Abstract
Purpose
This study focuses on the following questions: What are the morphological features at the transdural course of radiculomedullary veins? How are these short transdural segments that may harbour pathological arteriovenous shunts connected to the internal vertebral venous plexus? Is the conception of a reflux-impeding mechanism at the transdural segment indispensable and convincing?
Methods
A total of 102 radiculospinal veins were studied microscopically at various levels of the spinal canal using serial paraffin and semi-thin sections. In addition, 26 vessels were investigated microangiographically following orthograde (12) or attempted retrograde (14) opacification of the intradural venous segment with barium sulphate. After paraplast-embedding, contact-microradiographs were taken using high-resolution spectroscopic plates.
Results
At their transdural course, the veins showed narrowing of their lumen accompanied by changes in the vessel wall composition and a tortuous course. Two structurally distinct arrangements of the transdural segment could be identified: A slit type was seen in 60 % of the veins studied and a bulge- or nodular type was seen in 35 % of the veins. In total, 5 % of cases could not be assigned to either one of these types. Reflux to radicular veins from the outside of the dura mater could be produced in 2 out of 14 specimens. The extradural venous plexus, which primarily receives the radicular vein, was composed more frequently of lacunar spaces rather than plexiform blood vessel convolutions. Rare observations were fibrotic, blind ending radiculomedullary veins and continuation of a distinct venous blood vessel after crossing the dura.
Conclusions
Reflux from the epidural plexus to radicular veins is not reliably stopped at the dural level and possibly physiological. Different arrangements of the transdural course of the veins appear to be at least appropriate to modulate flow. The purpose for two different types of radicular vein exit is unclear. The clinical impact of disturbed reflux-control is uncertain, which is in stark contrast to the severe consequences resulting from dural arteriovenous shunts. The functional role of the probably predominant epidural venous plexus for the spinal cord blood circulation remains poorly understood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The experiences gained by selective spinal angiography in the late seventies and eighties of the past century instructed clinicians that the superficial spinal cord draining veins may play an important pathogenetic role in vascular diseases of the spinal cord, particularly in spinal arteriovenous malformations (SAVM) and different forms of spinal arteriovenous fistulae (SAVF), mainly the dural ones (SDAVF) [1, 2]. In these SDAVF, a spinal meningeal artery communicates without flow restriction with the dural segment of a radiculomedullary vein. The resulting arterialisation of spinal cord veins leads to severe impairment of spinal cord blood circulation without any participation of the spinal cord supplying arteries. Parenchymal damage developing in the long term had been described as ‘subacute necrotizing myelitis’. The disease was already known as ‘Foix-Alajouanine disease’ since 1926 [3, 4]. But the distinct pathogenetical features could only be explained and understood after Kendall and Logue [1] had elucidated this special type of dural AV shunt [4, 5].
‘The upsurge of interest in spinal veins’ [6] stimulated by these insights created the expectation that chronic impairment of spinal venous drainage alone could be the cause of myelopathic conditions of vascular origin [2, 5–8].
Two assumptions have played a major role in the discussion of aetiological conceptions. The first one is the idea that contrary to the high numbers of counted radicular veins only a small number definitely carry the venous return from the spinal cord [6].
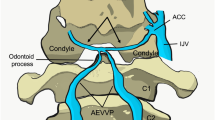
The second one is the assumed presence of valves in the radiculomedullary veins. This was based on the observation that retrograde filling of intradural radicular veins from the outside of the dura mater in autopsy studies was not successful [9–12]. Moreover, the argument that some mechanism or anatomical arrangement can prevent reflux from the internal epidural system (Batsons plexus) to the intradural spinal cord blood circulation in case of an increase in peripheral venous pressure was convincing (Fig. 1). Both outlined conditions would make venous return from the spinal cord vulnerable and unexplained myelopathies might be based on this pathogenesis.
Superficial spinal cord veins and radiculomedullary veins crossing the dura mater. X-ray of a contrast-injected human spinal cord specimen in anteroposterior view. Upper thoracic region. The anterior median venous trunk communicates with the internal vertebral venous plexus through radiculomedullary veins at different levels (arrowhead). These veins commonly follow a nerve root before they exit and join the lacunar venous spaces of the internal vertebral venous plexus Pl. ep Epidural plexus
We have shared these opinions and therefore inspired detailed macroscopic, microscopic and microangiographic [13–15] examinations of the transdural portions of radiculomedullary veins [13–15].
This article includes results of the doctoral dissertation in Medicine about the assumed reflux-impeding mechanisms of the transdural portion of spinal cord draining radicular veins carried out approximately 25 years ago [13]. Some of the results obtained at that time are worth being communicated in a more detailed manner and receiving greater attention. Others have to be confronted with new results from post-mortem investigations on the internal vertebral venous plexus using a thorough preparation of the cadavers before injecting a modern polymer [16, 17]. The obtained results suggest that reflux might be a physiological phenomenon [17]. We felt motivated to reconsider the clinical impact of the dural segment of radicular veins aside from a dural arteriovenous shunt and to raise the question whether the conception of a reflux-impeding mechanism at the dural exit of radicular veins is both indispensable and convincing.
Spinal cord blood circulation in general and especially venous return from the spinal cord is a topic in which only a few people were interested for the past 2 decades. But the challenge to discriminate between variation and clinically relevant pathologic findings might increase, thanks to considerably improved imaging of the spinal cord veins by magnetic resonance and flat-panel angiographic techniques [18, 19].
Material and Methods
In all, 104 specimens were obtained from 20 unselected autopsy cases between 1986 and 1988. These specimens included the dural exit of spinal radicular veins at different levels of the spinal canal.
A total of 19 specimens were excluded because of artefacts or erroneous preparation of arterial blood vessels. The remaining 85 veins were examined microscopically in serial histological sections using conventional formalin fixation, paraffin embedding and haematoxylin–eosin or elastica van Gieson staining. In a few cases, 3.2 % phosphate buffered glutaraldehyde fixation was used followed by epoxy resin embedding, semi-thin sectioning (0.5–1 µm in thickness) and toluidine as well as paraphenylenediamine staining.
In addition, 26 different specimens were used for microangiographic injections, followed by conventional histopathological evaluation as indicated earlier. In 12 of these specimens, anterograde injection of a barium sulphate-gelatine mixture into the intrathecal venous segment was performed. In the remaining 14, retrograde filling of the dural segment was attempted by injection of the X-ray contrast-medium-gelatine mixture from the extradural space.
Following vascular filling, fixation and paraplast-embedding, the contact-microradiographs were taken using a Packard Faxitron X-ray device and high-resolution spectroscopic plates.
A correlative evaluation of microangiographical and histological preparations was attempted in 17 out of these, in the second part of specimens. This means that altogether 102 veins were examined microscopically.
Results
Histology
Histological evaluation of 102 radiculomedullary human spinal cord veins did not demonstrate the presence of valves but confirmed special configurations and arrangements at its transdural course.
The acute angle, which exists between the dural sac and the nerve root entry/exit corresponds to the angle of venous blood vessel exits. The crossing of the dura mater in an oblique direction goes along with narrowing of the lumen and an angled course.
The topical relationship between the dural exit of radiculomedullary veins and nerve roots were
-
joint in 22 %
-
close to each other (< 1 mm) but separate in 47 %
-
distant to each other in 31 %
Two main types of venous exit through the dura mater were identified:
-
slit type comprising 60 % of the veins studied; and
-
bulge or nodular type, which was seen in 35 %.
The remaining 5 % of specimens showed exit-configurations, which could not be assigned to either one of the main types. Histological sections of both types are demonstrated in Fig. 2, a diagram of the two different arrangements in which the veins cross the dura mater is depicted in Fig. 3.
Structurally different types of blood vessel exit through the dura mater. Histological sections, H&E, original magnification 60 ×. a ‘Slit type’ showing a vein accompanying a nerve root to the nerve root sheath before penetrating the dura mater. The vessel course is marked with arrows. The narrowing and oblique transdural course are evident, as well as the alteration of the blood vessel into a fissure-like narrowed channel (Reproduced from [25]) b ‘Bulge or nodular type’ refers to the bulge of collagen in which the vein loses its normal structural integrity
In the slit type (Fig. 2a, 3a) the radicular vein approaches the wall of the dural sac in an acute angle and crosses the dura in an oblique direction. Kinking or sharp bends in different planes occur and may cause the impression of a tortuous course. As mentioned earlier, the calibre of the vessel decreases at its transdural course. Gradually the normal composition of the vessel wall gets lost and is replaced by dural tissue and a layer of arachnoid.
The slit type was regularly observed in specimens with a vein penetrating the dura mater at the entrance of the nerve root sheath. But it could also be seen in the other locations of dural exit. The bulge type (Fig. 2b, 3b, 4) is characterized by a voluminous formation of connective tissue, interrupting the longitudinal course of dural fibre architecture. In this type the vein is eccentrically encapsulated by a mass of dural collagenous fibres following the blood vessel to the epidural space. Within the bulge the vessel lumen is narrowed. It may even be split into different fissures and again the normal composition of the wall of a venous blood vessel gets lost. Additionally, inclination of the bulge parallel to the dura mater creates kinking of the vessel course.
No correlation was found between the slit and bulging type and their frequency at different segmental levels of the spinal cord.
Microradiographs
Microradiographs of the contrast-injected transdural portion of radiculomedullary veins in 12 specimens with anterograde filling demonstrated narrowing and/or bending in most cases (Fig. 5). Rare observations included blind ending radiculomedullary veins (Fig. 6a, b) and stenosis of the vein before entering the dura mater followed by a venous ectasia in the dural layer.
a–f Microangiographic X-rays of radiculomedullary veins following orthograde contrast injection. The veins cross the dura mater to the internal vertebral venous plexus in different configurations a The vein penetrates the dura mater in a right angle with a significantly reduced calibre (arrow) and primarily joins a sponge-like system of epidural cavities (slit-type, level L1). b Oblique transdural course of the vein with considerable narrowing of the dural segment (arrow). The epidural plexus at this point consists of a large lacunar space surrounded by a net-like system of fissures and small cavities (slit-type, level L3) c Tidy narrowing of the dural vein segment and acute angle between the subarachnoid vein and the recipient epidural plexus. In this case the internal vertebral venous plexus is composed of a plexiform irregular convolution of veins of different size (histologically, the type of dural transition could not be assigned, level T6) d Short transdural passage of a radiculomedullary vein running with the nerve root. The lacunar spaces of the epidural venous plexus surround the nerve root sheath (slit-type, level T7) e Two pairs of radiculomedullary veins of different size, merge directly before they cross the dura mater. Narrowing of the lumen and kinking or bending course are similar (arrows). The larger veins empty in a lacunar part of the epidural plexus distant from the nerve root, the smaller ones in an extensively contrasted epidural venous space surrounding the nerve root sleeve (bulging-type, level T10) f Rare configuration with short narrowing of the vessel lumen while crossing the dura mater in an oblique course and continuation through the epidural space as an equally sized intervertebral vein (slit-type, level T7)
Non-functional (fibrotic) veins. The figure parts a and b have been obtained from different specimens. a Photograph of an autopsy specimen at mid-thoracic level. The veins on the posterior surface of the spinal cord have been filled with black ink. The upper part of the main longitudinal venous trunk deviates from the midline to join the proximal segment of a lower radicular vein, emerging from the lower midline vein. The point of junction to form a single vessel is half way to the dura mater in this specimen. The common stem looks like a rudimentary residual of a spinal cord draining radicular vein (arrow). b Microangiography of a non-functional radiculomedullary vein at the L 1 level following orthograde injection via superficial veins. Two veins conjoin to a common stem. Whereas free communication between the two veins is preserved, the resulting radiculomedullary vein presents as a very thin band. Following injection of contrast-medium a filiform residual lumen can be followed to a tiny dural compartment.
Except one case with extradural continuation of a defined venous blood vessel (Fig. 5f), the dural segments of radiculomedullary veins directly joined the internal vertebral venous plexus (Fig. 5a, b, d, e). X-ray imaging of parts of the contrasted epidural venous plexuses demonstrate a complex three-dimensional system of lacunar spaces comparable to a sponge, in which narrow parts, fissures and small cavities alternate with considerably dilated cavities and ectasias. Areas consisting of irregularly composed blood vessel convolutions and large defined veins were rare in our examples (Figs. 5a, c).
Retrograde filling of intrathecal veins from the extradural space was successful in two cases out of 14 attempts (Fig. 7a, b). This was tried using an occasional short stump of an extradural radiculomedullary vein or through extensive filling of the epidural plexus through extraspinal sources.
a Reflux to radicular and superficial veins following injection of the epidural plexus with a solution of X-ray contrast-medium. X-ray of the specimen in anteroposterior view. The white areas of epidural vascular spaces appear irregular and incoherent. They are part of the internal vertebral venous plexus surrounding the dural sac. From this differently composed lacunar system retrograde filling of a radiculomedullary vein (arrowhead) through the narrow passage at dural level (arrow) was observed at the T5 level. Rmv radiculomedullary vein; D Dura mater b Histological section. The content of the radiculomedullary vein is X-ray contrast medium, which passed the dural segment retrogradely (arrow). There is a kinking course of the short dural vein segment, but a narrowing of this part of the vein does not exist. Instead, it looks rather dilated
Discussion
Most of our morphological results are in agreement with the findings of recent investigators, as far as it concerns what we called the ‘slit type’ of blood vessel exit [6, 7, 17]. The spinal cord draining veins exit the dural sac together with the nerve root or in close vicinity to it in approximately 70 % of our specimens, and in approximately 30 % they pierce the dura mater between two spinal nerves. Microscopically, we neither encountered classical valves, nor valve-like intravenous dural folds, as mentioned by van der Kuip et al. [17]. For the majority of examined specimens we confirm the description given by Tadié et al. [6] that the vein takes an oblique, sometimes bending course through the dura mater. The lumen narrows markedly and the layers of the vessel wall are replaced by a layer of arachnoid and dural tissue. Moet and Maillol [20] confirmed narrowing of the vessel diameter immediately before the transdural course. In addition, a significant number of smooth muscle fibres within the wall of the radicular vein before and behind the dural bottle neck was reported by van der Kuip et al. [17], suggesting—in their opinion—some type of dynamic regulation. We have not performed a staining for smooth muscle cells.
In approximately one third of our specimens, a second, so far not described arrangement was seen (Figs. 2b, 3b, 4). The very unusually configured device resembles a dural bulge or a fibrous nodule, which encapsulates the lumen of the blood vessel. Similar to the slit type the regular layers of a venous blood vessel wall are replaced within the dural bulge. The original lumen gets split (Fig. 4) and multiple clefts between the collagen bundles create the aspect of a partly spongy structure.
The functional significance of these different arrangements and configurations of the transdural vein segments is not yet clear. The spongy bulge of connective tissue envelops the narrowed and split vessel lumen and accompanies the vein from the subarachnoid compartment to the extradural compartment. One may speculate that apart from flow-control it might play a role in cerebrospinal fluid reabsorption. In a re-evaluation of histological sections of spinal dural AV fistulae from 4 of our early patients no elements similar to this nodular fibrous formation was found. On the other hand, this re-evaluation revealed a glomus-like element as described by Tadié et al. [6], lying close to the AV shunt, but without apparent causal relationship.
Numerous investigators reported that they were unable to inject intradural spinal veins from the outside of the dural sac in autopsy studies [6, 9–12]. Thus, the assumption of valves in the peridural segment of radicular veins was generally accepted without formal evidence. Only a single study in 1961 stated the presence of valves in three out of ten examined cases [21]. It was not until the investigations of Tadié et al. [6, 7] that the existence of valves in this localization was denied. Still, the idea of the necessity of a reflux-impeding mechanism was maintained. Tadié et al. proposed a different system of anti-reflux mechanism resulting from special arrangements implemented in the dural portion of radicular veins. The blocking mechanism to impede reflux to the intradural spinal cord veins was seen in narrowing of the lumen and a zigzag course of the transdural venous segment. With increasing volume and pressure in the epidural spaces the narrow transdural passage would gradually be closed by swelling of the arachnoid cuff. This would protect the intradural system from acute rises of pressure. However, impaired venous return resulting from chronically elevated pressure would not be influenced [6]. If one accepts this easily comprehensible mechanism the presented bulge type with its inclination parallel to the dura mater should be even more efficient in reflux–control than the slit type.
However, not only the presence of valves but also generally the existence of anti-reflux arrangements is not undisputed. In clinical epidural venography retrograde filling of a superficial spinal cord vein was occasionally observed [22, 23]. In two recent experimental cadaver studies using injection of a modern polymer (Araldite CY 221) to demonstrate the internal vertebral venous plexuses [16] and the human radicular veins [17] concomitant retrograde filling of intradural radicular veins was documented as a rather regular and not as an exceptional observation. In all 10 injected cadavers a total number of 62 radicular veins appeared to be filled macroscopically (range 1–15). These findings are appropriate to question the idea of an effective reflux-impeding system. The authors explain the high retrograde filling rate in the cadaver studies not with special properties of the injected polymer solution of low viscosity, but with the preparation of the specimens prior to the injection procedure. They flushed the vertebral venous system with saline and a thrombolytic agent, to remove obstructive blood clots and to obtain perfusion of the internal vertebral venous plexus.
In our 14 attempts to achieve retrograde transdural filling of radicular veins without a special preparation of the cadavers, contrast-medium in vessel segments of the subarachnoid space could be noted in two specimens. In the example illustrated on the microangiographic image of Fig. 7a the radiculomedullary vein is retrogradely filled with contrast material until the sharp bend at the point where it communicates with the median longitudinal vein. Narrowing of the radicular vein in the exit-zone is evident (arrow). A correlative histological section of this specimen is shown in Fig. 7b. The contrast-filled dural segment of the vein exhibits a somewhat serpentine course, but traceability and display of the vessel lumen is only possible on a series of consecutive histological sections. Figure 8 demonstrates an example of semi-thin sectioning. Only moderate narrowing of the dural segment can be seen, a specific anti-reflux arrangement is not detectable.
Simple configured transdural course demonstrated in this example of semi-thin sections. Specimen from the T9 level. Original magnification 360 ×. This blood vessel exit close to the nerve root displays only moderate narrowing of the lumen in its short transdural portion. The absence of valves is evident
The X-ray of the injected specimen shown in Fig. 7 demonstrates very well the connection between the radicular spinal cord vein and an internal vertebral venous plexus, which—in this example—is composed of multitudinous communicating lacunar spaces. The venular or plexal nature of this efferent system is still controversial [24]. Most of the epidural venous plexus compartments in our specimens injected for microangiography have a similar aspect, best be described as a system of smaller and larger venous lakes, lacunes and fissures (Fig. 5). Only in a few cases, the epidural plexus was composed of defined venous blood vessels or a mixture of both (Fig. 5a, c).
When retrograde injection of superficial spinal cord veins in post-mortem examinations failed, a causal relationship with significant thrombotic obstruction of this unusual epidural system of communicating lacunar spaces has not been considered. The same is true for a possible role of this system in flow and pressure adjustment.
In clinical applications of functional anatomy more open questions arise. Why is the direction of blood flow in SDAVF usually not associated with simultaneous shunting into compartments of the epidural plexus? If there is not spontaneous occlusion of the arterialized epidural compartment it should be expected that drainage of these shunts, which are located at the dural passage of radicular veins, should occur in various directions. Still, we have rarely observed epidural fistulas with perimedullary drainage in clinical cases [25]. Some more reports exist about clinically symptomatic arteriovenous fistulas with the flow primarily directed to the epidural plexus [26–28]. All of these cases except one [26] had secondary reflux from the epidural plexus to the superficial spinal cord veins, as demonstrated by angiography. In the clinical observation of epidural shunts, they are mostly confined to restricted segments and small spaces. In a case reported by our group in 2006 [25] the epidural involvement was more extensive, crossed the midline and filled multiple compartments before retrogradely entering the radicular vein. These clinical observations are suitable to additionally create doubt that the dural passage of radicular veins represents systems definitively preventing reflux although two different configurations of the transdural vessel course appear appropriate to modulate flow (Fig. 3). The purpose of two different arrangements, especially of the ‘nodular type’ remains unclear.
The occurrence of blind ending fibrotic radicular veins (Fig. 6a, b), most frequent among the posterior thoracic ones [20], might be explained by the individually poor development of the posterior internal vertebral venous plexus as described by Groen et al. [16]. The internal vertebral venous plexus as part of the voluminous vertebral venous system exhibits structural and functional characteristics, which might indicate an adaptive role for the entire spinal cord blood circulation. The results from our study and from recent reports [17] support the idea that valve-like blocking mechanisms in the transdural course of radicular veins are not needed and that investigations on flow and pressure modulating effects of the internal vertebral venous plexus should receive greater attention.
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
Kendall BE, Logue V. Spinal epidural angiomatous malformations draining into intrathecal veins. Neuroradiology. 1977;13:181–9.
Merland JJ, Riché MC, Chiras J. Les fistules arterio-veineuses intra-canalaires, extra-médullaires à drainage veineuxmédullaire. J Neuroradiol. 1980;7:271–320.
Foix Ch, AlajouanineTh. La myélite nécrotique subaigue. Rev Neurol. 1926;33:1–42.
Thron A, Koenig E, Pfeiffer P, Rossberg C. Dural vascular anomalies of the spine- an important cause of progressive myelopathy. In: Cervos-Navarro J, Ferszt R, editors. Stroke and microcirculation. New York: Raven Press; 1987.
Thron AK. Vascular anatomy of the spinal cord. Neuroradiological investigations and clinical syndromes. Wien: Springer; 1988.
Tadié M, Hemet J, Freger P, Clavier E, Creissard P. Anatomie morphologique et circulaire des veines de la moelle. J Neuroradiol. 1985;12:3–20.
Tadié M, Hemet J, Aaron C, Bianco C, Creissard P, Huard P. Le dispositive protecteur anti-reflux des veines de la moelle. Neuro-Chir. 1979;25:28–30.
Aboulker J, Bar D, Mursault L, Khoudja F, Redondo A, Gard L, Nahum H. L’hypertension veineuse intra-rachidienne par anomalies multiples du systeme cave: une cause majeure de souffrance medullaire. Chirurgie. 1977;103:1003–15.
Breschet G. Recherches anatomiques, physiologiques et pathologiques sur les systems veineux et specialement sur les canaux veineux des os. Villaret, Paris 1828–1832.
Batson OV. The vertebral vein system. Am J Roentgenol. 1957;78:195–212.
Clemens HJ. Die Venensysteme der menschlichen Wirbelsäule. Berlin: De Gruyter; 1961.
Crock HV, Yamagishi M, Crock MC. The conus medullaris and cauda equina in man. An atlas of the arteries and veins. Wien: Springer; 1986.
Otto J. Morphologie des Sperrmechanismus am Duradurchtritt der Venae radiculares des Menschen. Neuroradiologische und histologische Befunde. Thesis for Doctorate in Medicine. University Aachen, 1990.
Thron A, Otto J, Schroeder JM. Functional anatomy of the dural segment of spinal cord draining veins. A histological and microangiographical study. In: du Boulay G, editor. Symposium Neuroradiologicum. Book of Abstracts. London: Springer; 1990. p. 323.
Schroeder JM, Otto J, Thron A. Protective anti-reflux devices for spinal veins at the radicular nerve entry/exit zone: a correlative microscopic and microangiographic autopsy study. Schweiz Arch Neurol Psychiatr. 1993;144:29–30.
Groen RJM, Groenewegen HJ, van Alphen HAM, Hoogland PVJM. Morphology of the human internal vertebral venous plexus: a cadaver study after intravenous Araldite CY 221 injection. Anat Rec. 1997;249:285–94.
van der Kuip M, Hoogland PV, Groen RJ. Human radicular veins: regulation of venous reflux in the absence of valves. Anat Rec. 1999;154:173–80.
Chen J, Ethiati T, Gailloud P. Flat panel catheter angiotomography of the spinal venous system: an enhanced venous phase for digital subtraction angiography. AJNR Am J Neuroradiol. 2012;33:1875–81.
Gailloud P. The arrow-tipped loop is a marker of radiculomedullary vein thrombosis linked to the anti-reflux mechanism-angiographic anatomy and clinical implications. Neuroradiology. 2014;56(10):859–64.
Moes P, Maillot C. Les veines superficielles de la moelle epinière chez l´homme. Essai de systematisation. Archives D’Anatomie D’Histologie D’Embryologie normales et expérimentales. Extrait du tome 64. Paris: Edition Alsatia; 1981. pp. 5–110.
Oswald K. Untersuchungen über das Vorkommen von Sperrmechanismen in den Venae radiculares des Menschen. Berlin: Med Inaug Diss; 1961.
Théron J, Moret J. Spinal phlebography. Berlin: Springer; 1978.
Meijenhorst GCH. Lumbar epidural double-catheter venography with Metrizamide (Amipaque). Diagn Imaging. 1977;48:244–252.
Lasjaunias P, Berenstein A. Surgical neuroangiography. Vol. 3: Functional vascular anatomy of brain, spinal cord and spine. 1st Ed. Berlin: Springer 1990. p. 80–87.
Krings T, Mull M, Bostroem A, Otto, J, Hans FJ, Thron A. Spinal epidural arteriovenous fistula with perimedullary drainage. Case report and pathogenetical considerations. J Neurosurg Spine. 2006;5:353–8.
Chen CJ, Huang CC, Hsu YY, Hsu WC. Small isolated paraspinal arteriovenous fistula. AJNR Am J Neuroradiol. 1977;18:359–61.
Cognard C, Semaan H, Bakchine S, Miaux Y, Thibault S, Sola Martinez MT, Chiras J. Paraspinal arteriovenous fistula with perimedullary venous drainage. AJNR Am J Neuroradiol. 1995;16:2044–8.
Pirouzmand F, Wallace MC, WiIIinsky R. Spinal epidural arteriovenous fistula with intramedullary reflux. Case report. J Neurosurg. 1997;87:633–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thron, A., Krings, T., Otto, J. et al. The Transdural Course of Radicular Spinal Cord Veins—A Microangiographical and Microscopical Study. Clin Neuroradiol 25, 361–369 (2015). https://doi.org/10.1007/s00062-015-0476-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-015-0476-x