Abstract
The most widely accepted description of venous anatomy in the transverse foramen involves the presence of one or two veins running along and parallel to the external side of the vertebral artery. For most surgeons, the vertebral artery is surrounded by a rete of veins which is continous with the wide sinusoids which surround the thecal sac (internal vertebral venous plexus). The goal of this study was to ascertain the exact structure of the venous system in the transverse canal by micro dissection and histology. Six spinal segments (C1 to C7) removed from cadavers embalmed using 5% diluted formalin or not and studied with or without injection of colored latex after bilateral catheterization of the internal jugular vein, vertebral vein, common carotid artery, and vertebral artery. An anatomical study was performed by optical microscopy. After fixation and decalcification, tissue specimens were stained using hematoxylin–eosin–safran (HES) and immunocytochemical markers including CD43, CD31, and desmine (specific for vascular endothelium). Findings showed that venous blood in the transverse canal flows through a space formed by the periosteum. There was no evidence of a vein inside the transverse canal. The periosteum spans the space between the transverse processes and gives off fibrous leaflets to the artery thus forming a compartmentalized space lined with vascular endothelium around the artery. The venous system in the transverse canal presents itself as a sinus similar to the intracranial sinus structure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The venous organization and relationship to the vertebral artery in the transverse canal have clinical and surgical implications. This organization is relevant for (a) surgical procedures which involve the transversal canal and its contents and (b) neuroimaging especially for vertebral artery dissection diagnostic. According to classical anatomical descriptions, the cervical venous component of transverse canal is supposed to consist of one or two satellite veins running alongside the vertebral artery. Alternatively, some authors have proposed the presence of a venous plexus around the artery [2, 9]. In a recent study, Lu et al.[9] demonstrated three types of cervical venous organization: single or double veins, venous plexus, and absence of vein. The purpose of this investigation was to ascertain the exact structure of the venous system within the transverse canal by microdissection and histology.
Materials and Methods
To ensure inclusion of the whole transverse canal, cervical spine segments (atlas to C7) were removed from six adult cadavers and studied with injection of colored Latex in four cases and without injection in two cases. Table 1 describes the specimens for this study.
Equipment used included a LEICA® microscope (magnification, 10×, 16×, 25×), an electric hand-piece for bone drilling, and microsurgical instrumentation for dissection. The anterior aspect of the transverse processes of each vertebra (C1 to C7) was burred away in order to open the transverse canal along its full length. Care was taken to preserve and keep the fibrous periosteal sheath intact. Bone drilling was extended a half centimeter internally to the vertebral canal and the same distance externally to expose all collateral veins. Afterwards, exploratory microsurgery was undertaken. The periosteal sheath was opened to allow microscopic examination of venous anatomy in the transverse canal.
The spinal specimens that were removed for histological study included the left transverse processes of vertebras C3 and C4. The left body/disc complex was included since the medial section line passed through the vertebral body. Specimens were fixed in 5% formalin for 2 days and then were decalcified using formic acid (10%), hydrochloric acid (8%), and water (82%) for 3 weeks. After dehydration and inclusion in paraffin, histological sections (thickness, 3 μm) were cut and stained with hematoxylin–eosin–safran(HES). Immunohistochemical labeling was performed using markers specific for vascular endothelium (CD43,CD31, and desmine) to detect vascular structures.
Results
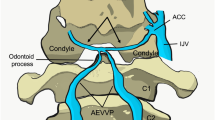
The same vascular anatomy was consistently found on all spinal segments examined in this study. In each case the transverse foramen of the sixth cervical vertebra was the entry point for both the vertebral artery and the main truck of the vertebral vein. Opening of the transverse canal always revealed a tough, fibrous periosteal sheath lining the whole canal. When this sheath was opened, no sign of a satellite vertebral vein was ever observed near the artery. The vertebral artery was in continuous contact with the medial aspect of the sheath. The space surrounding the artery was characterized by the presence of a network of compartments. Colored Latex appeared to circulate freely in this compartmentalized space and always flowed out of this space when opened. Compartmentalization was created by leaflets of conjunctive tissue between the artery and periosteal sheath (Fig. 1). Throughout the course of this venous space, there were metamerically organized collateral vessels arising from the scalenus muscles. A similar collateral system was present on the medial side with the epidural veins. The exploration along the transverse canal within the fibrous periosteal tunnel revealed no differences in the venous organization between inter-foraminal and intra-foraminal regions. Furthermore, no significant difference was found between cervical levels. However, on entrance of the transverse canal (sixth cervical vertebra) transition zones between the vertebral vein and the space around the vertebral artery revealed the presence of a venous plexus. On exit of the transverse canal (first cervical vertebra) the vertebral artery was surrounded by a rich venous plexus. The extension inside the fibrous periosteal tunnel of this transitional plexus was varied in length. In the two cases where a bilateral study was performed on the same spinal segment, significant differences were found in the venous organization between the right and left sides related to the length of the transitional plexus. In the same way, the length of the transitional plexus was varied between all spinal segments examined in this study.
: Anterior view of right transverse canal after bone drilling with white pliant leader running along the vertebral artery. 1 Periosteal sheath 2 Transverse processes after bone drilling 3, 7 Spinal nerves 4 Scalenus muscles 5 Pliant leader 6 Vertebral artery. (Cranial on the left, Caudal on theright, Medial on the top, Lateral on the bottom)
Histological study and immunocytochemical labeling demonstrated that the observed anatomy was not the result of anastomosis between several veins. There was no evidence of a venous wall in the transverse canal (Fig. 2). The best analogy for the periarterial space is a venous sinus. Figure 3 illustrates the findings of microsurgical dissection and histological study.
: Three-dimensional illustration of results. Anterior view of left vertebral artery with transversovertebral sinus. The transversovertebral sinus surrounds the vertebral artery. The sinus and the artery are contained in a periosteal sheath. Made with Blender (http://www.blender.org/).
Discussion
Venous anatomy of the transverse canal was already a controversial topic for anatomists at the end of the nineteenth century. The historical details were presented in the article of Laux et al.[7] where Trolard, Ch. Labbé and Ch. Walter were cited. Trolard stated that venous blood drained through a “transversovertebral venous sinus‘’. However, Ch. Labbé and Ch. Walter proposed a different description involving a venous confluence. In the twentieth century, authors have proposed a variety of descriptions but no one has revived the sinus theory of Trolard. Testut [16] and Rouvière and Delmas [14] described it as a single satellite vertebral vein accompanying the vertebral artery at the cervical level. Paturet [12] added that the satellite vein was always located externally to the artery. Laux et al.[7] have reported sound evidence in favor of the sinus theory proposed by Trolard. This histological study confirmed the existence of a “transverso-vertebral sinus”. Frymoyer et al.[4] described a large continuous venous compartment around the vertebral artery, which is continuous with the venous sinusoids surrounding the nerve roots in the root canals and with the wide sinusoids surrounding the thecal sac (epidural veins).
The periosteum is the first element encountered after opening the transverse canal. It is a tough fibrous sheath bridging from one transverse process to the other and therefore forming a fibrous canal with a constant diameter. This sheath also serves as a vascular wall and is lined internally by venous endothelium. Injections of colored Latex were necessary to distinguish fibrous and vascular elements in the canal.
Histological sections provided definite proof of a sinus venous anatomy. There was no specific labeling of the venous endothelium. However, the periarterial space was the only possible route for venous blood through the transverse canal.
Our results consistently confirmed the conclusions of Jovanovic which stated that the vertebral artery and vein entered together in the transverse canal at the level of the sixth vertebra [6]. Special attention was focused on entrance and exit of the transverse canal, and on the transition zones between the vertebral vein and sinus in the canal. Our findings suggested that this zone could contain a venous plexus. If so, this could account for much of the controversy that has surrounded this topic. Indeed, our findings suggest that the venous organization in the transverse canal is a set of successive venous structures from C1 to C6 (venous plexus, venous sinus, venous plexus, and vein). According to the length of each part, variable anatomic organization could be found. For Lu et al.[9] the venous organization was classified into three types: single or double veins, venous plexus, and absence of vein. These three types were in accordance with our findings. The type “absence of vein”, after microsurgical dissection and histological sections, should confirm the existence of the transversovertebral sinus.
Another intriguing aspect of this study was that the route of both internal carotid arteries and both vertebral arteries involved passage through a sinus structure, i.e., the cavernous sinus for the carotid arteries and the transversovertebral sinus of the vertebral arteries. This organization almost certainly has a physiological importance which remains to be elucidated or is the signature of common embryological process. A variety of mechanisms could come into play. One possibility is that the venous pressure has a cushioning effect on the blood pressure in cerebral arteries. Since the walls of the sinus are rigid and non-expandable, another possibility is that the throbbing artery facilitates drainage by forcing venous blood out at each pulsation. A further anatomical possibility is that in both sinuses there exists a transitional structure between the extracranial and intracranial spaces. In the extracranial spaces the volumes of the arteries and veins are independent of each other and in the intracranial space the sum of the volumes of the arteries and veins are constant at a fixed moment, which is the basis of the Monro Kelly law [15]. A hypothesis about physiological importance of the anatomical arterial–venous conjugation (carotid / cavernous sinus) was presented by Moreira [11]. He believed “...that besides protecting the vascular arterial wall in acute episodes of hypertension, it can also contribute to the mechanism of carotid blood flow”. The same hypothesis might be used to defend the arterial–venous organization in the transverse canal.
According to our findings, venous anatomy in the transverse canal resembles the intracranial venous sinus. Folding dura mater results in the creation of a non-expandable fibrous space lined with vascular endothelium. Attachment to the bone was observed in all cases. An excellent illustration of this arrangement is demonstrated by the crossing of cavernous sinus by the carotid artery at the base of the skull. Thus venous organization in the transverse canal replicates the well-documented and established intracranial venous anatomy [13, 15].
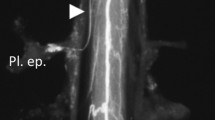
Magnetic resonance imaging and magnetic resonance angiography are sensitive for the detection of the vertebral artery dissection [8]. The semilunar signal hyperintensity in the periphery of an occluded vertebral artery on T1-weighted axial images is usually interpreted as a mural hematoma in the vessel wall. Miaux et al.[10] reported false-positive results of magnetic resonance in the diagnosis of vertebral artery dissection. According to this letter the semilunar signal hyperintensity could be interpreted as a flow-related enhancement in the vertebral venous system that surrounds the suspected dissected vertebral artery. Dumas et al.[3] evaluated the blood flow in the vertebral veins using magnetic resonance angiography. They confirmed that vertebral veins can create flow-related enhancement around the vertebral artery. According to Dumas et al.[3] this flow-related enhancement in the transverse canal is not related to the occlusion of the vertebral artery but related to normal anatomic venous organization. Our findings might help to interpret and understand magnetic resonance studies of the vertebral canal contents. We can suppose that flow-related enhancement around the vertebral artery is related to the existence of the transversovertebral sinus. Indeed the blood flow in a venous sinus is more laminar than in a venous plexus. Flow-related enhancement is created by slow laminar flow in a venous structure [1]. This hypothesis needs to be confirmed by further magnetic resonance studies. According to ours findings, the venous system around the vertebral artery is not the same along the transverse canal and seems to be variable between the right and left side and between individuals. In addition even if the transversovertebral sinus is an anatomical reality, further in vivo studies must be preformed to confirm that this sinus is functional.
Our findings are useful for the treatment of vertebral arteriovenous fistula, vein graft reconstruction of the vertebral artery [5], treatment of atherosclotic, traumatic and neoplasic diseases using transpedicular screw placement. The presence of a venous sinus in the transverse canal is consistent with intraoperative observations. Opening of the periosteal sheath always leads to venous bleeding making hemostasis difficult. Venous bleeding when the transverse canal is opened should be considered as a warning sign that the vertebral artery is in the immediate vicinity.
Conclusion
The traditional view of venous anatomy involving a satellite vein along side the artery in the transverse canal appears to be incorrect. There is no vein in the transverse canal. Venous blood flows through a space that is limited by the periosteum. The periosteum spans the gap between the transverse processes and expands fibrous leaflets to the artery, thus forming a compartmentalized periarterial space lined with vascular endothelium. The vascular anatomy in the transverse canal presents itself as a venous sinus similar to intracranial sinus structures. The transversovertebral sinus appears to be an anatomical reality.
References
Bradley WG Jr, Waluch V (1985) Blood flow: magnetic resonance imaging. Radiology 154:443–450
Chopard RP, de Miranda Neto MH, Lucas GA, et al. (1992) The vertebral artery: its relationship with adjoining tissues in its course intra and inter transverse processes in man. Rev Paul Med 110: 245–250
Dumas JL, Stanescu R, Goldlust D, et al. (1997) Vertebral vein imaging with MR angiography. AJNR Am J Neuroradiol 18:1190–1192
Frymoyer JW (1997) The adult spine. Principles and practice, vol 1. L.-R. Publishers, Philadelphia, pp1062
Iwai Y, Sekhar LN, Goel A., et al (1993) Vein graft replacement of the distal vertebral artery. Acta Neurochir (Wien) 120:81–87
Jovanovic MS (1990) A comparative study of the foramen transversarium of the sixth and seventh cervical vertebrae. Surg Radiol Anat 12:167–172
Laux G, Guerrier Y, Paras C (1949) Sinus veineux vertébro-transversaire. C. R. Ass Anat 36e réunion pp:416–418
Levy C, Laissy JP, Raveau V, et al (1994) Carotid and vertebral artery dissections: three-dimensional time-of-flight MR angiography and MR imaging versus conventional angiography. Radiology 190:97–103
Lu J, Ebraheim NA, Ouyang J, et al (2000) Cervical venous structure in the inter-transverse and intra-transverse foraminal region: an anatomic study. Am J Orthop 29:196–198
Miaux Y, Cognard C, Martin-Duverneuil N, et al (1996) Flow-related enhancement in the vertebral plexus mimicking an intramural hematoma. AJNR Am J Neuroradiol 17:191–192
Moreira MB (1998) Physiological importance of the conjugation of the internal carotid artery and cavernous sinus. Med Hypotheses 50:389–391
Paturet G (1958) Traité d ’Anatomie Humaine. Tome III. Masson, Paris, pp1305
Rhoton A L, Jr (2002) The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery 51:S375–S410
Rouvière H, Delmas A (1973) Anatomie Humaine descriptive, topographique, fonctionnelle. Tome I. Masson, Paris, pp608
Schaller B (2004) Physiology of cerebral venous blood flow: from experimental data in animals to normal function in humans. Brain Res Brain Res Rev 46:243–260
Testut L (1905) Traité d ’Anatomie Humaine. Tome II. Octvae Dion, Paris, pp988
Acknowledgements
The authors would like to thank Bryan Edward Long for his help.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palombi, O., Fuentes, S., Chaffanjon, P. et al. Cervical venous organization in the transverse foramen. Surg Radiol Anat 28, 66–70 (2006). https://doi.org/10.1007/s00276-005-0040-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-005-0040-5