Abstract
Purpose
Radioembolization of liver metastases of neuroendocrine neoplasms (NEN) has shown promising results; however, the current literature is of limited quality. A large international, multicentre retrospective study was designed to address several shortcomings of the current literature.
Materials
244 NEN patients with different NEN grades were included.
Methods
Primary outcome parameters were radiologic response 3 and 6 months after treatment according to RECIST 1.1 and mRECIST. Secondary outcome parameters included clinical response, clinical and biochemical toxicities.
Results
Radioembolization resulted in CR in 2%, PR in 14%, SD in 75% and PD 9% according to RECIST 1.1 and in CR in 8%, PR in 35%, SD in 48% and PD in 9% according to mRECIST. Objective response rates improved over time in 20% and 26% according to RECIST 1.1. and mRECIST, respectively. Most common new grade 3–4 biochemical toxicity was lymphocytopenia (6.7%). No unexpected clinical toxicities occurred. Radioembolization-specific complications occurred in < 4%. In symptomatic patients, improvement and resolution of symptoms occurred in 44% and 34%, respectively. Median overall survival from first radioembolization was 3.7, 2.7 and 0.7 years for G1, G2 and G3, respectively. Objective response is independent of NEN grade or primary tumour origin. Significant prognostic factors for survival were NEN grade/Ki67 index, ≥ 75% intrahepatic tumour load, the presence of extrahepatic disease and disease control rate according to RECIST 1.1.
Conclusion
Safety and efficacy of radioembolization in NEN patients was confirmed with a high disease control rate of 91% in progressive patients and alleviation of NEN-related symptoms in 79% of symptomatic patients.
Level of evidence
4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasm (NEN) is a generic term for a class of rare tumours, consisting of an array of many different tumour types with steadily rising incidence. NEN can be divided by tumour grading, in accordance with the World Health Organization/European NeuroEndocrine Tumour Society (WHO/ENETS) grading system [1, 2]. At diagnosis, 21% of grade 1 neuroendocrine tumours (NET), 30% of grade 2 NET and 50% of grade 3 NET (or neuroendocrine carcinoma = NEC) patients demonstrate distant metastases, of which the liver is the most commonly affected site [3, 4]. Once NEN patients are diagnosed with liver metastasis, only about 20–30% are eligible for surgical resection with curative intent, due to frequently present bilobar liver infiltration [3, 5]. With just a few randomized controlled trials providing evidence for efficacy of systemic therapeutic options in advanced NEN and no randomized controlled trials comparing efficacy of locoregional interventions, apart from several guidelines, there is little evidence to guide the choice of treatment for these patients [6,7,8,9,10].
Radioembolization has gained interest due to reports on promising results with limited toxicities. However, in current studies, NEN patients are often presented within a mixed population of non-NEN tumour types, and mostly in small numbers [11, 12]. Furthermore, many publications do not adequately report baseline characteristics, such as tumour grading and origin of the primary tumour, and if reported, these baseline characteristics are mostly not correlated to response or to survival [11, 12]. At the same time, large prospective studies and randomized controlled trials are notoriously difficult for NEN, due to its relatively rare occurrence, the large heterogeneity among NEN patients and the heavily pre-treated population that presents for liver-directed therapies. In this international, multicentre, retrospective study, we investigated efficacy and toxicity of a first radioembolization treatment in NEN with yttrium-90 (90Y) resin microspheres (SIRSpheres®, Sirtex Medical, Sydney, Australia) and focussed on missing data in the current literature.
Methods
All retrospective data were gathered in the period of July 2015 until October 2016 in eight participating hospitals in Europe and the USA (Supplemental Table 1) by the first author to ensure consistent data gathering. The inclusion criteria were patients with histologically proven NEN, of any origin, with at least baseline and 3 ± 1.5 month follow-up cross-sectional imaging (i.e. contrast-enhanced computed tomography = CT or magnetic resonance imaging = MRI). Additionally, biochemical and haematological laboratory data available after radioembolization with 90Y resin microspheres were gathered. If available, imaging up to 6 ± 1 months after treatment was collected. Baseline and follow-up imaging had to be the same imaging modality (either CT or MRI). If patients received multiple radioembolization treatments, of one lobe or whole liver, only the first treatment was evaluated. This to obtain a comparable and reliable toxicity profile, as repeated radioembolization treatments are known to have more treatment-related toxicities [13]. Baseline patient and tumour characteristics, angiography and treatment specifics were gathered according to the reporting standards recommended for radioembolization [14]. Histological diagnosis of a NEN was confirmed on a surgical specimen or biopsy. Intrahepatic tumour load was visually estimated, and the number of intrahepatic lesions was counted.
Prior to the actual radioembolization treatment, all patients received a treatment simulation during a preparatory angiography, in which the microcatheter position is determined for the actual treatment, followed by intra-arterial injection of technetium-99m macroaggregated albumin (99mTc-MAA). After the preparatory angiography, the patient is transported to the nuclear medicine department for planar imaging and SPECT or SPECT/CT. On planar imaging, the lung shunt fraction (LSF) is calculated, and based on the LSF, the physician could consider a dose reduction for treatment. On SPECT(/CT), extrahepatic depositions of the radiopharmaceutical were excluded prior to treatment. Within weeks following the preparatory angiography and imaging, the patient received radioembolization treatment. Prophylactic intravenous octreotide infusion or prophylactic antibiotic treatment was given at the discretion of the treating physician and according to the institutes’ guideline.
Study Outcome Parameters
The primary outcome parameter was imaging response after radioembolization of the liver disease only, defined according to Response Evaluation Criteria In Solid Tumours, version 1.1 (RECIST 1.1), and modified RECIST (mRECIST; in case multiphase imaging was available for hypervascular tumours) after 3 months [15, 16]. RECIST 1.1 was used, because it is currently the most commonly applied response criterion in the NEN literature. mRECIST was used for comparison to other previously published articles, and mRECIST is advised for the assessment of hypervascular liver metastases. Imaging evaluation was performed by three experienced physicians. The largest diameter in axial plane of two representative intrahepatic target lesions was selected on baseline imaging, one in each lobe in the case of a whole liver treatment or one in different liver segments in case of a lobar treatment, thus representing the whole treated intrahepatic tumour load. Objective response rate (ORR) was defined as complete response (CR) plus partial response (PR). Disease control rate (DCR) was defined as CR, PR plus stable disease (SD).
Secondary outcome parameters included clinical response (improvement of symptoms) and clinical toxicities (adverse events) within 3 months, and within 6 months after treatment. Biochemical and haematological toxicities at 4–8 weeks and at 3 months were assessed according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.03 [17]. To assess overall survival (OS), date of death or date of last contact (when lost to follow up) was collected and as OS might be influenced by treatments following radioembolization, additional treatments following radioembolization were collected as well. Progression-free survival (PFS) analysis was not reliable in this retrospective series.
Statistical Analysis
Survival curves were estimated using the Kaplan–Meier method and assessed with the log-rank test. The following variables were tested: tumour origin, NEN grade, Ki67 index, mitotic count, tumour differentiation, number of intrahepatic lesions, intrahepatic tumour load, resection of the primary tumour, the presence of extrahepatic disease at time of treatment, LSF based on 99mTc-MAA and elevated bilirubin levels at baseline. On the basis of the current literature, the following variables were studied for their value in predicting longer OS: NEN grade, elevated bilirubin levels, intrahepatic tumour load, the presence of extrahepatic disease, LSF, DCR according to RECIST after radioembolization [11, 18,19,20,21,22,23]. Continuous variables of intrahepatic tumour load (≥ 75% vs. < 75%) [20] and LSF (≤ 10% vs. > 10%) [18] were dichotomized in order to test the influence on OS from radioembolization. Variables that were not significant in univariate Cox regression analyses were not excluded for multivariate analyses. Therefore, we started with all preselected variables and subsequently eliminated the variables by backwards selection with a threshold p value of 0.20. Of all analyses, 95% confidence intervals (95% CI) [lower–upper boundaries] were reported. p values smaller than 0.05 were considered significant in all tests. The database was analysed using IBM SPSS statistics for Windows version 23.0 (IBM, Armonk, NY).
Results
Two hundred and forty-four patients were included in this retrospective analysis and treated between July 2004 and May 2016. Twenty-four patients received multiple radioembolization treatments (up to four treatments), of which only the first treatment was analysed. Patient demographics and baseline characteristics are shown in Table 1. Prior to radioembolization, 91% had progressive disease, clinically (increase in symptoms or tumour marker) or on imaging. Most patients had diffuse liver metastases (Table 2) [3, 5]. Median time to radioembolization after diagnosis was 4.0 years (range 75 days–33 years).
At 3 months, all 244 patients had follow-up imaging and 47.5% had multiphase contrast-enhanced imaging. At 6 months, follow-up imaging was available in 51.6% and multiphase contrast-enhanced imaging in 28.7%. Pre-treatment and follow-up imaging was performed with contrast-enhanced CT in 190 patients and with gadolinium enhanced MRI in 54 patients.
Treatments received after radioembolization are summarized in Supplemental Table 2. Follow-up period for available clinical data ranged from 51 days (patient lost to follow-up) to 12 years (patient alive at time of analysis). At time of analysis, 128/244 (52.5%) patients had died.
Procedure Details
No extrahepatic depositions of 99mTc-MAA were found. Median LSF was 5.6% (range 0.7–33%), with just one patient having an LSF exceeding 20% (i.e. 33%), who received a whole liver treatment in one session without an activity reduction. He did not develop a radiation pneumonitis afterwards. Median net administered 90Y activity was 1.8 GBq and mostly calculated by the body surface area (BSA) method (Table 2).
Efficacy
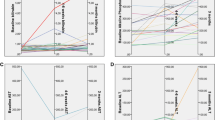
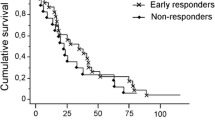
DCR of > 90% was observed at 3 and 6 months follow-up (Table 3). Achieved response rates after treatment according to both RECIST 1.1 and mRECIST are not correlated to NEN grade (Fig. 1). A similar figure arises when looking at the most common primary tumour origins. Figure 2 depicts the changes in response assessments over time between the assessment at 3 versus 6 months, which improves in 20–26% of patients in time.
Distribution of response 3 months and 6 months after radioembolization according to RECIST 1.1 and mRECIST per NEN grade. A RECIST 1.1 after 3 months (n = 244), B mRECIST after 3 months (n = 126), C RECIST 1.1 after 6 months (n = 116), D mRECIST after 6 months (n = 70). mRECIST measured in patients with available multiphased contrast-enhanced imaging at baseline and follow-up. RECIST 1.1 shows mainly stable disease, whereas mRECIST shows more objective response in all NEN grades compared to RECIST 1.1
Changes in objective response in time. Response assessment 3 months (X-axis) and 6 months (Y axis) after radioembolization. A Response assessment according to RECIST 1.1 in 116/244 patients. B Response assessment according to mRECIST in 70/244 patients. Most patients show a durable response (grey area). Just several patients show a poorer response after 6 months compared to the 3 months assessment (orange area; A 6/166 = 4%; B 5/70 = 7%). Remarkably, in a relatively large number of patients an increase in objective response can be noticed after 6 months compared to the 3 months assessment (green area; A 23/116 = 20%; B 18/70 = 26%)
Of all patients, 60% had malignancy-related symptoms prior to radioembolization; mainly flushing (43%) and diarrhoea (40%). Clinical response defined as improvement and complete resolution of pre-treatment complaints occurred in 44% and 35%, respectively. After radioembolization, 21% remained symptomatic after radioembolization.
Clinical Toxicity
Complications related to the angiography procedure itself were arterial dissection in two patients (0.8%). During 90Y resin microsphere administration, three patients experienced complaints necessitating early cessation of administration (Table 2).
Three and six months after radioembolization, no clinical toxicities occurred in 32% and 55% of patients, respectively. Known radioembolization-related adverse events occurred in 56% within the first 3 months (fatigue 28%, abdominal pain 27% and nausea 23%) and persisted in 6% at 6 months (mainly abdominal pain). Unfortunately, clinical toxicities were not registered by the treating physician in 12% and 39% of patients, at 3 and 6 months, respectively (missing data).
Radioembolization-specific complications occurred in < 4%. Radiation-induced gastric ulcer occurred in seven patients (2.8%; all seven had endoscopy, four of which had histological confirmation with biopsy), radioembolization-induced liver disease (REILD) in two patients (0.8%), radiation pneumonitis in one patient (0.4%; with a 99mTc-MAA LSF of 3.1%), liver abscess in one patient (0.4%) with bilioenteric anastomosis (without antibiotic prophylaxis) and cholangitis in one patient (0.4%) with bilioenteric anastomosis (without antibiotic prophylaxis).
Biochemical and Haematological Toxicity
New CTCAE grade 3–4 biochemical and haematological toxicities were limited; most common was lymphocytopenia in 6.7%. Grade 1–2 biochemical toxicities were encountered in up to 51%; however, grade 1–2 bilirubin elevation and/or decreased albumin levels occurred in 6%. Apart from an incidence of grade 1–2 lymphocytopenia in 52%, thrombocytopenia occurred in 17%, and a grade 1–2 anaemia or leukopenia occurred in < 8%. Coagulation was unaffected as measured by the international normalized ratio (INR).
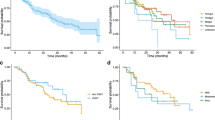
Overall Survival
Median OS after radioembolization for the entire population was 2.6 years (range: 51 days–12 years) [95% CI 2.2–3.0 years]. Median OS in G1NET and G2NET was significantly longer than in G3NET/NEC in the Kaplan–Meier analysis (p < 0.001). Median OS was 3.1 years [95% CI 2.6–3.7] in G1NET, 2.4 years [95% CI 1.9–3.0] in G2NET and 0.9 years [95% CI 0.1–1.9] in G3NET/NEC (Fig. 3A).
Kaplan–Meier analyses identified Ki67, intrahepatic tumour load ≥ 75% and the presence of extrahepatic disease as significant negative prognostic factors for OS (all p < 0.003; Fig. 3B–D). In the Kaplan–Meier analyses, OS was independent of tumour origin (also when stratified by tumour grade), tumour differentiation, mitotic count, number of intrahepatic lesions, resection of the primary tumour, LSF based on 99mTc-MAA and elevated bilirubin levels at baseline.
DCR and ORR according to either RECIST 1.1 (p = 0.001 and p = 0.032, respectively; Fig. 4A, B) or mRECIST (p = 0.002 and p = 0.007, respectively; Fig. 4C, D) after 3 months showed a longer survival. The same was seen after 6 months (p < 0.01 in all four categories). Patients experiencing improvement or resolution of pre-treatment symptoms had no significant improved OS (p = 0.85).
In the multivariate analysis, DCR according to RECIST 1.1 at 3 months was predictive of a better OS (hazard ratio; HR 0.4; p < 0.01), whereas G3NET/NEC (HR 3.3; p < 0.01), unknown NEN grade (HR 1.7; p = 0.03), ≥ 75% intrahepatic tumour load (HR 2.2; p < 0.01) and the presence of extrahepatic disease (HR 1.7; p = 0.04) were predictive of a worse OS (Table 4).
Discussion
In this study, the efficacy of radioembolization of neuroendocrine liver metastases was confirmed with high DCR > 90%, concordant between the two radiologic response assessment criteria (RECIST 1.1 and mRECIST), and a long median OS of 2.6 years (i.e. 31 months) for the entire study population. This is the first time a prolonged response for at least 6 months has been objectively demonstrated in patients with available imaging after 6 months and in approximately one-quarter of those patients, the optimal time to evaluate treatment might be later than 3 months (Fig. 2). Additionally, a high percentage of patients benefited from improvement (44%) or complete resolution (35%) of their malignancy-related symptoms, an important finding in this specific patient population.
Compared to a recent meta-analysis by Devcic et al. and other more recently published studies in the period of 2015–2016, radioembolization in NEN shows consistent results, with a median OS ranging between 24.7 and 39.0 months and a DCR of between 83 and 94% according to either RECIST 1.1 or mRECIST, in line with the 31 months [95% CI 26–36] and DCR of 91% according to either RECIST 1.1 or mRECIST in the presented population [11, 18, 20, 24].
This study addressed several shortcomings of the current literature on radioembolization in NEN, by analysing all available retrospective data. The current literature consists of small single-centre patient cohorts only, except for one large retrospective study by Kennedy et al. with 148 NEN patients [22, 25]. As stated by Devcic et al., including the study by Kennedy et al., most studies described a heterogeneous group of NEN patients and lacked proper baseline parameter description [11]. A major limitation of prior published cohorts was the lack of data referring to the NEN histopathological characteristics, especially NEN grading according to the current WHO/ENETS classification, and its effect on tumour response and survival. ORR and DCR in this study are independent of the NEN grade (Fig. 1), Ki67-index, mitotic index or tumour differentiation, and NEN grade is a prognostic factor for OS. Previously published data suggest a poorer response rate for patients with pancreatic NEN [11]. However, in accordance with three other studies, no significant difference in survival was observed between different origins of NEN (p > 0.3) [18, 20, 21]. The present study does confirm that the presence of extrahepatic disease is a significant factor for poorer survival [22, 26, 27]. Comparable to most other studies, a poorer OS with an intrahepatic tumour load ≥ 75% was found (p < 0.01) [20].
Radioembolization has some benefits over other liver-directed treatments in NEN, of which trans-arterial (bland) embolization (TAE) and trans-arterial chemoembolization (TACE) are most commonly applied. To date, only one retrospective study addresses the differences [23]. In that study, radioembolization resulted in a similar hepatic PFS (15.7 months) compared to TAE (15.0 months), while achieving a significantly longer hepatic PFS compared to TACE (8.1 months). However, a significantly higher number of patients experienced abdominal pain after TAE compared to either radioembolization or TACE. On the other hand, radioembolization showed more biochemical toxicities compared to TAE and TACE. However, the total number of severe toxicities between radioembolization, TAE and TACE was similar [23]. The percentage of total clinical toxicities in the radioembolization group of that study (85%) was higher than the current study (56%), while severe biochemical toxicities were similar (7.5% vs. 7%) [23]. Compared to TAE and TACE, lately some concerns have been risen on the late onset cirrhosis after radioembolization [28]. With our limited follow-up of 6 months, we could not investigate this phenomenon. Other radioembolization-induced complications were limited (< 4%). REILD and gastric ulceration were consistent with other studies in different disease groups [29]. One patient received a whole liver treatment without dose reduction, while having a LSF of 33%. On planar imaging, a lot of free pertechnetate could be acknowledged and 99mTc-MAA is known to significantly overestimate LSF [30]. Based on these findings, LSF was recalculated on SPECT/CT, which was 7.8%, and patient was treated without a dose reduction.
This study has several limitations because of its retrospective design. Some histopathological characteristics could not be obtained for some patients, because the WHO/ENETS classification was not reported by pathologists before its introduction in 2011. Retrospective review of medical records did not allow comprehensive CTCAE grading of clinical toxicities and incorporated a reporting bias by the treating physician. PFS could not be measured reliably in this retrospective series since follow-up imaging intervals were not standardized across all centres. Follow-up was limited to 6 months after treatment in this cohort as most patients went on to receive subsequent treatment even before intrahepatic PD was documented according to either RECIST 1.1 or mRECIST, while some other patients were lost to follow-up after the first- or second-response assessment. Patients lost to follow-up and subsequent treatments prior to intrahepatic PD after radioembolization made imaging and toxicity follow-up beyond 6 months unreliable. If patients received a new treatment within the 6-month follow-up, patients were excluded to avoid contamination of toxicity and imaging response data. Not all centres acquired post-treatment imaging, making dosimetric evaluation impossible, and half of patients had no multiphasic imaging after treatment to assess response according to mRECIST. In recent years, a lot has changed in treatment of NEN patients, so treatment sequencing is different in the patients evaluated in this study, making these results more difficult to interpret. Additionally, radioembolization was performed relatively late in the treatment regimen of patients, negatively influencing the reported OS after radioembolization.
Prospective randomized controlled studies on radioembolization in NEN are desperately needed, although it should also be recognized that clinical experience, captured in high-quality retrospective study cohorts, is indispensable in this difficult-to-study heterogeneous patient population. Currently, treatment algorithms typically place radioembolization after failure of systemic treatments [3]. However, in NEN patients with disease limited or ‘dominant’ to the liver, radioembolization might be a more appropriate choice prior to, or in combination with first-line systemic treatment. Future studies need to address the sequencing of radioembolization along or amongst other treatment (systemic) options, like peptide receptor radionuclide therapy (PRRT) or chemotherapy consisting of capecitabine + temozolomide (CAPTEM) in first or second line, and have longer follow-up after treatment [31, 32]. Technical advances in radioembolization should lead to better treatment planning and dosimetry in eligible patients, which may improve ORR and OS [33,34,35]. Currently literature on dosimetry in NEN is limited. Based on 99mTc-MAA SPECT/CT, a mean tumour absorbed dose of > 190 Gy with 90Y resin microspheres has been suggested to predict tumour response with high specificity [36]. Dosimetry is of particular importance for future studies. The combination of a relatively favourable prognosis with lifestyle-limiting symptomatic disease in NEN patients favours quality of life as an important endpoint [37,38,39]. Quality of life indices should definitely be included in future studies as well.
Conclusion
In a broad spectrum of NEN and at different moments of the disease, radioembolization is safe, effective and can relieve symptoms, even in heavily pre-treated, progressive patients with high intrahepatic tumour load. In one-fourth of patients, objective response might improve after the commonly used 3-month evaluation scan.
References
Heetfeld M, Chougnet CN, Olsen IH, et al. Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer. 2015;22(4):657–64. https://doi.org/10.1530/ERC-15-0119.
Rindi G, Petrone G, Inzani F. The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endcr Pathol. 2014;25(2):186–92. https://doi.org/10.1007/s12022-014-9313-z.
Pavel M, Baudin E, Couvelard A, et al. ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology. 2012;95(2):157–76. https://doi.org/10.1159/000335597.
Lawrence B, Gustafsson BI, Chan A, et al. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am. 2011;40(1):1–18. https://doi.org/10.1016/j.ecl.2010.12.005.
Frilling A, Li J, Malamutmann E, Schmid KW, et al. Treatment of liver metastases from neuroendocrine tumours in relation to the extent of hepatic disease. Br J Surg. 2009;96(2):175–84. https://doi.org/10.1002/bjs.6468.
Strosberg JR, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Eng J Med. 2017;376(2):125–35. https://doi.org/10.1056/NEJMoa1607427.
Yao JC, Fazio N, Singh S, et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387:968–77. https://doi.org/10.1016/S0140-6736(15)00817-X.
Caplin ME, Pavel M, Ćwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Eng J Med. 2014;371(3):224–33. https://doi.org/10.1056/NEJMoa1316158.
Raymond E, Dahan L, Raoul JL, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Eng J Med. 2011;364(6):501–13. https://doi.org/10.1056/NEJMoa1003825.
Frilling A, Modlin IM, Kidd M, et al. Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol. 2014;15(1):e8–21. https://doi.org/10.1016/S1470-2045(13)70362-0.
Devcic Z, Rosenberg J, Braat AJAT, et al. The efficacy of hepatic 90Y resin radioembolization for metastatic neuroendocrine tumors: a meta-analysis. J Nucl Med. 2014;55(9):1404–10. https://doi.org/10.2967/jnumed.113.135855.
Kennedy AS, Bester L, Salem R, et al. Role of hepatic intra-arterial therapies in metastatic neuroendocrine tumours (NET): guidelines from the NET-Liver-Metastases Consensus Conference. HBP (Oxford). 2015;17(1):29–37. https://doi.org/10.1111/hpb.12326.
Lam MGEHLJ, Iagaru AH, Goris ML, Sze DY. Safety of repeated yttrium-90 radioembolization. Cardiovasc Intervent Radiol. 2013;36(5):1320–8. https://doi.org/10.1007/s00270-013-0547-9.
Salem R, Lewandowski RJ, Gates VL, et al. Research reporting standards for radioembolization of hepatic malignancies. J Vasc Interv Radiol. 2011;22(3):265–78. https://doi.org/10.1016/j.jvir.2010.10.029.
Response Evaluation Criteria In Solid Tumors. www.recist.com. Accessed March 2016.
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60.
USA NCI. Common terminology criteria in adverse events, version 4.03 (CTCAE v4.03). NIH. 2010. http://www.hrc.govt.nz/sites/default/files/CTCAE%20manual%20-%20DMCC.pdf. Accessed March 2016.
Ludwig JM, Ambinder EM, Ghodadra 3, et al. Lung shunt fraction prior to yttrium-90 radioembolization predicts survival in patients with neuroendocrine liver metastases: single-center prospective analysis. Cardiovasc Intervent Radiol. 2016;39(7):1007–14. https://doi.org/10.1007/s00270-016-1323-4.
Sommer WH, Ceelen F, Garcia-Albeniz X, et al. Defining predictors for long progression-free survival after radioembolisation of hepatic metastases of neuroendocrine origin. Eur Radiol. 2013;23(11):3094–103. https://doi.org/10.1007/s00330-013-2925-8.
Peker A, Çiçek O, Soydal Ç, et al. Radioembolization with yttrium-90 resin microspheres for neuroendocrine tumor liver metastases. Diagn Interv Radiol. 2015;21(1):54–9. https://doi.org/10.5152/dir.2014.14036.
Singla S, LeVea CM, Pokuri VK, et al. Ki67 score as a potential predictor in the selection of liver-directed therapies for metastatic neuroendocrine tumors: a single institutional experience. J Gastrointest Oncol. 2016;7(3):441–8. https://doi.org/10.21037/jgo.2016.02.02.
Cao CQ, Yan TD, Bester L, et al. Radioembolization with yttrium microspheres for neuroendocrine tumour liver metastases. Br J Surg. 2010;97(4):537–43. https://doi.org/10.1002/bjs.6931.
Chen JX, Rose S, White SB, et al. Embolotherapy for neuroendocrine tumor liver metastases: prognostic factors for hepatic progression-free survival and overall survival. Cardiovasc Intervent Radiol. 2017;40(1):69–80. https://doi.org/10.1007/s00270-016-1478-z.
Barbier CE, Garske-Román U, Sandström M, et al. Selective internal radiation therapy in patients with progressive neuroendocrine liver metastases. Eur J Nucl Med Mol Imaging. 2016;43(8):1425–31. https://doi.org/10.1007/s00259-015-3264-6.
Kennedy AS, Dezarn WA, McNeillie P, et al. Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. Am J Clin Oncol. 2008;31(3):271–9. https://doi.org/10.1097/COC.0b013e31815e4557.
Saxena A, Chua TC, Bester L, et al. Factors predicting response and survival after yttrium-90 radioembolization of unresectable neuroendocrine tumor liver metastases: a critical appraisal of 48 cases. Ann Surg. 2010;251(5):910–6. https://doi.org/10.1097/SLA.0b013e3181d3d24a.
Ozao-Choy J, Friedman ML, Kim AS, et al. Radioembolization for treatment of liver metastases from neuroendocrine tumors: correlation with imaging and biomarkers. Pancreas. 2013;42(2):358–60. https://doi.org/10.1097/MPA.0b013e31825f4087.
Tomozawa Y, Jahangiri Y, Pathak P, Kolbeck KJ, Schenning RC, Kaufman JA, Farsad K. Long-term toxicity after transarterial radioembolization with yttrium-90 using resin microspheres for neuroendocrine tumor liver metastases. J Vasc Interv Radiol. 2018;29(6):858–65. https://doi.org/10.1016/j.jvir.2018.02.002.
Kennedy AS, McNeillie P, Dezarn WA, et al. Treatment parameters and outcome in 680 treatments of internal radiation with resin 90Y-microspheres for unresectable hepatic tumors. Int J Radiat Oncol Biol Phys. 2009;74(5):1494–500. https://doi.org/10.1016/j.ijrobp.2008.10.005.
Elschot M, Nijsen JF, Lam MGEH, et al. (99m)Tc-MAA overestimates the absorbed dose to the lungs in radioembolization: a quantitative evaluation in patients treated with 166Ho-microspheres. Eur J Nucl Med Mol Imaging. 2014;41(10):1965–75. https://doi.org/10.1007/s00259-014-2784-9.
Soulen MC, van Houten D, Teitelbaum UR, Damjanov N, Cengel KA, Metz DC. Safety and feasibility of integrating yttrium-90 radioembolization with capecitabine-temozolomide for grade 2 liver-dominant metastatic neuroendocrine tumors. Pancreas. 2018;47(8):980–4.
Braat AJAT, Kwekkeboom DJ, Kam BLR, et al. Additional hepatic 166Ho-radioembolization in patients with neuroendocrine tumours treated with 177Lu-DOTATATE; a single center, interventional, non-randomized, non-comparative, open label, phase II study (HEPAR PLUS trial). BMC Gastroenterol. 2018;18(1):84. https://doi.org/10.1186/s12876-018-0817-8.
Mikell JK, Mahvash A, Siman W, et al. Selective internal radiation therapy with yttrium-90 glass microspheres: biases and uncertainties in absorbed dose calculations between clinical dosimetry models. Int J Radiat Oncol Biol Phys. 2016;96(4):888–96. https://doi.org/10.1016/j.ijrobp.2016.07.021.
Garin E, Lenoir L, Edeline J, et al. Boosted selective internal radiation therapy with 90Y-loaded glass microspheres (B-SIRT) for hepatocellular carcinoma patients: a new personalized promising concept. Eur J Nucl Med Mol Imaging. 2013;40(7):1057–68. https://doi.org/10.1007/s00259-013-2395-x.
Smits MLJ, Elschot M, Sze DY, et al. Radioembolization dosimetry: the road ahead. Cardiovasc Intervent Radiol. 2015;38(2):261–9. https://doi.org/10.1007/s00270-014-1042-7.
Chansanti O, Jahangiri Y, Matsui Y, et al. tumor dose response in yttrium-90 resin microsphere embolization for neuroendocrine liver metastases: a tumor-specific analysis with dose estimation using SPECT-CT. J Vasc Interv Radiol. 2017;28(11):1528–35. https://doi.org/10.1016/j.jvir.2017.07.008.
Fidelman N, Kerlan RK Jr, Hawkins RA, et al. 90Y glass microspheres for the treatment of unresectable metastatic liver disease from chemotherapy-refractory gastrointestinal cancers: a pilot study. J Gastrointest Cancer. 2014;45(2):168–80. https://doi.org/10.1007/s12029-013-9566-7.
Turkmen C, Ucar A, Poyanli A, et al. Initial outcome after selective intraarterial radionuclide therapy with yttrium-90 microspheres as salvage therapy for unresectable metastatic liver disease. Cancer Biother Radiopharm. 2013;28(7):534–40. https://doi.org/10.1089/cbr.2012.1455.
Cramer B, Xing M, Kim HS. prospective longitudinal quality of life assessment in patients with neuroendocrine tumor liver metastases treated with 90Y radioembolization. Clin Nucl Med. 2016;41(12):e493–7. https://doi.org/10.1097/RLU.0000000000001383.
Funding
Travel expenses and accommodations of AJATB were partially covered by Sirtex Medical Europe, producer of SIR-spheres. Remaining travel expenses were granted by the Girard de Mielet van Coehoorn Foundation (Grant of the Board of Directors UMC Utrecht, the Netherlands). Both parties have no access to the data and have not been involved in data analysis or in the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.M.D. has acted as a consultant for Sirtex, Bayer Healthcare and Ipsen. A.F. receives research funding from Ipsen, Novartis and Sirtex Medical. D.B.B is a consultant for BTG, receives research funding from Sirtex and has served on a speaker’s bureau for Boston Scientific. D.Y.S. has acted as consultant for BTG, Boston Scientific, Amgen, EmbolX and Viralytics. M.G.E.H.L. has acted as a consultant for BTG, Sirtex, Mirada and Bayer Healthcare. All other authors have no conflicts of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Braat, A.J.A.T., Kappadath, S.C., Ahmadzadehfar, H. et al. Radioembolization with 90Y Resin Microspheres of Neuroendocrine Liver Metastases: International Multicenter Study on Efficacy and Toxicity. Cardiovasc Intervent Radiol 42, 413–425 (2019). https://doi.org/10.1007/s00270-018-2148-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2148-0