Abstract
Purpose
This multicenter phase I/II study evaluated the safety, feasibility, and initial efficacy of radiofrequency ablation (RFA) for small malignant renal tumors.
Methods
Thirty-three patients were enrolled in the study. A single session of RFA was performed in patients with a renal tumor of 1–3 cm in greatest diameter, with the exception of lesions adjacent to the renal hilum. The primary endpoint was the safety of renal RFA, and the secondary endpoints were its feasibility and initial efficacy for local control, as well as the incidence and grade of adverse events. Clinical efficacy was evaluated by CT scans within 1 week and at a further 4 weeks after the procedure using the criteria adapted from the Response Evaluation Criteria in Solid Tumors.
Results
The RFA procedure was completed in 100 % (95 % confidence interval [CI] 89–100 %) of all 33 patients. There were no severe adverse events (0 % [95 % CI 0–11 %]). Among the 33 patients, a complete response, partial response, progressive disease, and stable disease were seen in 28 (85 %), 0 (0 %), one (3 %), and one (3 %) patient(s), respectively, with a tumor response rate of 85 % [95 % CI 68–95 %]). Three patients (9 %), including one ineligible patient (3 %), were not evaluable. Out of 30 evaluable patients, a complete response was achieved in 28 (93 %).
Conclusion
The current multicenter trial revealed that RFA is a safe, feasible, and effective treatment for small malignant renal tumors in patients who are not candidates for surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current gold standard therapy for small RCC is partial nephrectomy. Because of its minimally invasive character, radiofrequency ablation (RFA) and cryoablation are options reserved for patients who are not candidates for surgery because of comorbidity or refusal [1–5]. Reliable evidence on the effectiveness of the treatment is still lacking as most previously published reports on renal RFA were retrospective studies, comprehensive reviews, and meta-analyses of case series. Multicenter prospective studies have not been reported regarding the evaluation of renal RFA. Therefore, we undertook a phase I/II multi-institutional prospective study of renal RFA, the Japan Interventional Radiology in Oncology Study Group (JIVROSG) Study 0701. Its objective was to evaluate the safety, feasibility, and initial efficacy of renal RFA in patients with small malignant renal tumors.
Materials and Methods
Patient Selection
This study was approved by the institutional review board at each institution. Inclusion criteria were: malignant renal tumors confirmed pathologically, or by course and diagnostic imaging; tumors that were 1–3 cm in greatest diameter; tumors with increased attenuation of ≥20 HU on CT scan after intravenous administration of contrast media; patients in whom surgical resection was out of indication or not desired; adequate major organ function defined as a white blood cell count of 3000/μL or higher, a platelet count of 100,000/μL or higher, a hemoglobin level of 8.0 g/dL or higher, creatinine clearance of 50 mL/min or higher, and serum bilirubin of 2.0 mg/dL or lower; age ≥20 years when informed consent was obtained; Eastern Cooperative Oncology Group performance status of 0–2; and life expectancy of at least 2 months.
Exclusion criteria included: patients with a cardiac pacemaker; definite existence of arteries, nerves, or ureters on the root of an electrode seen on imaging; a target lesion adjacent to the renal hilum, or difficulty in advancing an electrode without passing though the renal hilum or gastrointestinal tract; difficulty in measuring the diameter of the lesion on CT; a definite bleeding disorder; treatment with an antiplatelet agent, thrombolytic agent, or anticoagulant therapy that could not be discontinued; a history of allergy to contrast media; active infection; active inflammation; a fever temperature of ≥38 °C; multiple renal tumors, for which additional treatment could not be extended beyond 4 weeks after RFA; chemotherapy or immunotherapy that could not be discontinued at 4 weeks before registration to a CT study and at 4 weeks after the protocol treatment; previous local treatment; and pregnancy or suspected pregnancy. Any patients who were deemed otherwise unsuitable for the study by the investigator were excluded.
Percutaneous renal needle biopsy was recommended before or during the procedure, but it was not mandatory.
Renal RFA Procedures
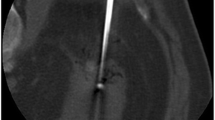
A 17-gauge Cool-tip electrode (Valleylab, Boulder, CO, USA) or a 14-gauge LeVeen electrode (Boston Scientific, Natick, MA, USA) was selected based on user preference. Under conscious sedation, patients were placed on the table. Local anesthesia was performed for skin and subcutaneous tissue on the puncture line. The image guidance modality was not specified in the protocol. A radiofrequency (RF) electrode was advanced to the tumor. After confirmation that the RF electrode had been placed inside the target tumor, the RF application was performed using a RF generator (Cool-tip RF, Valleylab; RF 3000, Boston Scientific). For the Cool-tip RF system, based on 12 min of energy application in the impedance control mode for applying energy to one site, ablation was complete when the temperature of the tip of the needle electrode was at least 60 °C at the completion of energy application. For the RF 3000 system, based on whether there were roll-offs (the phenomenon of the impedance increasing to an infinitely large degree and output decreasing to 0 Watts) or 15 min of continuous energy application, ablation was complete at one energy application site when there were two roll-offs, 15 min of continuous energy application and one roll-off, or two 15-min periods of continuous energy application. If the tumor was not covered by the ablated area of one ablation site, the electrode was repositioned and ablation was repeated as described above.
Study Endpoints and Study Design
This study was a multi-institutional, single-arm, open-label, noncomparative trial. The primary endpoint was the safety of renal RFA, and the secondary endpoints were its feasibility and initial efficacy in local tumor control, as well as the incidence and grade of adverse events. The phase I component of this trial was conducted in nine patients using the three-by-three method proposed by the JIVROSG, which has been described in detail previously [6]. In brief, this is a step-by-step safety evaluation of the first nine patients divided into three cohorts. The first cohort is treated and evaluated for the occurrence of severe adverse events. If they occur in one patient or less during the observation period of 4 weeks, the next cohort is treated, followed by the next observation period of 4 weeks, and finally, the third cohort of three patients is treated. This method was developed to assure the safety of a new interventional procedure. In the phase II component of this study, 24 patients were enrolled.
Evaluation of safety involved confirmation of the incidence of severe adverse events that corresponded to grade 4 or 5 according to the Common Terminology Criteria for Adverse Events (CTCAE) version 3.0 [7], or equivalent to these grades; an incidence of <34 % severe adverse events among all enrolled cases was considered to be acceptable safety. The incidence and severity of the adverse events were calculated in all patients who underwent at least part of the protocol treatment. The incidence of adverse events and each grade, based on the worst grade, for the patients were recorded.
The feasibility of the procedure was measured together with the rate of protocol completion in all enrolled patients. Tumor response rates were calculated from all enrolled patients and eligible patients. Patients underwent an abdominal CT study in which pre- and post-contrast arterial and equilibrium phases with axial images of 5-mm slice thickness were obtained within 4 weeks before registration, and within 1 week after completion of the procedure as the first post-procedure CT scan. The second post-procedure CT scan was obtained at a further 4 weeks after the first post-procedure CT scan. The efficacy was evaluated with tumor response rate, namely complete response (CR) or partial response (PR) using our criteria (Table 1) adapted from the Response Evaluation Criteria in Solid Tumors (RECIST) criteria [8]. In the current study, the target lesion was limited to one renal tumor undergoing treatment, and tumor response of the viable target lesion was evaluated. Viable lesion was defined as the site showing contrast enhancement of at least 20 HU on a contrast-enhanced CT scan. CT images were evaluated based on central review to minimize bias by at least three committees who had had their board certification of diagnostic radiology approved by the Japan Radiological Society.
Overall survival was calculated using a Kaplan–Meier analysis in which the survival of patients was evaluated at the time of analysis.
Statistical Analysis
According to the three-by-three method proposed by the JIVROSG, in the phase I component of the trial, a cohort size of nine patients was considered to be adequate to terminate the study if the incidence of severe adverse events associated with the procedure exceeded one-third of the patient population [6]. During phases I and II, the study was designed to detect the incidence of adverse events, set at 10 % for the lowest rate, 10 % for the predicted rate, and 30 % for the unacceptable rate, with a power of 80 %. Since a protocol dropout rate of 10 % was anticipated, the target accrual number of patients was calculated to be 33. All enrolled patients were included in the intention-to-treat analyses for evaluation of safety, feasibility, and initial efficacy. This study was registered under Clinical Trials Registry, number UMIN000001123 (www.umin.ac.jp/ctr/index.htm).
Results
The registration period extended from April 2008 until August 2010. Patients were enrolled from eight institutions that were participating in the JIVROSG (Supplementary Table S1). There was no report of a severe adverse event corresponding to grade 4 or 5 during phase I, and the study therefore proceeded to phase II. Patient characteristics are listed in Table 2. One patient had a renal tumor located adjacent to the renal hilum; this met the exclusion criteria, but RFA treatment was mistakenly performed. The numbers of all eligible patients and patients for whom protocol treatment was performed were 32 and 33, respectively.
Results of Biopsy
Percutaneous renal biopsy was performed in 31 patients, although it was not mandatory. Biopsy data are detailed in Table 3. Among the 31 patients, a pathologic diagnosis of RCC was made in 28 patients. In the other three patients, the specimen obtained by biopsy was not sufficient for a pathological diagnosis to be made. As a result, no tumor was diagnosed as a benign renal tumor or other type of malignant renal tumor. In five patients, diagnosis of malignant renal tumors was made using CT imaging.
RFA Procedures
RFA procedures, including RF electrode insertion into the target renal tumors and ablation according to the protocol, were completed in all (100 % [95 % confidence interval [CI], 89–100 %]) of 33 cases. The ablation parameters are summarized in Table 4.
Adverse Events
The procedure was well tolerated by all 33 patients. No grade 4 or 5 adverse event (0 % [95 % CI 0–11 %]) occurred. The adverse events using CTCAE version 3.0 classifications are summarized in Table 5. A total of 59 adverse events were seen in 29 (88 % [95 % CI 72–97 %]) out of the 33 patients.
Efficacy
Data regarding the evaluation of tumor response for a target lesion are detailed in Table 6. A tumor response rate, which was equal to a CR rate, was 85 % (95 % CI 68–95 %) among all 33 enrolled patients and 88 % (95 % CI 71–97 %) among 32 eligible patients. One patient was deemed as ineligible, who had a renal mass adjacent to the renal hilum. Three patients whose imaging studies were not completed were deemed as not evaluable, including one ineligible patient. A CR was achieved in 28 (93 %) out of 30 evaluable patients.
Survival
No deaths occurred within 1 month after the RFA procedure. Two patients died during the follow-up period; their deaths were not related to the RFA procedure. One patient died from shock of unknown etiology during CT-guided lung biopsy at 247 days after the RFA procedure. The patient exhibited hypotension and bradycardia after removal of the biopsy needle, resulting in cardiac arrest. He could not be resuscitated, although cardiopulmonary resuscitation was provided. The other patient who underwent RFA for a metastatic RCC died of primary disease at 383 days after the procedure. Patient survival was evaluated at a mean follow-up time of 442 (range, 127–731) days (SD, 150 days). One- and 2-year overall survival rates were 97 % (95 % CI 91–103 %) and 92 % (95 % CI 81–103 %), respectively (Fig. 1).
Discussion
In the literature, the complication rate for renal RFA in larger (at least 70 cases), observational, noncomparative series ranges from 4–13 % [1–5]. This broad range of complication rates may reflect the lack of a standard definition of complications due to the studies being retrospective. Reported early complications included perirenal hematoma, thermal injury to the bowel, urinoma, perirenal abscess, pneumothorax, pneumonia, neuropathic pain, hydronephrosis, and others [1–5]. In the current study, the RFA treatment protocol was completed in all 33 patients without severe adverse events corresponding to grade 4 or 5. These results suggest that the protocol treatment was safe and feasible.
Gervais et al. [1] reported that complete necrosis of a renal tumor of ≤3 cm in diameter was achieved in 48 (92 %) of 52 tumors after a single ablation session of renal RFA. Both small size (≤3 cm) and a noncentral location proved to be independent predictors of complete necrosis after a single ablation session. Breen et al. [3] performed RF ablation on 105 renal tumors in 97 patients, with a mean tumor size of 32 mm (11–68 mm). Eighty-three tumors were completely treated in a single session (79 %). Tumor size was the only predictor of procedure outcome, with tumors of ≤3 cm in size being associated with complete treatment in a single ablation session. As mentioned above, in the literature, tumor size and location seem to be significant predictive factors in achieving complete necrosis of the tumor after a single RFA session. This was the reason why we excluded tumors that were >3 cm in size and had a central location from the inclusion criteria. In the current study, out of 30 evaluable patients, CR was achieved in 28 (93 %). Our results were comparable with the initial success rates of the previous retrospective reports, even though our study was a prospective multicenter trial.
In the literature, RECIST has not yet been used in evaluation of renal RFA, although standard methods of response assessment have been required to compare treatment options. The concepts of our evaluation criteria are analogous to those of modified RECIST (mRECIST) [9, 10]. Regarding the evaluation of hepatocellular carcinoma, recent studies have found a poor correlation between the extent of tumor necrosis induced by interventional procedures and RECIST [10]. Edeline et al. [11] mentioned that mRECIST should be used as the standard assessment for treatment efficacy with regard to hepatocellular carcinoma. As for RCC, any area exhibiting contrast enhancement within the ablation zone is conventionally regarded as residual unablated tumor or local tumor progression. Therefore, mRECIST provides appropriate criteria to evaluate the therapeutic effects of renal RFA; however, mRECIST had not yet been published when we completed the study protocol. In the current study, a viable lesion was defined as a site showing contrast enhancement of at least 20 HU on a contrast-enhanced CT scan. Enhancement on dual-phase CT has classically been defined as an increase in attenuation of >10 HU between the unenhanced and enhanced phases. However, because of the greater frequency of pseudoenhancement effects seen with multi-detector row CT than with single-detector CT, this threshold has lost specificity and ≥20 HU is now the more common definition [12, 13].
The limitations of the current trial include the small number of patients enrolled and the short follow-up time. The follow-up time using CT scan after RFA was 4–6 weeks, which is sufficient to evaluate the primary technical success and technique efficacy in an imaging study [14], but too short a time over which to evaluate the presence of subsequent local tumor progression. In the literature, most local tumor progression has been reported to be detectable within 1 year after thermal ablation [2, 15]. However, recently reported long-term outcomes showed local tumor progression with a median time to local progression of 1 to 2.5 years [16–18]. Other limitations were that one ineligible patient (3 %) was included in this study and five patients (15 %) had a renal tumor not confirmed by biopsy.
In conclusion, the current prospective multicenter trial revealed that RFA is a safe, feasible, and effective treatment for small malignant renal tumors. RFA is a promising alternative treatment for small malignant renal tumors in patients who are not candidates for surgery. A larger clinical trial with a longer follow-up is warranted.
References
Gervais DA, McGovern FJ, Arellano RS, McDougal WS, Mueller PR. Radiofrequency ablation of renal cell carcinoma: part 1, indications, results, and role in patient management over a 6-year period and ablation of 100 tumors. Am J Roentgenol. 2005;185(1):64–71.
Zagoria RJ, Traver MA, Werle DM, Perini M, Hayasaka S, Clark PE. Oncologic efficacy of CT-guided percutaneous radiofrequency ablation of renal cell carcinomas. Am J Roentgenol. 2007;189(2):429–36.
Breen DJ, Rutherford EE, Stedman B, Roy-Choudhury SH, Cast JE, Hayes MC, et al. Management of renal tumors by image-guided radiofrequency ablation: experience in 105 tumors. Cardiovasc Intervent Radiol. 2007;30(5):936–42.
Hegarty NJ, Gill IS, Desai MM, Remer EM, O’Malley CM, Kaouk JH. Probe-ablative nephron-sparing surgery: cryoablation versus radiofrequency ablation. Urology. 2006;68(1 Suppl):7–13.
Veltri A, Gazzera C, Busso M, Solitro F, Piccoli GB, Andreetto B, et al. T1a as the sole selection criterion for RFA of renal masses: randomized controlled trials versus surgery should not be postponed. Cardiovasc Intervent Radiol. 2014;37(5):1292–8.
Kobayashi T, Arai Y, Takeuchi Y, Nakajima Y, Shioyama Y, Sone M, et al. Phase I/II clinical study of percutaneous vertebroplasty (PVP) as palliation for painful malignant vertebral compression fractures (PMVCF): JIVROSG-0202. Ann Oncol. 2009;20(12):1943–7.
Cancer Therapy Evaluation Program, Common Terminology Criteria for Adverse Events Version 3.0. Available from URL: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Accessed Oct 11, 2015.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92(3):205–16.
Llovet JM, Di Bisceglie AM, Bruix J, Kramer BS, Lencioni R, Zhu AX, et al. Design and endpoints of clinical trials in hepatocellular carcinoma. J Natl Cancer Inst. 2008;100(10):698–711.
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60.
Edeline J, Boucher E, Rolland Y, Vauléon E, Pracht M, Perrin C, et al. Comparison of tumor response by response evaluation criteria in solid tumors (RECIST) and modified RECIST in patients treated with sorafenib for hepatocellular carcinoma. Cancer. 2012;118(1):147–56.
Patel J, Davenport MS, Khalatbari S, Cohan RH, Ellis JH, Platt JF. In vivo predictors of renal cyst pseudoenhancement at 120 kVp. Am J Roentgenol. 2014;202(2):336–42.
Israel GM, Bosniak MA. How I do it: evaluating renal masses. Radiology. 2005;236(2):441–50.
Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria-a 10-year update. Radiology. 2014;273(1):241–60.
Matin SF, Ahrar K, Cadeddu JA, Gervais DA, McGovern FJ, Zagoria RJ, et al. Residual and recurrent disease following renal ablative therapy: a multi-institutional study. J Urol. 2006;176(5):1973–7.
Psutka SP, Feldman AS, McDougal WS, McGovern FJ, Mueller P, Gervais DA, et al. Long-term oncologic outcomes after radiofrequency ablation for T1 renal cell carcinoma. Eur Urol. 2013;63(3):486–92.
Tracy CR, Raman JD, Donnally C, Trimmer CK, Cadeddu JA. Durable oncologic outcomes after radiofrequency ablation: experience from treating 243 small renal masses over 7.5 years. Cancer. 2010;116(13):3135–42.
Levinson AW, Su LM, Agarwal D, Sroka M, Jarrett TW, Kavoussi LR. Long-term oncological and overall outcomes of percutaneous radio frequency ablation in high risk surgical patients with a solitary small renal mass. J Urol. 2008;180(2):499–504.
Acknowledgments
This work was supported by the Health and Labour Sciences Research Grants from the Japanese Ministry of Health, Labour and Welfare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HM, KY, TM, HG, and TY reported grants from the Japanese Ministry of Health, Labour and Welfare as mentioned above during the conduct of the study. All remaining authors have declared no conflicts of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mimura, H., Arai, Y., Yamakado, K. et al. Phase I/II Study of Radiofrequency Ablation for Malignant Renal Tumors: Japan Interventional Radiology in Oncology Study Group 0701. Cardiovasc Intervent Radiol 39, 717–723 (2016). https://doi.org/10.1007/s00270-015-1275-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1275-0