Abstract
We aimed to make first demonstration of the course and branching pattern of deep branch of the radial nerve (DBRN) in relation to the supinator muscle in the forearms of fetuses and make morphological measurements in both fetuses and adults. We carried out dissection on 80 radial nerves from 20 adult cadavers (16 males and 4 females), ranging from 30 to 56 years old and 20 formalin-fixed, spontaneously aborted fetuses (10 males and 10 females) without detectable malformations, ranging from 20 to 37 weeks of gestation. There were three different branching patterns of the DBRN in fetuses. It divided its terminal branches at entrance of the supinator in 2 (5%), after entry of the supinator in 4 (10%) and after the supinator in 34 (85%) forearms. The course was bilaterally same in fetuses. Dividing pattern at the entrance of the supinator was not seen in adults. Only 4 (10%) were seen at after entering to the supinator and 36 (90%) were seen at after the supinator. We saw in fetuses neither fibrous band deep from the extensor carpi radialis longus nor upper border of the supinator. We assume that these fibrous structures appear after birth, perhaps favored by physical exercise, such as repeated pronation–supination movements. We think that it is one of the reasons why DBRN compression has never been reported in children. This is the first fetal study about the course and branching pattern of the DBRN and there is a constant ratio (mean 4.3) between the measurements of the fetuses and adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radial nerve entrapment syndromes in the forearm, accounting for approximately 0.7% of nontraumatic upper extremity lesions [15], are less common conditions compared with median and ulnar nerve entrapment syndromes. If true frequencies could be measured, deep branch of the radial nerve (DBRN), also known as posterior interosseous nerve (PIN), is probably the most common of these. PIN is often used in the literature instead of DBRN, despite it corresponds only to the distal part of DBRN. This confusion comes from an abuse of language. It enters the radial tunnel after leaving from the radial nerve and could be related with two entrapment syndromes, radial tunnel syndrome (RTS) and posterior interosseous nerve syndrome (PINS).
Radial tunnel is defined as a space created by structures surrounding the radial nerve and DBRN that expands through the proximal forearm over a 5 cm starting at the humeroradial joint and past proximal edge of the supinator muscle [23]. The anterior capsule of the humeroradial joint together with the deep layer of the supinator muscle form the floor of the tunnel; the fibrous adherences between brachialis and brachioradialis muscles in front of the radial head, the medial edge of extensor carpi radialis brevis muscle (ECRB), and the superficial layer of the supinator muscle form the roof of the tunnel; brachioradialis and extensor carpi radialis longus (ECRL) muscles constitute the anterolateral wall; and the medial wall includes the tendon of biceps resting on brachialis muscle [21].
There is no clear distinction in the literature between two syndromes because of the same clinical findings such as pain in the forearm and marked weakness of extensors of fingers or wrist. The hallmark of RTS is pain over radial proximal forearm with little or no motor weakness. Contrary to this, PINS shows loss of motor function or even complete palsy of one or more muscle innervated by the DBRN. Patients with the PINS may have pain but this is not the main symptom [7].
Many authors studied DBRN to identify the causes of the compression at the proximal forearm in adults. Cravens and Kline [3] reported the incidence of PINS was 19% in their study containing 170 patients with radial nerve disorders. Kalb et al. [8] also reported PINS incidence was less than 10% in 111 patients with problems related to the radial nerve in the proximal forearm. Vrieling et al. [27] reported that in 25% of patients PINS is caused by a trauma, in 15% the syndrome is iatrogenic, and in the remaining 60%, the disorder develops spontaneously. The ‘spontaneous’ PINS is most frequently caused by an entrapment at the level of the arcade of Frohse, the part where the nerve enters the supinator muscle [3, 6, 27]. In addition to the arcade of Frohse there are some rare compression sites including adhesions between the brachialis and brachioradialis muscles, the edge of the ECRB [28], fibrous bands associated with the supinator muscle, a capsula-tendon-aponeurosis group located on the anterior aspect of both the humeroradial joint and the radial head, and lateral branches of the recurrent radial artery termed the “leash of Henry” [2, 4, 21]. It is most likely caused by a combination of anatomical anomalies and combined with repetitive pronation–supination movements of the forearm [8, 24, 27].
The aim of the study was to make first demonstration of the course of the deep branch of the radial nerve in fetus elbow and its branching pattern according to the supinator muscle and make morphological measurements in both fetuses and adults for comparison.
Materials and methods
We studied 40 radial nerves from 20 formalin-fixed, spontaneously aborted fetuses (10 males and 10 females) without detectable malformations, ranging from 20 to 37 weeks of gestation (10 of 20 fetuses older than 30 weeks of gestation). The fetuses were obtained from the pathology department and dissected at anatomy department of Gulhane Military Medical Academy.
We carried out dissection on 40 upper extremity from 20 formalin-fixed adult cadavers (16 males and 4 females), ranging from 30 to 56 years old (average 43). The cadavers were dissected at the anatomy departments of Gulhane Military Medical Academy, Hacettepe and Istanbul University School of Medicine.
We used Carl–Zeiss OPMI1-FR surgical microscope for the dissections. Using a longitudinal approach, the radial nerve was found in the groove between the brachialis and brachioradialis muscles. The DBRN was followed after it left the radial nerve. After removal of the brachioradialis, ECRL and ECRB muscles, supinator muscle was exposed and cut obliquely to observe the course and branching pattern of the DBRN to its terminal branches. We observed branching pattern of the DBRN to its terminal branches according to the relationship with the supinator muscle and measured following distances by a digital caliper for comparing them with the previous studies; D1: the length of the radial nerve from the point of piercing the lateral intermuscular septum to the humeroradial joint line, D2: the length of DBRN from the point of branching from the radial nerve to the humeroradial joint line, D3: the length of the DBRN from humeroradial joint line to the superior edge of the supinator muscle, D4: the length of the DBRN from humeroradial joint line to the inferior edge of the supinator muscle, D5: entire length of the radius from humeroradial joint line to the radial styloid process. Schematic illustration of the measured distances is seen in Fig. 1. We also calculated the ratio between each of the adult and fetal measurements. We used only values of 10 fetuses, older than 30 weeks of gestation for measurements and calculations.
Our methods of data analysis included using an SPSS program for descriptive statistical analysis and an independent t test, which was statistically significant at P < 0.05.
Results
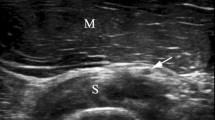
In fetuses, superficial branch of the radial nerve was observed in its normal course at the forearm. DBRN gave a branch to the extensor carpi radialis brevis muscle before entering the arcade of Frohse and continued below the supinator muscle. There were also two minor motor branches to the supinator muscle, a medial and a lateral, branching from DBRN originating above the supinator muscle. There were three different branching patterns of the DBRN to its terminal branches in fetuses. DBRN divided into its terminal branches proximally to the superior edge of the supinator in 2 (5%) forearms, after entering into the supinator in 4 (10%) forearms (Fig. 2) and distal to the inferior edge of the supinator in 34 (85%) forearms. The course was bilaterally same in all fetuses.
Terminal muscular branching pattern in adults, which includes all the muscles on the radial side and dorsal surface of the forearm, excepting the Anconæus, Brachioradialis, ECRL, ECRB and Supinator, proximally to the superior edge of the supinator was not seen. Only 4 (10%), 2 left and 2 rights, were seen at after entering into the supinator and 36 (90%) were seen at distal to the inferior edge of the supinator (Fig. 3).
The course and branching pattern of the DBRN above the arcade of Frohse in forearm of the adult. Dbrn Deep branch of the radial nerve, Sb superficial branch of the radial nerve, sm supinator muscle, asterisks nerves to the supinator muscle, Nb nerve to the brachioradialis muscle, Nel nerve to the extensor carpi radialis longus muscle, Neb nerve to the extensor carpi radialis brevis muscle
Measurement data acquired from both fetuses and adults are given in Table 1. There was no significant statistical difference in any of the measurements between right and left sides of both adults and fetuses (P < 0.05). There was a nearly constant ratio mean 4.30 (minimum 4.18 and maximum 4.47) between each of the adult and fetal measurements in both right and left sides. The ratios which belong to the each measurement are seen Table 2.
Discussion
Although many anatomical and clinical studies have been carried out on the DBRN in adults, there are no data available on the course of the DBRN in fetuses.
Historically, the most important study was designed by Roles and Maudsley [22] with 36 cases and they identified all aspect of RTS especially apparent diagrammatic representation of anatomical structures in radial tunnel. They found three major factors causing compression intraoperatively; first the nerve and its branches were often bound down by adhesions to the tissues overlying the radial head, second the origin of ECRB extended in some cases more medially than is usually described to form a point of possible constriction and third the superficial layer of the supinator with its fibrous edge appeared almost always to compress the PIN.
Rath et al. [20] investigated DBRN relation with the supinator muscle in three segments: segment I, from its origin to its entry into the supinator muscle; segment II, corresponding to its passage through the supinator muscle; and segment III, extending from its exit from the supinator muscle to the origin of the nerves to the lateral epicondylar muscles. Our investigation is similar to their one except we did not investigate segment III and our results show that distribution of terminal muscular branches from DBRN is very similar in both fetuses and adults. We only observed one fetus, in which DBRN branched to its terminal muscular branches proximally to the superior border of the supinator muscle.
There are many precious articles about anatomy of the terminal muscular branches of the DBRN and its entrapment clinics. Portilla Molina et al. [18] studied possible compression sites for DBRN distal to the inferior border of the supinator muscle. Ay et al. [1] measured the distance of the point that DBRN divides into the terminal branches from the inferior border of the supinator muscle. Elgafy et al. [5] stated that terminal branches of PIN formed a six-branched common leash at 1 cm from the distal border of superficial head of the supinator muscle. Moss and Switzer [14] studied the spectrum of clinical presentation of RTS in 15 cases. Lister et al. [12] showed the effect of the therapy on 20 RTS patients.
Beside these studies, which mainly focus on terminal muscular branches of DBRN, there are so many articles in the literature explained relationship between DBRN and the supinator muscle anatomically and clinically. We can compare our results with these papers.
Our adult results show that the length of the radial nerve from the point of piercing the lateral intermuscular septum to the humeroradial joint line, D1, is approximately 9.3 cm. Kirici and Irmak [9] and Prasartritha et al. [19] found same distance 13 and 8.85 cm, respectively. The length of DBRN from the point of branching from the radial nerve to the humeroradial joint line, D2, is approximately 3 cm. Kirici and Irmak [9], Prasartritha et al. [19] and Konjengbam and Elangbam [10] found same distance 1.3, 3.35 and 0.85 cm, respectively. We think that our results are concordant with the result of Prasartritha et al. Difference in D1 and D2 measurements between results of ours and other’s studies is caused by definition of the lateral intermuscular septum and the humeroradial joint line. Thomas et al. [25] reported that the radial nerve bifurcated into the PIN and superficial radial nerve 8.0 ± 1.9 cm distal to the lateral intermuscular septum. Low et al. [13] found that the radial nerve branched into superficial radial nerve and PIN at an average of 1.8 cm below the lateral condyle. Ozkan et al. [16] measured the distance between the lateral intermuscular septum and the site of division of radial nerve into its superficial and deep branches, which is equal to D1 minus D2, was 9.2 cm.
The length of the DBRN from humeroradial joint line to the superior edge of the supinator muscle, D3, is approximately 2.85 cm. Kirici and Irmak [9], Konjengbam and Elangbam [10] and Riffaud et al. [21] reported same distance 2, 2.35 and 2.5 cm, respectively. Thomas et al. [25] reported that the bifurcation of the radial nerve occurred 3.6 ± 0.7 cm proximal to the leading edge of the supinator. Low et al. [13] found that the PIN passed beneath the arcade of Frohse at an average of 3.8 cm below the lateral condyle. Tubbs et al. [26] stated that the PIN entered the supinator muscle at approximately the level of the radial head; mean 6 cm distal to the lateral epicondyle of the humerus. Ozturk et al. [17] measured that the distance between the lateral epicondyle and the superior margin of the supinator muscle was 4.62 cm. Lawton et al. [11] measured the mean length of PIN from radiocapitellar joint line to the branching point in the supinator muscle, which is approximately 2 cm plus D3, was 4.6, 5.3 and 5.7 cm in supination, neutral position and pronation, respectively.
Ozkan et al. [16] measured the length of the PIN from its division to the arcade of Frohse, which is equal to D2 plus D3, was 4.6 cm.
The length of the DBRN from humeroradial joint line to the inferior edge of the supinator muscle, D4, is approximately 6.85 cm. Kirici and Irmak [9] and Konjengbam and Elangbam [10] found same distance 6.2 and 6.53 cm, respectively. Riffaud et al. [21] reported that the average distance between the superior and inferior margins of the supinator muscle was 4.5 cm. Thomas et al. [25] reported that the PIN exited the supinator muscle 3.8 ± 0.9 cm distal to the proximal margin.
We think that the most important measurements for decompression surgery are D3 and D4 because of the most common compression site is the superior edge of the supinator muscle. Our results are concordant with the literature for these measurements.
Entire length of the radius from humeroradial joint line to the radial styloid process, D5, is approximately 23.5 cm. Kirici and Irmak [9] found same distance 22.5 cm. Ozturk et al. [17] measured that the distance between the lateral epicondyle and the radial styloid process was 23.32 cm. Tubbs et al. [26] stated that the exit site from the distal edge of the supinator muscle was also found to be mean 18 cm proximal to the styloid process of the ulna. We added D5 measurement to the study because of the necessity of a bony parameter for comparing fetal and adult results. We found that this measurement was also concordant with the literature.
Since there is no study to compare within the literature; we compared our results of the fetal measurements with the adult ones. We found a nearly constant ratio, mean 4.3 (minimum 4.18 and maximum 4.47), dividing adult value to the fetal one in all of the measurement. This might be interpreted that there is no difference between adults and fetuses according to the morphological measurements.
Branching pattern of the DBRN according to the supinator muscle might not vary the symptoms of both RTS and PINS impressively. If the DBRN branches proximal to the supinator or between superior and inferior border of the supinator, more motor branches might be affected in the case of the compression at the most common site that is arcade of Frohse.
Finally as a conclusion, because of neither fibrous band deep from the ECRL, nor upper border of the supinator was seen in fetuses; we assume that these fibrous structures appear after birth. We think that it is one of the reasons why DBRN compression has never been reported in children. There is a constant ratio (mean 4.3) between the measurements of the fetuses and adults in this the first fetal study about the course and branching pattern of the DBRN. Studying and publishing of the nerve courses in fetus will be helpful for our understanding of comparative anatomy and also an encouraging accelerator for researchers to work on unstudied peripheral nerves.
References
Ay S, Apaydin N, Acar H, Akinci M, Piskin A, Tekdemir I, Elhan A (2005) Anatomic pattern of the terminal branches of posterior interosseous nerve. Clin Anat 18(4):290–295
Barnum M, Mastey RD, Weiss AP et al (1996) Radial tunnel syndrome. Hand Clin 12(4):679–689
Cravens G, Kline DG (1990) Posterior interosseous nerve palsies. Neurosurgery 27:397–402
Dm Dawson, Hallett M, Wilbourn AJ (1999) Entrapment neuropathies. Lippincott-Raven, Philadelphia, pp 4–19
Elgafy H, Ebraheim NA, Rezcallah AT, Yeasting RA (2000) Posterior interosseous nerve terminal branches. Clin Orthop Relat Res 376:242–251
Hashizume H, Nishida K, Nanba Y et al (1996) Non-traumatic paralysis of the posterior interosseous nerve. J Bone Joint Surg Br 78:771–776
Huisstede BM, Miedema HS, van Opstal T et al (2006) Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies. J Peripher Nerv Syst 11(2):101–110
Kalb K, Gruber P, Landsleitner B (2000) Non-traumatically induced paralysis of the ramus profundus nervi radialis. Aspects of a rare disease picture. Handchir Mikrochir Plast Chir 32:26–32
Kirici Y, Irmak MK (2004) Investigation of two possible compression sites of the deep branch of the radial nerve and nerve supply of the extensor carpi radialis brevis muscle. Neurol Med Chir (Tokyo) 44(1):14–18
Konjengbam M, Elangbam J (2004) Radial nerve in the radial tunnel: anatomic sites of entrapment neuropathy. Clin Anat 17(1):21–25
Lawton JN, Cameron-Donaldson M, Blazar PE, Moore JR (2007) Anatomic considerations regarding the posterior interosseous nerve at the elbow. J Should Elb Surg 16(4):502–507
Lister GD, Belsole RB, Kleinert HE (1979) The radial tunnel syndrome. J Hand Surg (Am) 4(1):52–59
Low CK, Chew JT, Mitra AK (1994) A surgical approach to the posterior interosseous branch of the radial nerve through the brachioradialis—a cadaveric study. Singap Med J 35(4):394–396
Moss SH, Switzer HE (1983) Radial tunnel syndrome: a spectrum of clinical presentations. J Hand Surg (Am) 8(4):414–420
Mumenthaler M (1974) Charakteristiche Krankheitsbilder nicht unmittelbar traumatischer peripherer Nervenschaden. Nervenarzt 45:61–66
Ozkan M, Bacakoğlu AK, Gül O, Ekin A, Mağden O (1999) Anatomic study of posterior interosseous nerve in the arcade of Frohse. J Should Elb Surg 8(6):617–620
Ozturk A, Kutlu C, Taskara N et al (2005) Anatomic and morphometric study of the arcade of Frohse in cadavers. Surg Radiol Anat 27(3):171–175
Portilla Molina AE, Bour C, Oberlin C, Nzeusseu A, Vanwijck R (1998) The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. Int Orthop 22(2):102–106
Prasartritha T, Liupolvanish P, Rojanakit A (1993) A study of the posterior interosseous nerve (PIN) and the radial tunnel in 30 Thai cadavers. J Hand Surg (Am) 18(1):107–112
Rath AM, Perez M, Mainguené C, Masquelet AC, Chevrel JP (1993) Anatomic basis of the physiopathology of the epicondylalgias: a study of the deep branch of the radial nerve. Surg Radiol Anat 15(1):15–19
Riffaud L, Morandi X, Godey B et al (1999) Anatomic bases for the compression and neurolysis of the deep branch of the radial nerve in the radial tunnel. Surg Radiol Anat 21:229–233
Roles NC, Maudsley RH (1972) Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br 54(3):499–508
Rosembaum R (1999) Disputed radial tunnel syndrome. Muscle Nerve 22:960–967
Spinner M (1968) The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg (Br) 28:133–137
Thomas SJ, DE Yakin, Parry BR et al (2000) The anatomical relationship between the posterior interosseous nerve and the supinator muscle. J Hand Surg (Am) 25(5):936–941
Tubbs RS, Salter EG, Wellons JC 3rd et al (2006) Superficial surgical landmarks for identifying the posterior interosseous nerve. J Neurosurg 104(5):796–799
Vrieling C, Robinso PH, Geertzen JH (1998) Posterior interosseus nerve syndrome: literature review and report of 14 cases. Eur J Plast Surg 21:196–202
Werner CO (1979) Lateral elbow pain and posterior interosseous nerve entrapment. Acta Ortop Scan Suppl 174:1–62
Acknowledgment
The authors are grateful to Cenk Kilic M.D. for drawing Fig. 1.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tatar, I., Kocabiyik, N., Gayretli, O. et al. The course and branching pattern of the deep branch of the radial nerve in relation to the supinator muscle in fetus elbow. Surg Radiol Anat 31, 591–596 (2009). https://doi.org/10.1007/s00276-009-0487-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-009-0487-x