolar tooth. This technique may be more reliable in the 50% of cases in which the supraorbital notch and the infraorbital nerve are not in the same vertical plane. As per the measurements in this study, the best site for local anesthetic block for the infraorbital nerve would be about 6.5 mm inferior to the inferior orbital rim (at the point where one can palpate the zygomatico-maxillary suture), about 25 mm from the midline, and about 43 mm below the SON/F in the same vertical line.
The average length of the line from the SOF to the IOF was 45.6 mm in one study [11] and 44.95 ± 2.96 in another [2], a value slightly higher than the one found in this study (42.92 mm). Our finding is very similar to the measurements found by Aziz et al. [3], with mean values from 42.2 to 43.3 mm.
As in the study of Agthong et al. [1], we decided to measure the angle between the line passing the ANS and the IOF and HP. According to these authors, this angle was measured since the distance from this foramen to midline is likely to be affected by the anatomy of nasal bones and cartilages, which varies among individuals and races. The anterior nasal spine can be located in living subjects, and its position is not affected by the anatomy of nose, thereby making the data derived from this method of measurement more applicable to clinical settings. The angle measured from the line passing the ANS and the IOF to horizontal line may improve the accuracy of determination of the location of this foramen in clinical situations. Agthong et al. [1] found a mean angle of 25.1° ± 0.4° on the right side and 26.8° ± 0.4° on the left side. We found higher values; 30.54° ± 5.06° on the right and 31.98° ± 5.02° on the left side. Agthong et al. [1] found 7.8 and 8.0 mm (right and left sides, respectively) as the mean IOF-IOR distance, and in the present study the same mean distances were 6.30 and 6.52 mm. As the mean angle was lower and the mean distance IOF-IOR was higher in the present study than in the study of Agthong et al. [1], it might be assumed that the IOF is positioned in a higher location in relation to the middle facial third in Brazilians than in Thais, if Agthong et al. [1] had measured the MFTH, as we did.
A statistically significant difference was observed between the left and the right sides of the distances SOF-NSM (P = 0.012), SOF-TCFB (P < 0.001), IOF-MSM (P = 0.003), and the angle ANS–IOF–HP (P < 0.001) in the present study. Three (SOF-NSM, SOF-TCFB, and IOF-MSM) of these four measurements with significant difference between the sides show that there may have been great variability in the positions of IOF and SOF in relation to the facial midline.
Aziz et al. [3] found in 50% of the cases that the IOF is situated in the same vertical plane as the SOF, with 36.4% observed by Chung et al. [11], and with 52.50% in this study. The only other relation encountered by Chung et al. [11] was the IOF lateral to the plane of SOF. They did not find a medial relationship, as found in the present study (18.75%). This locational relationship would be helpful clinically to determine the location of the IOF, by palpation of the supraorbital notch.
Single IOF was seen in all cases in the present study; there were 29 cases of double SOF (18.13%) and 2 cases of triple SOF (1.25%). Surgeons should realize that multiple foramina may exist in a minority of the patients, and injury to any branch can result in a sensory deficit [3]. Multiple SON/F and IOF have been found in various frequencies among racial groups [3, 6, 26]. When a surgeon makes an attempt to infiltrate these nerves, the anesthesia will not be sufficient if there is an accessory nerve [22]. Double and triple IOF, or accessory foramina, were reported as 2.2–18.2 and 0.5–1.28%, respectively, in several studies [3, 6, 8, 19, 21, 26]. The accessory IOF was stated to be superior and medial to the main foramen in 79.6% of specimens with single accessory foramen [8].
Conclusions
All these findings are important for performing local nerve block and surgery in the forehead and the periorbital regions in order to avoid the neurovascular structures passing through these two foramina. As per the measurements in this study, the best site for local anesthetic block for the infraorbital nerve would be about 6.5 mm inferior to the inferior orbital rim (at the point where one can palpate the zygomatico-maxillary suture), about 25 mm from the midline, and about 43 mm below the SON/F in the same vertical line. Extra care should be taken during surgical dissection in the superior orbital region especially in the middle aspect of the superior orbital rim. Some intra-ethnic and interethnic variations in the position of the SOF and IOF nerve may exist, and thus these mean distances found may vary from population to population.
Our findings suggest that gender should be taken into account when the foramina here studied are to be located, as the distances may be longer in males than in females. In general, there were changes in measurements between the genders, but the ratios of these measurements with the horizontal and vertical measurements chosen remained the same between the genders.
References
Agthong S, Huanmanop T, Chentanez V (2005) Anatomical variations of the supraorbital, infraorbital, and mental foramina related to gender and side. J Oral Maxillofac Surg 63:800–804
Apinhasmit W, Chompoopong S, Methathrathip D, Sansuk R, Phetphunphiphat W (2006) Supraorbital notch/foramen, infraorbital foramen and mental foramen in Thais: anthropometric measurements and surgic relevance. J Med Assoc Thai 89:675–682
Aziz SR, Marchena JM, Puran A (2000) Anatomic characteristics of the infraorbital foramen: a cadaver study. J Oral Maxillofac Surg 58:992–996
Berge JK, Bergman RA (2001) Variations in size and in symmetry of foramina of the human skull. Clin Anat 6:406–413
Bergman RA, Thompson SA, Afifi AK, Saadeh FA (1988) Compendium of human anatomic variation: catalog, atlas and world literature. Urban and Schwarzenberg, Baltimore
Berry AC (1975) Factors affecting the incidence of non-metrical skeletal variants. J Anat 120:519–535
Berry AC, Berry RJ (1967) Epigenetic variation in human cranium. J Anat 101:361–379
Canan S, Asim OM, Okan B et al (1999) Anatomic variations of the infraorbital foramen. Ann Plast Surg 43:613–617
Caputi CA, Firetto V (1997) Therapeutic blockade of greater occipital and supraorbital nerves in migraine patients. Headache 37:174–179
Cheng AC, Yuen HK, Lucas PW, Lam DS, So KF (2006) Characterization and localization of the supraorbital and frontal exits of the supraorbital nerve in Chinese: an anatomic study. Ophthal Plast Reconstr Surg 22:209–213
Chung MS, Kim HJ, Kang HS, Chung IH (1995) Locational relationship of the supraorbital notch or foramen and infraorbital and mental foramina in Koreans. Acta Anat (Basel) 154:162–166
Cutright B, Quillopa N, Schubert W (2003) An anthropometric analysis of the key foramina for maxillofacial surgery. J Oral Maxillofac Surg 61:354–357
Ferembach D, Schwidetzky I, Stloukal M (1979) Empfehlungen für die Alters- und Geschlechtsdiagnose am Skelett. Homo 30:1–32
Graw M (2001) Significance of the classical morphological criteria for identifying gender using recent skulls. Forensic Sci Comm 3. http://www.fbi.gov/hq/lab/fsc/backissu/jan2001/graw.htm. Accessed on 23 Mar 2010
Gupta T (2008) Localization of important facial foramina encountered in maxillo-facial surgery. Clin Anat 21:633–640
Hanihara T, Ishida H (2001) Frequency variations of discrete cranial traits in major human populations. IV. Vessel and nerve related variations. J Anat 199:273–287
Hollinshead WH (1982) Anatomy for surgeons, vol 1—The head and neck, 3rd edition edn. Harper and Row, Philadelphia, pp 328–330
Hwang K, Baik SH (1999) Surgical anatomy of Korean adults. J Craniofac Surg 10:129–134
Kadanoff D, Mutafov S, Jordanov J (1970) Über die Hauptöffnungen resp. Incisurae des Gesichtsshadels. Morph Jb 115:102–118
Karakas P, Bozkir MG, Oğuz Ö (2002) Morphometric measurements from various reference points in the orbit of male Caucasians. Surg Radiol Anat 24:358–362
Kazkayasi M, Ergin A, Ersoy M, Bengi O, Tekdemir I, Elhan A (2001) Certain anatomical relations and the precise morphometry of the infraorbital foramen-canal and groove: an anatomical and cephalometric study. Laryngoscope 111:609–614
Kazkayasi M, Ergin A, Ersoy M, Tekdemir I, Elhan A (2003) Microscopic anatomy of the infraorbital canal, nerve, and foramen. Otolaryngol Head Neck Surg 129:692–697
Keskil S, Gozil R, Calgüner E (2003) Common surgical pitfalls in the skull. Surg Neurol 59:228–231
Kleier DJ, Deeg DK, Averbach RE (1983) The extra oral approach to the infraorbital nerve block. J Am Dent Assoc 107:758–760
Krogman WM, Iscan MY (1986) The human skeleton in forensic medicine, 2nd edn. Charles C Thomas, Springfield
Leo JT, Cassell MD, Bergman RA (1995) Variation in human infraorbital nerve, canal and foramen. Ann Anat 177:93–95
Moore KL, Dalley AF II (1999) Clinically oriented anatomy, 4th edn. Lippincott Williams & Wilkins, Philadelphia, p 861
Ochs MW, Buckley M (1993) Anatomy of the orbit. Oral Maxillofac Surg Clin North Am 5:419–429
Rontal E, Rontal M, Guilford FT (1979) Surgical anatomy of the orbit. Ann Otol Rhinol Laryngol 88:382–386
Salam GA (2004) Regional anesthesia for office procedures. Part I. Head and neck surgeries. Am Fam Physician 69:585–590
Saylam C, Ozer MA, Ozek C, Gurler T (2003) Anatomical variations of the frontal and supraorbital transcranial passages. J Craniofac Surg 14:10–12
Shapiro H (1954) Maxillofacial Anatomy. Lippincott Williams & Wilkins, Philadelphia, pp 119–121
Webster RC, Guant JM, Hamdan US, Fuleihan NS, Giandello PR, Smith RC (1986) Supraorbital and supratrochlear notches and foramina: anatomical variations and surgical relevance. Laryngoscope 96:311–315
Weisman RA (1988) Surgical anatomy of the orbit. Otolaryngol Clin North Am 21:1–12
Whitnall SE (1932) The Anatomy of the human orbit. Oxford University Press, New York, pp 14–22
Zide BM, Swift R (1998) How to block and tackle the face. Plast Reconstr Surg 101:840–851
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chrcanovic, B.R., Abreu, M.H.N.G. & Custódio, A.L.N. A morphometric analysis of supraorbital and infraorbital foramina relative to surgical landmarks. Surg Radiol Anat 33, 329–335 (2011). https://doi.org/10.1007/s00276-010-0698-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-010-0698-1