Abstract
Purpose
To test the performance of an expandable bipolar probe as a simple technical solution for extending the coagulation volume.
Methods
On the basis of a commercially available monopolar radiofrequency (RF) probe (LeVeen), an expandable bipolar RF probe was developed by integrating a second electrode into the probe shaft. The influence of length on the second electrode, and the distance between both electrodes and generator output was investigated by performing ten ablations for each condition on a freshly excised bovine liver. Macroscopically quantified coagulation volumes, lesion shape characteristics, and procedure durations were recorded. Results of the prototype featuring the optimal configuration were compared to the original LeVeen probe and commonly used bipolar RF probe (CelonLabPower).
Results
Extension of the shaft electrode length, increasing distance between the shaft electrode and the tip electrode, and reduction of generator output resulted in increasing coagulation volumes. The coagulation volumes the prototype generated were significantly smaller and more elliptically shaped than the monopolar probe (9.4 ± 1.5 cm3 vs. 12.1 ± 1.6 cm3), but were larger than the commercially available bipolar RF probe (vs. 7.3 ± 0.5). The procedure duration of the prototype was comparable to the monopolar probe (467 ± 31 s vs. 464 ± 17 s) and shorter than the bipolar probe (vs. 2009 ± 444 s). In comparison to the commercially available bipolar system, the developed prototype exhibited favorable results.
Conclusion
The first benchmark testing of the developed bipolar prototype had promising results. However, further optimization of the applicator design and ablation protocol is needed to enlarge the achievable coagulation volume.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiofrequency (RF) ablation has been one of the most often utilized techniques among minimally invasive therapies because of its well-established evidence, ease of use, and the option of repeated treatment [1–3]. The basic principle is as following: a high-frequency alternating current is applied to the target tissue by the uninsulated part of the electrode; then the current leads to ionic agitation that is converted into thermal energy by frictional energy loss and finally results in tissue ablation [4, 5].
In clinically used RF systems, two different principles are implemented to close the electric circuit between the RF electrode placed in the target and the second required electrode; in monopolar RF systems, large grounding pads, which are usually fixed at the patient’s thigh, represent the neutral electrode. Therefore, parts of the applied electromagnetic energy pass through the body without contributing to the local ablation effect but lead to an increase in body temperature or heating of metallic implants such as surgical clips. Furthermore, skin burns at the site of the neutral electrodes are a typical complication. In contrast, in bipolar systems, both electrodes, which are separated by a small insulation, are integrated into the tip of the RF probe, obviating the need for a neutral electrode. In this case, the applied current only flows in the vicinity of the RF probe; the need for the grounding pad is thus eliminated.
Monopolar probes have been utilized as standard devices by making various technical advances, such as expandable electrodes and internal cooling to achieve larger coagulation volume. On the other hand, only needle-shaped RF probes, with which the achievable coagulation volume by solo use is limited, had been commercially available for the bipolar system until recently. To extend the coagulation volume, multiple probes were used in this system. However, this approach requires precisely positioned probes, which may sometimes be technically challenging. To combat this drawback, similar to the monopolar probes, an expandable bipolar RF probe had been developed (Concerto, Boston Scientific Corporation, Natick, MA, USA), which was removed from the market as a result of technical problems. A few researchers have reported on the other expandable bipolar RF probes, but their techniques still have not been well established.
The aim of the presented work was to test a simple technical solution for extending the coagulation volume by comparing the performance of an expandable bipolar probe, which was developed on the basis of a commonly used umbrella-shaped RF probe (LeVeen, Boston Scientific Corporation), with the commercially available probes (i.e., the standard LeVeen electrode and the most commonly used needle-shaped bipolar RF probe, CelonLabPower [Celon AG Medical Instruments, Teltow, Germany]).
Material and Methods
Prototype Development
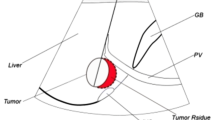
The prototypes tested in this study were developed on the basis of a commercially available LeVeenSuperSlim RF probe for soft tissue ablation featuring a 3-cm array with 10 prongs and a shaft diameter of 17 gauge. In order to integrate a second electrode into the probe shaft, a steel tube with an outer diameter of 2.1 mm and a wall thickness of 0.1 mm was pushed over the probe shaft in such a way that no direct contact between the uninsulated tip of the RF probe (tip electrode) and the tube (shaft electrode) was possible. Furthermore, the metallic tube was covered with a polytetrafluoroethene (PTFE) coat for insulation from the surrounding tissue (Fig. 1). The distal end of the metallic tube remained uninsulated and was connected to the used RF generator via a clamp working as a shaft electrode. Prototypes with different configurations were built and tested.
Schematic drawing of the developed prototype. (a) Insulation between electrode array at the tip and second electrode located on the shaft of the RF probe (0.5–1.5 cm). (b) Metal tube representing the second electrode on the shaft of the RF probe (0.5–1.5 cm). (c) Insulation (PTFE) between second electrode and surrounding tissue
To investigate the influence of the distance between shaft, electrode, and tip, the electrode length of the insulation was systematically varied between 0.5 and 1.5 cm, whereas the length of the shaft electrode was kept constant (Table 1).
As a next step, the length of the second electrode was also varied (0.5–1.5 cm) (Table 2). As a third step, the recommended ablation protocol for the original LeVeen electrode (Fig. 2) was modified on the basis of the experience that less generator output is needed when bipolar RF probes are used for soft tissue ablation (Table 3).
Finally, on the basis of the obtained results, a prototype with a 3-cm-long electrode shaft and a 0.5-cm distance between the shaft and tip of the electrode was constructed.
Every RF probe was used for ten ablation procedures as described below.
Experimental Setting
For the evaluation of achievable coagulation volume and lesion shape, RF ablations were performed on bovine liver using a clinical RF ablation generator (RF 3000, Boston Scientific Corporation). The system delivers variable power output between 2 and 200 W at a frequency of 461 ± 5 kHz. During the ablation procedure, the generator output and tissue impedance, as well as application time, were continuously displayed. Freshly excised bovine liver was obtained from the local animal laboratory. Before the RF ablations, the whole organ was placed in a metallic basin that was filled with a 0.9 % saline solution to simulate the surrounding soft tissue. Then the RF electrode was placed into the liver with an insertion depth of at least 3.5 cm in order to prevent the lesions from reaching the liver surface. As recommended by the vendor for the original LeVeen electrode, the generator output was initially set to 40 W. Then the wattage was increased by 10 W every 30 s until 80 W was reached. The first ablation cycle was finished when a rapid rise in tissue impedance due to desiccation stopped the energy deposition—the so-called roll-off. After a 30 s interval, a second ablation cycle was accomplished starting with 40 W again for 5 min as recommended. Then, the generator output was increased to 60 s by 10 W until the second roll-off occurred.
To evaluate the influence of the generator output, another protocol was used for the second ablation cycle starting with a power output of 20 W that was increased every 30 s by 5 W until 40 W was reached. For the bipolar RF ablations, a commercially available CelonProSurge T30 probe with a 30-mm active tip length and a diameter of 1.8 mm was used. The active tip consisted of both the active and return electrodes, which were separated by a small insulator. In addition, the probe featured an internal cooling system using a circulating saline solution. According to the vendor’s recommendations, the output of the RF generator (CelonLabPower, Celon AG Medical Instruments) was set to 20 W for the electrode with the 30-mm active tip length and the Resistance Controlled Automatic Power mode was used, which means that power output was automatically adjusted to the measured tissue resistance to avoid early tissue dehydration and a resulting rise in impedance. RF ablations were automatically interrupted when tissue resistance measured by the RF system exceeded 900 Ω.
Lesion Size Measurement
After the completion of RF procedures, the RF probe was removed and the puncture tract was marked with a piece of stiff wire. Next tissue samples were dissected along the axis of the electrode track using the wire piece as guidance. In ex vivo specimens, the tan to charcoal-gray area of the RF-induced lesion corresponds to the zone of coagulation necrosis by macroscopic examination [6]. The diameter of the induced coagulation necrosis was measured along the electrode insertion axis (x-axis) as well as the diameter in the two perpendicular planes (y- and z-axes). Then the volume was calculated by approximating its shape into a sphere, in accordance with the formula published by Lee et al. [7]:
For characterization of the lesion shape, the ratio between the vertical (x-axis) and the mean of the two horizontal diameters was calculated:
A shape index around one indicated a spherical lesion, whereas an index larger than one characterizes a more elliptically shaped lesion.
Lesions that had been induced in the vicinity of large vessels, as evaluated after dissection, were excluded from the analysis because large vessels near ablation areas influence the achieved coagulation volume [8]. Every constructed RF electrode, as well as the commercially available probes, was used for 10 ablation procedures, which were included in the statistical analysis.
Statistical Analysis
Data were displayed as arithmetic means ± standard deviation. After performance of an F test to compare the variances, the results obtained using the developed prototype were compared with the original LeVeen probe and the CelonLabPower bipolar RF probe by a t test for independent samples (equal variances) or a Welch test (unequal variances). A p value of < 0.05 was considered statistically significant. Because of the explorative character of the study, no Bonferroni adjustment was performed. Data analysis was conducted by Medcalc software, version 9.1.0.1 (Medcalc Software, Mariakerke, Belgium).
Results
A total of 90 ablation procedures were performed using the different electrodes. The generated zones of coagulation necrosis were characterized by a pale brown area surrounding the centrally located puncture tract of the RF probe (Fig. 3). No lesion reached the surface of the liver samples. Results and electrode characteristics are summarized in Tables 1, 2, 3 and 4.
The extension of the distance between active tip electrode and shaft electrode resulted in an increase of achieved mean coagulation volume (Table 1), whereas mean shape indices were similar for the different electrodes indicating an ellipsoidal shape. The increase of the shaft electrode length led to an increase of coagulation volume as well (Table 2). The reduction of the initially set generator output from 40 to 20 W was associated with a slight increase of the procedure duration but also resulted in larger coagulation volumes (Table 3). Regarding the shape indices, only minor changes were observed.
In comparison with the original LeVeen probe, the coagulation volumes generated by the prototype under adjusted conditions based on the obtained results were significantly smaller (9.4 ± 1.5 cm³ vs. 12.1 ± 1.6 cm³, p = 0.0008). The mean shape indices signified a more elliptical shape for the lesion induced with the prototype (2.3 ± 0.3 vs. 1.2 ± 0.1; p = 0.0001). No significant differences were found regarding procedure duration.
Considering generator output and achieved coagulation volume, the prototype was more effective in comparison to the original monopolar RF probe. Although the original monopolar probe generated approximately 30 % larger coagulation volumes, the generator output was twice as high as for the prototype (40 vs. 20 W) at comparable procedure durations (464 ± 17 vs. 467 ± 31 s).
In comparison to the commercially available bipolar needle-shaped RF probe, the developed prototype generated a larger mean coagulation volume (7.3 ± 0.5 vs. 9.4 ± 1.5) with considerably shorter procedure duration (468 ± 31 vs. 2009 ± 444) (Table 5).
Discussion
During the last decade, RF ablation has become an established minimally invasive treatment modality, particularly for the therapy of liver tumors in patients whose disease is not suitable for curative resection and in patients who are not eligible for orthotropic liver transplantation. During monopolar RF procedures, which have been commonly performed, the current running between the active electrode that is placed into the target lesion and the neutral electrodes, which are usually fixed at the patient’s thigh, can result in an elevation of body temperature dependent on the amount of applied energy [8]. Especially in patients with severe comorbidities, this elevation of body temperature is a relevant burden for the cardiovascular system. In addition, metallic implants, such as surgical clips or prostheses, may be heated by the current passing through the body. Also, skin burns at the site of the neutral electrode may occur as a result of a mismatch between the applied energy and the size of the grounding pads, especially if high-energy ablation protocols are used [9, 10]. In bipolar RF ablation, the second electrode is integrated into the shaft of the RF probe, obviating the need for grounding pads and thereby reducing the risk of the aforementioned complications. However, the bipolar RF system has drawbacks; it requires either the simultaneous placement of multiple probes or the repositioning of multiple probes in order to achieve the sufficient coagulation volume. These two solutions can be technically challenging and/or associated with an increased risk of complication resulting from multiple passages [11]. Thus, a bipolar RF probe with which larger volume coverage can be obtained is required. The concept of bipolar RF ablation was introduced by McGahan et al. [12], who used two monopolar electrodes in a bipolar mode. The first clinical reports about the commercially available bipolar RF ablation system were published by Tacke et al. [13], who treated liver, kidney, and bone tumors with bipolar or multipolar RF ablation using needle-shaped RF probes. Since then, simultaneous placement has been commonly performed in order to achieve complete tumor destruction in clinical settings. Some trials have been conducted for expanding the coagulation volume safely and simply, but a standardized solution has not been rigidly established [14–21].
Compared to the original LeVeen electrode, the developed prototype generated significantly smaller coagulation volumes with a more ellipsoidal shape. The ellipsoidal ablation zone in particular would be the major drawback of the current prototype because including the target into the eccentric shape is obviously difficult. An explanation for this shape with a smaller volume is given by the development of the ablation zone around bipolar RF probes [22]. At first, the tissue between the two electrodes is coagulated as a result of the high current density in this area. Then the coagulation zone grows into the peripheral area. At the same time, a zone of dehydration occurs closely around the electrodes, which leads to an increase in tissue resistance. Once both electrodes are surrounded completely by this area of dehydration, no more electromagnetic energy can be applied and the ablation process stops. Thus, in the case of the presented prototype, coagulation starts along the probe shaft because the RF probe has a small uninsulated section at the very end of the shaft. Then the coagulated lesion grows along the shaft and along the prongs of the electrode array. If the zone of dehydration around the second electrode on the shaft develops quickly, the zone of coagulation may not reach the outer parts of the prongs, resulting in an ellipsis-shaped coagulation volume (Fig. 3). As a consequence, a stable and predictable treatment would be difficult to achieve in the clinical setting.
An initial, and probably the simplest, solution to overcome this limitation could be to reduce the applied energy, which we tested. The result was in accordance with the ex vivo study by Clasen et al. [23] demonstrating an inverse relationship between generated coagulation volume and power output using an internally cooled needle-shaped bipolar RF probe. However, with the increasing volume of coagulation, the required duration of energy application was also increased. Additionally, further technical developments and optimizations are conceivable. First, instead of the integration of the second electrode into the probe shaft, the construction of a second expandable array may offer the advantage of a more homogeneous distribution of the induced electromagnetic and thermal fields. Second, lengthened or wider spreading original expandable electrode, which is assumed to expand the volume of current distribution, may improve the shape and volume. Third, in comparison with the needle-shaped bipolar CelonLabPower RF probe, which has internal cooling circulation, the presented prototype created a larger coagulation volume. Thus, as it has been demonstrated that internally cooled RF probes provide more homogeneous energy deposition, the integration of an internal cooling system or of an injection channel into the probe shaft is another option for further improvement [24, 25]. Because those future modifications require more sophisticated technical constructions, we decided not to test these ideas with the preliminary prototype, but our studies are ongoing. We also plan to study the benefit of using multiple expandable bipolar RF probes.
The presented study has two limitations that should be discussed: primarily, all ablations were performed in an ex vivo liver model without the cooling effect of the physiological perfusion. It is known that the cooling effect of the blood flow, which is known as the heat-sink effect, results in smaller coagulation volumes in vivo [26]. The relatively homogeneous impedance of the normal liver parenchyma in comparison to tumors was also not taken into account. However, the aim of our study was the development and first benchmark testing of an expandable bipolar RF device. For this purpose, ex vivo studies in freshly excised bovine livers provide an established basis for the evaluation of different RF ablation techniques [17, 23, 25, 27]. Additionally, the approximation in volume calculations needs to be taken into account. The formula adopted is based on the assumption that all ablation zones are similarly spherical or elliptical, although ablation zones achieved by the expandable bipolar RF probe were found to be significantly more eccentric than the other two. That might have some impact on the result; however, we believe that that approximation was reasonable for pathological volume measurements in this study in view of enough simplicity in the calculation method for reproducibility.
In summary, the presented data demonstrate the successful development of a new expandable bipolar RF ablation prototype that is based on a commercially available umbrella-shaped RF probe. The first benchmark testing in the ex vivo liver model had promising results. However, further work on probe design, features, and ablation protocol is needed for the optimization of the presented probe concept.
References
Ahmed M, Brace C, Lee F et al (2011) Principles of and advances in percutaneous ablation. Radiology 258:351–369
de Baere T (2011) Lung tumor radiofrequency ablation: where do we stand? Cardiovasc Interv Radiol 34:241–251
Venkatesan A, Wood B, Gervais D (2011) Percutaneous ablation in the kidney. Radiology 261:375–391
Pereira PL, Trübenbach J, Schmidt D (2003) Radiofrequency ablation: basic principles, techniques and challenges. Fortschr Röntgenstr 175:20–27
Goldberg SN, Dupuy DE (2001) Image-guided radiofrequency tumor ablation: challenges and opportunities—part I. J Vasc Interv Radiol 12:1021–1032
Morimoto M, Sugimori K, Shirato K et al (2002) Treatment of hepatocellular carcinoma with radiofrequency ablation: radiologic–histologic correlation during follow-up periods. Hepatology 35:1467–1475
Lee JM, Han JK, Kim SH et al (2005) Bipolar radiofrequency ablation using wet-cooled electrodes: an in vitro experimental study in bovine liver. AJR Am J Roentgenol 184:391–397
Sawada M, Watanabe S, Tsuda H, Kano T (2002) An increase in body temperature during radiofrequency ablation of liver tumors. Anesth Analg 94:1416–1420
Livraghi T, Solbiati L, Meloni MF et al (2003) Treatment of focal liver tumors with percutaneous radio-frequency ablation: complications encountered in a multicenter study. Radiology 226:441–451
Razafindratsira T, Isambert M, Evrard S (2011) Complication of intraoperative radiofrequency ablation of liver metastases. HPB (Oxford) 13:15–23
Bruners P, Schmitz-Rode T, Günther RW, Mahnken A (2008) Multipolar hepatic radiofrequency ablation using up to six applicators: preliminary results. Rofo 180:216–222
McGahan JP, Gu WZ, Brock JM et al (1996) Hepatic ablation using bipolar radiofrequency electrocautery. Acad Radiol 3:418–422
Tacke J, Mahnken A, Roggan A, Günther RW (2004) Multipolar radiofrequency ablation: first clinical results. Rofo 176:324–329
Lee JM, Han JK, Kim SH et al (2003) A comparative experimental study of the in-vitro efficiency of hypertonic saline-enhanced hepatic bipolar and monopolar radiofrequency ablation. Korean J Radiol 4:163–169
Haemmerich D, Staelin ST, Tungjitkusolmun S et al (2001) Hepatic bipolar radio-frequency ablation between separated multiprong electrodes. IEEE Trans Biomed Eng 48:1145–1152
Mack MG, Straub R, Desinger K (2000) MR-guided interstitial bipolar RF thermometry: in-vivo evaluations and first clinical results. Radiology 217:359
Stoffner R, Kremser C, Schullian P et al (2012) Multipolar radiofrequency ablation using 4–6 applicators simultaneously: a study in the ex vivo bovine liver. Eur J Radiol 8:2568–2575
Neuhaus J, Blachut L, Rabenalt R et al (2011) Efficiency analysis of bipolar and multipolar radiofrequency ablation in an in vivo porcine kidney model using three-dimensional reconstruction of histologic section series. J Endourol 25:859–867
Clasen S, Rempp H, Schmidt D et al (2012) Multipolar radiofrequency ablation using internally cooled electrodes in ex vivo bovine liver: correlation between volume of coagulation and amount of applied energy. Eur J Radiol 81:111–113
Eisele RM, Neuhaus P, Schumacher G (2008) Radiofrequency ablation of liver tumors using a bipolar device. J Laparoendosc Adv Surg Tech A 18:857–863
Meijerink MR, van den Tol P, van Tilborg AA et al (2011) Radiofrequency ablation of large size liver tumors using novel plan-parallel expandable bipolar electrodes: initial clinical experience. Eur J Radiol 77:167–171
Frericks BB, Ritz JP, Roggan A et al (2005) Multipolar radiofrequency ablation of hepatic tumors: initial experience. Radiology 237:1056–1062
Clasen S, Schmidt D, Boss A et al (2006) Multipolar radiofrequency ablation with internally cooled electrodes: experimental study in ex vivo bovine liver with mathematic modelling. Radiology 238:881–890
Brieger J, Pereira PL, Trubenbach J et al (2003) In vivo efficiency of four commercial monopolar radiofrequency ablation systems: a comparative experimental study in pig liver. Invest Radiol 38:609–616
Bruners P, Pfeffer J, Kazim RM et al (2007) A newly developed perfused umbrella electrode for radiofrequency ablation: an ex vivo evaluation study in bovine liver. Cardiovasc Intervent Radiol 30:992–998
Goldberg SN, Hahn PF, Tanabe KK et al (1998) Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis? J Vasc Interv Radiol 9:101–111
Lee JM, Kim SH, Han JK et al (2005) Ex vivo experiment of saline-enhanced hepatic bipolar radiofrequency ablation with a perfused needle electrode: comparison with conventional monopolar and simultaneous monopolar modes. Cardiovasc Interv Radiol 28:338–345
Acknowledgments
The authors thank L. Schönherr for text editing.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ito, N., Pfeffer, J., Isfort, P. et al. Bipolar Radiofrequency Ablation: Development of a New Expandable Device. Cardiovasc Intervent Radiol 37, 770–776 (2014). https://doi.org/10.1007/s00270-013-0703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-013-0703-2