Abstract
Background
This study aimed to investigate the prognostic value of C-reactive protein to albumin ratio (CAR) in hepatocellular carcinoma (HCC) patients after transcatheter chemoembolization (TACE).
Methods
Totally, 958 HCC patients with Barcelona Clinic Liver Cancer (BCLC) stage B were incorporated into the secondary analysis. X-Tile software was applied to determine the optimal cutoff point for CAR, and the total patients were divided into two groups. Cox proportional hazard regression models and Kaplan–Meier analyses were used to estimate the relationship between CAR and overall survival (OS). Stratified analyses were performed to evaluate the prognostic role of CAR in subgroups of major confounding factors, such as alpha‐fetoprotein (AFP), diameter of the main tumor, Glasgow prognostic score (GPS) and modified GPS (mGPS).
Results
The optimal cutoff level for the CAR was 0.06. There was a direct correlation between an elevated CAR (≥ 0.06) and shorter OS after adjustment (HR:1.580; 95%CI:1.193–2.092). Kaplan–Meier analysis and log-rank test showed a significant difference in OS curves between the two groups (P < 0.001). CAR showed the distinct value of prognostic stratification in most subgroups, especially in the subgroup of GPS-0 (HR:1.966; 95%CI:1.453–2.660), mGPS-0 (HR:1.984; 95%CI:1.509–2.608) and AFP ≤ 400 ng/ml (HR:1.925; 95%CI:1.393–2.659).
Conclusion
The CAR was one of the prognostic factors for HCC patients undergoing TACE treatment. CAR could also provide further prognostic stratification for HCC patients who appear to have a good prognosis, such as patients with AFP-negative, GPS-0 or mGPS-0 to identify patients at a higher risk of death for closer follow-up or more aggressive treatment.
Level of Evidence
Level 3, Cohort Study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver cancer is the sixth most common type of cancer worldwide and one of the leading causes of cancer-related death [1]. Hepatocellular carcinoma (HCC) accounts for approximately 90% of these tumors [2]. Most patients with liver cancer miss the opportunity of surgery by the time they are first diagnosed. As one of the minimally invasive treatments, transcatheter chemoembolization (TACE) is of great significance for these patients, especially those who are in Barcelona clinic liver cancer intermediate stage (BCLC-B) [3]. However, the responses of HCC patients to TACE are highly heterogeneous, which presents a great challenge for predicting clinical outcomes. Therefore, it is urgent to find effective prognostic biomarkers for HCC patients before TACE.
Various studies have demonstrated that immune-inflammatory response serves a significant part of tumor development and progression, especially in HCC patients with chronic inflammation [4]. C-reactive protein (CRP), regulated by proinflammatory cytokines, is an acute-phase protein with good stability and accuracy [5]. High levels of CRP have been found to predict not only the degree of inflammation and tissue damage, but also inferior prognosis in many tumors, such as lung, breast and stomach cancers [6,7,8,9]. Serum albumin is synthesized in the liver reflecting people’s nutritional status and liver function. Previous research showed that a low albumin level could predict poor survival in multiple cancers [10, 11]. Taking the serum level of CRP and albumin as elements, a series of valuable scores for assessing the prognosis of different tumor types have been developed, such as Glasgow prognostic score (GPS), modified GPS (mGPS) and C-reactive protein to albumin ratio (CAR) systems [12,13,14].
Extensive studies have validated patients with cancer could be classified into three different levels (0/1/2) of risk of death by GPS or mGPS [15]. In recent years, research has found that compared with GPS or mGPS, CAR is a quantitative parameter synthesizing values more reasonable and has been considered a more potential prognostic indicator in different types of tumors, including HCC [16]. Nevertheless, the previous studies mainly focused on the HCC patients receiving surgical treatment, and there was a lack of separate analysis for HCC patients with BCLC-B, for whom TACE is recommended as the first-line treatment [17]. In this study, we investigated the prognostic value of CAR in HCC patients undergoing TACE.
Materials and Methods
Design and Patients
This was a secondary data analysis of a multicenter cohort study including 2020 newly diagnosed HCC patients from January 2007 to December 2016. The inclusion criteria were: (1) The clinical stage was BCLC stage B; (2) the data of blood routine examination, serum CRP and albumin levels, abdominal imaging and follow-up were complete; and (3) without other malignant tumors. We mainly studied the derivation cohort of 979 HCC patients, and 21 patients who missed CRP or albumin data were ruled out. Finally, 958 HCC patients were incorporated into our study.
Demographic and laboratory data were extracted for analysis: gender, age, serum CRP level, cause and type of hepatitis (hepatitis B virus [HBV] infection or others), blood routine examination factors (hemoglobin [Hb] level, white blood cell [WBC] count, platelet [PLT] count), parameters of liver function (albumin [ALB], aspartate transaminase [AST] and total bilirubin [TBIL] levels, etc.), tumor characteristics (diameter of the main tumor, number and location of intrahepatic lesions) and alpha‐fetoprotein (AFP) level.
TACE Procedure and Follow-Up
TACE treatments included conventional TACE (cTACE) and drug-eluting bead TACE (DEB-TACE). It depended on the physicians to choose based on the patient’s liver function and tumor size, number and location. All procedures were performed by experienced interventional radiologists to ensure the standardization of procedures. Take cTACE for example, the right femoral artery was punctured using the Seldinger technique and a catheter was routinely placed to perform digital subtraction angiography (DSA) of the hepatic artery to locate the lesion distribution and tumor supply vessels. After the catheter was properly positioned, a mixture of doxorubicin (10–50 mg) and lipiodol (2–20 ml) was injected, followed by embolization with gelatin sponge particles. Successful embolization was determined if there was no contrast staining during angiography after embolization. DEB-TACE was similar to cTACE except for embolic materials.
Subsequent treatment after TACE consisted of repeated TACE, ablative therapies, surgical resection, targeted therapies, or palliative chemotherapy, determined by the multidisciplinary teams, including hepatologists, radiologists, and interventional radiologists. Patients were followed monthly during initial treatment and every 2–3 months for the first 2 years if complete remission was achieved. After two years of remission, the frequency could decrease to once every 3–6 months.
Definition and Measurement
The GPS consisted of inflammatory (if CRP > 1.0 mg/dl was assigned a score of 1, otherwise 0) and nutritional conditions (if albumin < 3.5 mg/dl was assigned a score of 1, otherwise 0). For mGPS, if both CRP > 1.0 mg/dl and albumin < 3.5 mg/dl were assigned a score of 2, and only one or neither of the two biochemical abnormalities was assigned a score of 1 or 0, respectively. The CAR was calculated by dividing the serum CRP level (mg/dl) by serum albumin level (g/dl). OS was defined as the time from the date of diagnosis of HCC to death by any cause. HBV was defined as hepatitis B virus infection and other as other causes of hepatitis. In addition, both lobes with lesions was defined as lesions occurring at both the left and right lobes of the liver.
Statistical Analysis
We applied X-Tile software (version 3.6.1, copyrighted by Yale University, 2003–2005) to determine the optimal cutoff point for CAR, and the total patients were divided into two groups (Online Resource 1). The χ2 test or Fisher exact test was used to compare the baseline characteristics of the two groups. The Kaplan–Meier method was used to draw the cumulative risk curve and the log-rank test was used to compare survival differences between the groups. The relationship between the clinical factors and OS was explored by applying univariate and multiple Cox proportional hazard regression analysis. Statistically significant factors obtained from univariate analysis were included in multivariate analysis. We made a stratified analysis of the known major covariates that may influence the OS, including age, cause and type of hepatitis, LDH, AFP, diameter of the main tumor, number and location of tumors, Child–Pugh class, GPS and mGPS (Fig. 2). Heterogeneity across subgroups was determined by stratified Cox proportional hazards models, and the likelihood ratio tests were used to examine the interactions between the subgroups.
A two-tailed P value < 0.05 was considered statistically significant. All analyses were performed using Empower (R) (www.empowerstats.com, X&Y solutions, Inc. Boston, MA).
Results
Baseline Characteristics
From January 2007 to May 2012, a total of 958 HCC patients with BCLC stage B were retrospectively analyzed. The patients were predominantly male (90.8%), whose average age was 55 (14–85) years. According to the cause of disease, most participants (829/958, 86.5%) were HBV infected. The median OS time was 23.3 months (95%CI:20.294–26.306). By the last follow-up date, 540 (56.4%) patients had died. The patients were divided into two groups based on the best cutoff value of CAR (0.06). We compared the clinical characteristics of patients between the two groups in Table 1, indicating significant differences in age, Hb, AST, LDH, AFP, diameter of the main tumor, Child–Pugh class, GPS and mGPS.
Association Between CAR and OS in HCC Patients Undergoing TACE
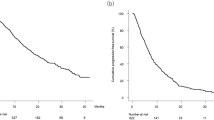
The comparison between the OS for HCC patients of the two groups is shown in Fig. 1. The median OS time was 49.1 months (95%CI:36.513–61.687) for the group of CAR < 0.06, 23.3 months (95%CI:20.294–26.306) for the group of CAR ≥ 0.06. The 1-, 3-, and 5-year OS rates were 87.3, 56.5, and 40.5% for the low CAR group, and were 62.7, 35.6 and 27.6% for the high CAR, respectively. The two groups showed significant differences in survival rates (P < 0.0001).
As given in Table 2, the results of univariate analyses showed that CAR ≥ 0.06 (HR:1.801; 95%CI:1.425–2.276), both lobes with lesion (HR:1.509; 95%CI:1.267–1.797), intrahepatic lesion > 3 (HR:1.569; 95%CI:1.314–1.873), main tumor > 50 mm (HR:2.246; 95%CI:1.850–2.726), AFP > 400 ng/ml (HR:1.430; 95%CI:1.203–1.700), LDH > 215 U/L (HR:1.546; 95%CI:1.299–1.840), Child–Pugh class = B(HR:1.387; 95%CI:1.092–1.761), GPS = 1,2 (HR:1.296; 95%CI:1.083–1.552) and mGPS = 1,2 (HR:1.241; 95%CI:1.045–1.473) were related to a higher mortality risk.
Multivariate analysis including the above prognostic factors indicated that CAR ≥ 0.06 was independently linked to a higher death risk (HR:1.580; 95%CI:1.193–2.092) along with both lobes with lesion (HR:1.407; 95%CI:1.174–1.687), intrahepatic lesion > 3 (HR:1.395; 95%CI:1.160–1.679), main tumor > 50 mm (HR:2.078; 95%CI:1.697–2.544), AFP > 400 ng/ ml (HR:1.231; 95%CI:1.032–1.469), LDH > 215 U/L (HR:1.233; 95%CI:1.026–1.481) and Child–Pugh class = B (HR:1.320; 95%CI:1.024–1.701).
Subgroup Analysis for OS
In the subgroup of age ≥ 50(y), cause and type of hepatitis(HBV/others), LDH ≤ 215/ > 215(U/L), AFP ≤ 400/ > 400(ng/ml), diameter of the main tumor ≤ 50/ > 50(mm), both lobes with lesions(no/yes), number of intrahepatic lesions(≤ 3/ > 3), Child–Pugh class = A, GPS-0 and mGPS-0, CAR ≥ 0.06 showed a significant increase in death risk, especially in the subgroup of AFP, GPS and mGPS (Fig. 2).
To explore the combined effect of age, AFP, and CAR on mortality risk, the HRs of the CAR groups stratified by five subgroups of age (5-y groups) and two subgroups of AFP (≤ 400 and > 400) are shown in Table 3. After adjusting for confounding factors, among age 55–60(y) and age 60–65(y) people with AFP ≤ 400(ng/ml), the high CAR group showed a 2.3- and 2.9-fold increase in mortality risk compared with the low CAR group, respectively. In contrast, the increased risk for other age subgroups was not statistically significant.
As shown in Fig. 2, the CAR classified patients with GPS-0 points and mGPS-0 points, who showed longer survival than those with GPS-1/2 or mGPS-1/2 points, into two groups. Two survival curve analyses confirmed that the death risk of patients with CAR ≥ 0.06 was significantly higher than patients with CAR < 0.06, whether in the GPS-0 group (median OS:18.400 months; 95%CI:12.606–24.194 VS median OS:49.100 months; 95%CI:31.708–61.492) or mGPS-0 group (median OS:18.200 months; 95%CI:14.038–22.362 VS median OS:49.100 months; 95%CI:31.513–61.687) (Fig. 3).
Discussion
In this secondary analysis, we demonstrated that HCC patients undergoing TACE with a high level of CAR tended to have a shorter OS. Moreover, CAR can identify subgroups at high risk for poor outcomes among those indicating better postoperative survival, such as the AFP-negative group, GPS-0 and mGPS-0 group. As an adjustable prognostic factor, CAR could guide physicians to monitor patients with high CAR levels more closely and provide anti-inflammatory therapy or nutritional support in their clinical practice.
Several studies have revealed that systemic inflammatory responses and nutrient consumption serve important parts in promoting poor prognosis in malignant tumor patients [18, 19]. CRP is an acute-phase protein stimulated mainly by proinflammatory cytokines, particularly Interleukin-6(IL-6). Elevated CRP level in tumors, indicating the presence of an intense inflammatory reaction, often accompanies total protein loss and increased tissue metabolism, leading to a poor nutritional status and a high risk of death[15, 20]. Serum albumin is a recognized marker of malnutrition in cancer, as a higher rate of albumin degradation and turnover within more aggressive tumor cell populations. This should be particularly emphasized in the treatment of HCC patients. As most HCC patients have cirrhosis, liver synthesis dysfunction caused by liver cirrhosis and tumor can lead to impaired nutritional status. These research backgrounds have contributed to the development of prognostic scores based on CRP and albumin levels, such as the GPS, mGPS and CAR [12, 13, 16].
In the univariate analysis, the GPS, mGPS and CAR were all related to the adverse clinical outcomes of HCC patients undergoing TACE. After multivariate analysis, CAR remained an independent prognostic indicator. The results were consistent with previous research on CAR in HCC patients [16]. We also identified that tumor size, tumor number, tumor location, AFP level, Child–Pugh class and LDH level were still significant prognostic factors in the multivariate analysis, which were generally compatible with those of previous studies that described these markers’ roles in tumor burden [21].
AFP is still the most authoritative serological indicator for the diagnosis and monitoring of HCC. However, it has been found that AFP elevation in many HCC patients is not obvious or even not elevated [22], which was consistent with our findings. Therefore, based on the AFP threshold of 400 ng/ml, we classified the participants to perform a subgroup analysis. The stratified results demonstrated that HCC patients with a higher CAR level were more likely to have worse clinical outcomes independent of serum AFP levels, which was also confirmed by recent research reported by Wu et al. [23]. Besides, we disclosed that the relationship between CAR and OS varied with aging, making CAR a potent prognostic predictor for AFP-negative HCC patients aged 55 to 65 years. The mechanisms underlying the heterogeneity of AFP- and age-related CAR effects remain to be clarified.
Consistent with the study of Ishizuka et al., CAR was shown could divide patients with GPS-0 (Fig. 3a) or mGPS-0 (Fig. 3b) into two independent groups [9]. The possible mechanisms might be explained as follows. As GPS and mGPS are qualitative scores in nature, the additive effect of rough classification of values may lead to higher or lower prognostic assessments of tumor patients than they are [24]. Although CAR, like GPS and mGPS, divides a patient’ prognosis into different tiers, CAR acts as a quantitative ratio that theoretically makes more precise use of values. This suggests that even HCC patients with a low GPS/mGPS score, which generally indicates a better long-term prognosis, can still be screened out for high-risk patients (GPS:155/329; mGPS:180/412) with additional CAR assessment for active intervention.
In subgroup analysis, we also found that CAR showed the distinct value of prognostic stratification in most subgroups of clinical indicators, especially in the subgroup of age ≥ 50 years, LDH > 215 U/L, number of intrahepatic lesions > 3, both lobes with lesions and Child–Pugh = A, which further demonstrated the ability of CAR to predict cancer prognosis.
Several limitations of this study should also be acknowledged. Firstly, the study was based on retrospective data from a single center. Secondly, although stratified analyses showed the prognostic value of CAR in HCC patients with different etiology, the most patients in this study were HBV infected, and further validation is needed in a larger population with non-hepatitis B. Thirdly, the type of TACE procedures including cTACE and DEB-TACE was not collected in the raw data, though until today, no significant difference in tumor response or survival has been observed between them [25]. In addition, as the treatment model for hepatocellular carcinoma has changed from single local treatment to multi-disciplinary integrated treatment, further confirmation of the prognostic value of CAR in HCC patients receiving TACE-based combination therapy is needed.
Conclusions
In this large-scale, retrospective cohort study, we demonstrated that the CAR could serve as a simple, inexpensive, readily available prognostic factor in HCC patients undergoing TACE treatment. CAR could also provide further prognostic stratification for HCC patients who appear to have a good prognosis, such as patients with AFP-negative, GPS-0 or mGPS-0 to identify patients at a higher risk of death for closer follow-up or more aggressive treatment.
Data Availability
The raw data were freely obtained from the Dryad Digital Repository database (www.Datadryad.org; Dryad data package: Shen, Lujun et al. (2019), Data from: Dynamically prognosticating patients with hepatocellular carcinoma through survival paths mapping based on time- series data, Dryad, Dataset, https://doi.org/10.5061/dryad.pd44k8r).
References
Sung H, Ferlay J. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021. https://doi.org/10.3322/caac.21660.
EASL-EORTC. EASL-EORTC clinical guidelines: management of hepatocellular carcinoma. J Hepatol. 2012. https://doi.org/10.1016/j.jhep.2011.12.001.
Han K, Kim JH. Transarterial chemoembolization in hepatocellular carcinoma treatment: Barcelona clinic liver cancer staging system. World J Gastroenterol. 2015. https://doi.org/10.3748/wjg.v21.i36.10327.
Chan SL, Chan AW. Systematic evaluation of circulating inflammatory markers for hepatocellular carcinoma. Liver Int. 2017. https://doi.org/10.1111/liv.13218.
Nagaoka S, Yoshida T. Serum C-reactive protein levels predict survival in hepatocellular carcinoma. Liver Int. 2007. https://doi.org/10.1111/j.1478-3231.2007.01550.x.
Zhang XY, Zhang G. The prognostic value of serum C-reactive protein-bound serum amyloid A in early-stage lung cancer. Chin J Cancer. 2015. https://doi.org/10.1186/s40880-015-0039-1.
Villaseñor A, Flatt SW. Postdiagnosis C-reactive protein and breast cancer survivorship: findings from the WHEL study. Cancer Epidemiol Biomarkers Prevent. 2014. https://doi.org/10.1158/1055-9965.Epi-13-0852.
Kim EY, Yim HW. C-reactive protein can be an early predictor of postoperative complications after gastrectomy for gastric cancer. Surg Endosc. 2017. https://doi.org/10.1007/s00464-016-5272-4.
Ishizuka M, Nagata H. Clinical significance of the C-reactive protein to albumin ratio for survival after surgery for colorectal cancer. Ann Surg Oncol. 2016. https://doi.org/10.1245/s10434-015-4948-7.
Johnson PJ, Berhane S. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015. https://doi.org/10.1200/jco.2014.57.9151.
Königsbrügge O, Posch F. Association between decreased serum albumin with risk of venous thromboembolism and mortality in cancer patients. Oncologist. 2016. https://doi.org/10.1634/theoncologist.2015-0284.
Forrest LM, McMillan DC. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2003. https://doi.org/10.1038/sj.bjc.6601242.
McMillan DC, Crozier JE. Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Colorectal Dis. 2007. https://doi.org/10.1007/s00384-006-0259-6.
Fairclough E, Cairns E. Evaluation of a modified early warning system for acute medical admissions and comparison with C-reactive protein/albumin ratio as a predictor of patient outcome. Clinical Med. 2009. https://doi.org/10.7861/clinmedicine.9-1-30.
McMillan DC. The systemic inflammation-based glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013. https://doi.org/10.1016/j.ctrv.2012.08.003.
Kinoshita A, Onoda H. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015. https://doi.org/10.1245/s10434-014-4048-0.
Lin N, Li J. Clinical significance of C-reactive protein to albumin ratio in patients with hepatocellular carcinoma: a meta-analysis. Dis Markers. 2020. https://doi.org/10.1155/2020/4867974.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001. https://doi.org/10.1016/s0140-6736(00)04046-0.
Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015. https://doi.org/10.1038/nrclinonc.2015.105.
Roxburgh CS, McMillan DC. Cancer and systemic inflammation: treat the tumour and treat the host. Br J Cancer. 2014. https://doi.org/10.1038/bjc.2014.90.
Xu L, Peng ZW. Prognostic nomogram for patients with unresectable hepatocellular carcinoma after transcatheter arterial chemoembolization. J Hepatol. 2015. https://doi.org/10.1016/j.jhep.2015.02.034.
Asrih M, Lenglet S. Alpha-fetoprotein: a controversial prognostic biomarker for small hepatocellular carcinoma. World J Gastroenterol. 2013. https://doi.org/10.3748/wjg.v19.i3.328.
Wu MT, He SY. Clinical and prognostic implications of pretreatment albumin to C-reactive protein ratio in patients with hepatocellular carcinoma. BMC Cancer. 2019. https://doi.org/10.1186/s12885-019-5747-5.
Liu X, Sun X. Preoperative C-reactive protein/albumin ratio predicts prognosis of patients after curative resection for gastric cancer. Transl Oncol. 2015. https://doi.org/10.1016/j.tranon.2015.06.006.
Müller L, Stoehr F. Current strategies to identify patients that will benefit from tace treatment and future directions a practical step-by-step guide. J Hepatocell Carcinoma. 2021. https://doi.org/10.2147/jhc.S285735.
Acknowledgements
We gratefully thank for the raw data from Prof. Peihong Wu (E-mail: wuph@sysucc.org.cn) and the support from the Dryad Digital Repository database.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by the author. The original study approach (2017-FXY-129) had been approved by the department of clinical research at SYSUCC.
Informed Consent
As this was a secondary analysis study and the data were anonymous, informed consent was not necessary.
Consent for Publication
As this was a secondary analysis study and the data were anonymous, consent for publication was not necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, J., Yang, S., Li, Y. et al. The C-Reactive Protein to Albumin Ratio Is an Independent Prognostic Factor in Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization: A Large Cohort Study. Cardiovasc Intervent Radiol 45, 1295–1303 (2022). https://doi.org/10.1007/s00270-022-03208-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-022-03208-w