Abstract
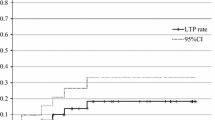
Today, radiofrequency ablation (RFA) of primary and metastatic lung tumor is increasingly used. Because RFA is most often used with curative intent, preablation workup must be a preoperative workup. General anesthesia provides higher feasibility than conscious sedation. The electrode positioning must be performed under computed tomography for sake of accuracy. The delivery of RFA must be adapted to tumor location, with different impedances used when treating tumors with or without pleural contact. The estimated rate of incomplete local treatment at 18 months was 7% (95% confidence interval, 3–14) per tumor, with incomplete treatment depicted at 4 months (n = 1), 6 months (n = 2), 9 months (n = 2), and 12 months (n = 2). Overall survival and lung disease-free survival at 18 months were, respectively, 71 and 34%. Size is a key point for tumor selection because large size is predictive of incomplete local treatment and poor survival. The ratio of ablation volume relative to tumor volume is predictive of complete ablation. Follow-up computed tomography that relies on the size of the ablation zone demonstrates the presence of incomplete ablation. Positron emission tomography might be an interesting option. Chest tube placement for pneumothorax is reported in 8 to 12%. Alveolar hemorrhage and postprocedure hemoptysis occurred in approximately 10% of procedures and rarely required specific treatment. Death was mostly related to single-lung patients and hilar tumors. No modification of forced expiratory volume in the first second between pre- and post-RFA at 2 months was found. RFA in the lung provides a high local efficacy rate. The use of RFA as a palliative tool in combination with chemotherapy remains to be explored.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The initial target of radiofrequency ablation (RFA) as an thermal ablation technique was unresectable primary and metastatic liver tumors, where impressive results have been achieved. This has encouraged interventional radiologists to use the same technique to treat cancers at other sites. Because RFA was initially applied to treat liver tumors, the algorithm for RFA current delivery had to be tailored to the lung to obtain a predictable and reproducible volume of destruction. Indeed, the characteristics (e.g., vascularity and electric conductivity) of tissue that surrounds the tumor affects heat and electricity diffusion, and consequently ablation outcomes. For example, a given quantity of radiofrequency (RF) current delivered to a tumor produces a larger volume of ablation in the lung than in subcutaneous tissues or in kidney [1]. This highlights the site-specific differences in favor of lung, probably as a result of heat insulation and low electric conductivity provided by lung around the tumor.
Several experimental works have demonstrated that RF can completely destroy an area of healthy lung or malignant lung tumors in an animal tumor model [2, 3]. Consequently, RFA of primary and metastatic lung tumors is increasingly used, with impressive results in terms of local efficacy. Percutaneous thermal ablation, including RFA, is only a small integrative part in the more vast and complex area of oncology. Treatment strategies combining other therapeutic weapons such as surgery, radiotherapy, and chemotherapy need to be defined and evaluated. Today, RFA is mostly used as a stand-alone technique, with the main objective being complete destruction of tumor cells in the targeted volume. The low morbidity, including breathing impairment pain, and shorter hospital stay make the procedure possible in patients who have comorbidities that result in their not being surgical candidates. In the future, it will be necessary to define the impact of pre- or post-RFA chemotherapy used adjuvantly or neoadjuvantly. The same question applies to target therapies, which for most patients are responsible for the decrease in vascularization of tumor tissue, and it might be helpful to increase the efficacy of RFA, as has been demonstrated in an animal model [4].
Technique
Principle
RFA induces a thermal destruction of tissues and does not have any specificity for tumor cell. Even if tumor has been reported as more sensitive to hyperthermia than normal tissue, this does not apply—or at least it has never been demonstrated in the thermal range used for RFA. The goal of RFA is to destroy tumors by heating cells to >60°C to obtain nonreversible cellular modification. The RF is a sinusoidal current with a frequency of 400 to 500 kHz that heats tissues through ionic agitation. Three factors are involved in tissue heating. Resistive heating is proportional to the density of RFA energy in the tissue and diminishes to the fourth power of the distance to the needle, to such an extent that only the tissue very close to the electrode is affected by this resistive heating. Conduction differs according to tissue type and is the means by which heat obtained via resistive heating spreads to neighboring tissues. Convection causes decay in tissue heating by transporting heat via fluid traversing heated tissue. In the liver, convection is mostly due to calorific dispersion due to vascularization. These three factors are responsible for a thermal equilibrium that depends on the distance to the electrode, the RFA energy delivered, the duration of treatment, and the type of tissue and its vascularization.
To increase the RFA volume by a single delivery, the single-needle electrode has been transformed into more complex tools: expandable multiprong, cooled, and bipolar electrode/needles. The so-called expandable needle is a needle containing several (usually 8–12) electrodes that are deployed in the targeted tissue once punctured. These electrodes produce as many small areas of destruction as the number of electrodes, and a larger area of destruction is achieved by summing the small ones as a result of the adequate design (spatial geometry) of the expandable prongs/electrodes. The cooled needle is a double-lumen needle housing the electrode that is cooled with chilled water. This cooled needle can be used as a single device or clustered. More current can be delivered with this technique than with a bare electrode, without boiling or desiccation of tissue close to the electrode. Although current density is very high in the tissues close to the needle, these tissues are cooled via forced convection as a result of the chilled water running in the double lumen of the needle. In other words, the excess RF energy deposition close to the needle, invariably producing excess heat, is reabsorbed to avoid boiling close to the needle.
Bipolar RF is made of two electrodes situated a few millimeters apart on a single needle. The principle is to create a high-density field of RF energy between the two electrodes inserted in the targeted tissue. In this setting, grounding pads are no longer necessary, and up to three needles (six electrodes) can be activated by a single generator providing multipolar RF by activation of all dipole combinations, one after the other. Specific algorithms, usually requiring lower power, are needed to deliver treatment to the lung [5]. A perfused needle has been developed that takes advantage of enhanced RF delivery with the help of saline perfusion, which increases electric conductivity and boiling temperature. If this technique has been demonstrated to increase the volume of ablation, it has also been demonstrated to be poorly predictable, with irregular margins in healthy lung [6]. Consequently, the use of this needle is rarely reported in clinical practice.
The expandable needle is the most commonly used design in reports of lung RFA, probably because it is less prone to migration when deployed in very soft lung parenchyma, even if this advantage has never been demonstrated in preclinical or clinical studies. The use of guiding needle or flexible needle allows easier access inside the computed tomography (CT) gantry and decreases the risk of breaking sterility by contact between the handle of the RF needle and the gantry. In addition, the guiding needle allows biopsy to be performed at the same time as RFA through a single path when needed, as described in liver ablation [7]. The RF delivery must be adapted to tumor location because impedance before ablation is significantly different (P = 0.04) for the tumors, with >50% of the tumor abutting the pleura (86.5 ± 29.9 Ω), as well as the tumors that were not abutting the pleura (121.3 ± 42.8 Ω) or the tumors with <50% of the tumor abutting the pleura (112.6 ± 32.9 Ω). Indeed, tumor surrounded by lung parenchyma is highly electrically and thermally insulated by the air-filled lung parenchyma compared to a tumor abutting on the pleura and will require less energy deposition.
Treatment Planning
Pre-RFA imaging is the same as preoperative imaging, because most indications for RFA are curative, and thus distant disease must not be ignored. Abdominal CT or positron emission tomography (PET)–CT are useful to search for distant metastases, and PET can be used for follow-up of treated tumors. A chest CT is needed to determine target tumor location and size, which will determine possibility of treatment, patient positioning, and access route. Lung spirometry is useful in patients with a history of diffuse lung disease or lung surgery, but it is not systematically performed in clinical studies, namely in patients without medical or surgical history in the lung.
Lungs are usually treated one at a time to avoid the possibility of life-threatening complications from bilateral adverse events, such as bilateral massive hemorrhage or pneumothorax. Whatever the number of targeted tumors, when they are unilateral, they are usually targeted in a single session. An interval of a few weeks is usual between two treatment sessions scheduled for bilateral disease. When patients have had previous lung surgery, the risk of pneumothorax is low, and bilateral treatment has been reported. Such bilateral treatment in a single session concerns a small percentage of reported cases and is reserved for patients who underwent uneventful treatment completion in the first lung without any CT-depicted complications.
No difference in tumor control was reported by Hoffmann et al. [8] when comparing procedures performed with the patient either under general anesthesia or under conscious sedation in a series of 26 treatment sessions; a review of the literature in liver tumor RFA reports the use of general anesthesia as a predictive factor of complete ablation [9]. In the series of Hoffmann et al., 11 of 11 treatments could be completed under general anesthesia, while 2 of 15 treatments could not be completed under conscious sedation and required a second step under general anesthesia [8]. In other reports, the use of conscious sedation was associated with periprocedural pain in 29% of cases, with 3% of treatment interrupted as a result of pain [10] or stopped altogether as a result of intractable coughing in 5 of 30 patients [11]. The feasibility of the technique under general anesthesia is reported to be as high as 97% [5]. General anesthesia may be preferable for the novice operator in cases of difficult or multiple lesions, although it might be considered in all patients as a result of increased feasibility and the comfort in targeting tumor that might result in a higher success rate of ablation.
Image Guidance
Electrode positioning must be performed for sake of accuracy. Unlike the liver, kidney, or soft tissue, where the choice of image guidance may be among ultrasound, magnetic resonance imaging (MRI), and CT, CT is today the only accurate image guidance modality for lung RFA. Real-time CT with foot-pedal control results in faster needle placement than other technologies, and the procedure is more comfortable for the operator. Multiplanar reconstruction is mandatory to assess adequate needle positioning, namely to image prongs/electrodes deployment relative to tumor margins in all planes (Fig. 1). Antoch et al. [12], after evaluating needle positioning centered in a liver tumor via axial CT, then assessed a image data set created via multiplanar and volume-rendered analyses and reclassified the needle position from centered to marginal or from marginal to outside in 44% of RF procedures (14 of 32). Marked differences in density between the tumor, the surrounding lung parenchyma, and RF probes make it easy to clearly differentiate between normal lung tissue, tumor, and needle tines and to accurately evaluate adequate targeting of the tumor. The excellent visualization of the RF probe and its expandable tines within the tumor in three dimension allows for excellent accuracy of probe placement and is probably an explanation for the excellent results of RFA in lung.
Multiplanar reconstruction of a chest computed tomographic scan in axial (A), sagittal (B), and coronal (C) planes. A 4-cm expandable radiofrequency (RF) needle within a 2.5-cm lung metastasis is targeted for RF ablation. Note the large size of the RF needle when compared to the tumor to achieve an ablation margin. Needle position is adequate because the tines oversize the tumor in any direction
When a needle with an expandable electrode is used, puncturing the tumor with the electrode shaft is not required for small tumors as long as the deployed arrays are encompassing the tumor, with one of the arrays through the tumor and a volume of ablation containing the tumor. Great care must be taken to avoid traversing the tumor with the electrode shaft or deploying the arrays through the tumor without delivering RF to minimize the risks of potential seeding, even if seeding has not been proven after such maneuver. Pneumothorax obtained on purpose with a Veress needle and reaspirated after treatment can be used to avoid collateral damage during ablation of subpleural tumors to separate subpleural tumor from the parietal pleura or the mediastinum. When tumor is located subpleurally, the accuracy of puncture has been reported to be more accurate by two different teams when a longer/oblique needle path is used vs. a short/right-angle one [13, 14].
Imaging Follow-up
CT images taken immediately after RFA show the lung tumor surrounded by ground-glass opacity, which enlarges the diameter of the hyperattenuating tumor [5, 15] (Fig. 2). In normal lung, a central, dense opacity is surrounded by an extensive area of ground-glass opacity. Pathologically, the central, dense opacity corresponds to destructive tissue, while the ground-glass opacity corresponds to tissue with some degree of injuries, which represents a zone of ongoing necrosis [16]. In clinical practice, a well-demarcated zone of ablation is seen as early as 24 and 48 h after treatment, after which the ablation area will not increase in size [5]. In most cases, this zone will start to shrink slightly as early as 2 to 3 weeks after ablation, representing a tissue-repairing process in which the granulation tissue progressively replace the inner necrotic tissue [16]. Cavitation of the ablation zone has been reported to occur in up to 31% of ablations, more commonly when ablation was in contact with a segmental bronchus [17]. Most reports of lung RFA use CT as the follow-up imaging modality to assess the ablation volume, which mostly looks at morphologic changes to evaluate treatment efficacy. Enhancement of the residual tumor after RFA is commonly used for follow-up of liver tumors, but it seems less informative in lung tumors treated with RFA [18]. Recently, diffusion MRI has demonstrated interesting preliminary results, which remain to be confirmed in larger series [19]. It is generally considered that an ablation volume that does not increase in size on subsequent imaging is a complete ablation.
Computed tomographic (CT) scan showing right upper centimetric metastases from colorectal cancer (A). Immediately after radiofrequency ablation, a thin peripheral rim is seen (B). Two days after ablation, a new CT is performed for an obvious subcutaneous emphysema (C). One can notice ground-glass opacity encompassing the tumor with adequate ablation margins. The subcutaneous emphysema resolved spontaneously 5 weeks later
This method of evaluation has some drawbacks, namely late discovery of incomplete treatment. Indeed, for de Baere et al. [5], among six incomplete treatments, one was depicted at 4 months, two were depicted at 6 months, one was depicted at 9 months, and one was depicted at 12 months; the mean ± standard deviation duration before depicting incomplete treatment was 7.66 ± 2.77 months in a report with a minimum of 1-year follow-up (mean, 18 months). The follow-up of 79 non-small-cell carcinoma in 79 patients with CT revealed 10.1% incomplete local treatment at 1 year and 28% at 2 years, which highlights the delay in the discovery of incomplete ablation [20].
To avoid late discovery of incomplete ablation, PET-CT seems promising to provide early evaluation of treatment response. Sensitivity and specificity of PET have been reported to be better than CT in early detection of incomplete ablation. Okuma et al. demonstrated in a preclinical study that timing of PET after ablation is a key factor because fluorine-18 fluorodeoxyglucose (F18-FDG) uptake is highly increased 1 to 3 weeks after ablation, with an standard uptake value (SUV) ratio of ≥5 between RF ablation zone to muscle [19]. Consequently, it is wise to avoid PET imaging between 1 and 4 weeks after ablation so as to not misinterpret a post-RFA inflammatory reaction for active tumor.
In our unpublished experience, which we presented at the Radiological Society of North America 2009 meeting, 28 patients with 46 lung tumors treated with RFA received fludeoxyglucose (FDG)-PET–CT at 1 day, 1 month, and 3 months after ablation. Complete treatment was diagnosed in 41 tumors and incomplete treatment in 5 tumors (3 at 1 month and 2 at 3 months) by FDG-PET-CT follow-up. It was truly positive in 4 cases, falsely positive in 1 case, and truly negative in 41 cases. For the same population, chest CT scan diagnosed complete treatment in 44 lesions and incomplete treatment in 2 tumors at 3 months, with true-positive findings in 1 case, false-positive findings in 1 case, false-negative findings in 3 cases, and true-negative findings in 41 cases. FDG uptake in inflammatory mediastinal lymph nodes was observed in 15, 21, and 15% of the patients at 24 h, 1 month, and 3 months, respectively. FDG uptake at RFA puncture was observed in 19, 11, and 15% of the patients at 24 h, 1 month, and 3 months, respectively.
Indications
Today, RFA is used for treatment of primary and metastatic lung neoplasms with indications close to those of surgical resection. RFA is thus performed with curative intent in nonsurgical or borderline surgical candidates. Inoperability is most often due to poor respiratory function in relation to chronic obstructive pulmonary disease (COBP) in primary tumors, and iterative surgery in metastatic patients. Because the intent is curative, a preablation imaging workup must be equivalent to a presurgical one—namely evaluating potential distant disease with imaging of the most common sites of metastatic disease according to the location of the primary tumor with CT, MRI, or PET-CT. In addition, the size and number of the tumors matter not only for the oncologic indication, but also for the technical possibilities. It is usually thought that the number of tumors deposited per hemithorax should not be >5, and that the largest diameter should be <5 cm, and ideally <3.5 cm.
The use of lung RFA as a palliative treatment needs to be explored in a manner close to that reported in the liver colorectal cancer metastases by Ruers et al. [21], who evaluate the benefit of RFA plus chemotherapy vs. chemotherapy alone and demonstrated a benefit in progression-free survival from 10 to 16.8 months.
Results
Local Efficacy
A review of 17 of the most recent publication demonstrated a median reported rate of complete ablation of 90%, even if high variability exists between publications, which report ranges from 38 to 97% [22]. It seems from a very small-sized ablation and resection study that tumor <2 cm in size is completely ablated, while overall ablation rate was only 37.5% [23]. It is noteworthy that in this study, RFA was performed per-operatively, and no image guidance was used. Tumors <2 cm in size can be ablated in 78 to 96% of cases, according to several reports of CT-guided RFA performed with a lengthy imaging follow-up of treated patients [5, 15, 24–26].
Most studies report a statistically significant lower success rate of ablation with tumors >2 to 3 cm in diameter [5, 15, 24, 25]. Lee et al. [11], in a early report of lung RFA, observed success rates declining to 38% for tumors between 30 and 50 mm and to 8% for tumors of >50 mm. The rate of complete ablation is highly dependent on the volume of ablation relative to the tumor volume, which affects ablation margins. For de Baere et al. [5], when the ratio between the area of post-RFA ground-glass opacity and the tumor area before treatment was at least 4, the rate of complete ablation was 96% at 18 months, and significantly higher (P = 0.02) than the 81% obtained when this ratio was below 4. In the same manner, a 83% complete ablation rate at 1 year has been reported when the ratio of ablation volume to tumor volume was ≥3, while the success rate was 61% when this ratio was <3 [24].
Ground-glass opacity margins have been reported absent in 85% of post-RFA CT of incompletely ablated tumors [27]. In the same study’s receiver operating characteristic curve analysis constructed from recurrence, according to ground-glass opacity, minimal width after ablation confirmed the usefulness of the ablation zone as a predictor of recurrence, with an estimated cutoff of 4.5 mm for a specificity of 100%—that is, no local recurrence. The above-mentioned results from three different centers clearly emphasize that there is a need for oversizing the ablation zone relative to the tumor volume to obtain safety margins that guarantee success. This need for oversizing is also demonstrated by the pathologic findings of resected specimens, where clusters of aerogenous spread with floating cancer cells are found in 41% of lung metastases from colorectal cancer at a distance of 0.5 to 11 mm (median, 2 mm) of the external boarder of the main nodule in metastases [28]. Consequently, because RFA tools provides a volume of ablation with a shortest diameter of approximately 4 to 5 cm, selection of tumor <3 cm in size will provide better complete ablation rate considering that an ablation margin of 1 cm is sought.
One of the drawbacks of RFA is that only one probe can be activated at one time, even when using the switching monopolar RF technique [29] or multipolar RFA [30]. Consequently, overlapping the ablation zone to create a larger volume of ablation requires subsequent probe placement and RF deliveries, which is time-consuming and can be technically difficult to perform, whereas lung parenchyma is already modified by previous probe puncture and RF ablation. More recent ablative technologies (e.g., microwaves, cryoablation, irreversible electroporation) have the advantage of simultaneous delivery of the energy through several probes activated at the same time. A single microwave (MWA) antenna has been demonstrated to provide a mean diameter of ablation 25% larger than a single cooled electrode [31]. This study did not compare MWA with the best available RF option in the lung, so its results are questionable. However, simultaneous delivery induced a synergy between the probes that provided a larger volume of ablation than the same probes activated one after the other.
Wright et al. [32] demonstrated that for a given MWA applicator with a fixed energy deposit, activation of one antenna provided 7.4 ± 3.9 cm3 of ablation, activation of three antennae, one after the other, provided 14.6 ± 5.2 cm3 of ablation, while simultaneous activation of the three antennae provided a significantly larger volume of ablation, 43.1 ± 4.3 cm3. The possibility of ablating larger volumes gives hope for a better rate of complete ablation for larger tumors, even if data about outcomes of MWA of pulmonary malignancies remain relatively scarce. Early reports are promising, with the largest available clinical study including 50 patients, 30 with a non-small-cell lung cancer (NSCLC) treated with MWA during 66 ablation sessions for tumors ≤5 cm with a mean size of 3.5 cm ± 1.6 [33]. Tumor <2 cm in size was treated with a single antenna (53%); two antennae were used in 5%, three antennae in 27%, four antennae in 9%, and multiprobe loop antenna in 6%. A total of 26% of patients had recurrent disease at the ablation site. This recurrent disease was most commonly found in tumor >3 cm in size (P = 0.01). It is noteworthy that after MWA, on follow-up imaging, cavitary changes were found in 43% of ablation, and 6% resulted in documented infectious complications, including one abscess and one case of pneumonia [33]. Furthermore, the abscess eroded a mural blood vessel and was responsible for fatal hemoptysis. On the other hand, the patient with cavitation found at follow-up imaging had significantly better survival.
Contact with a large vessel (>3 mm) has been reported as a negative predictive factor of complete tumor ablation in lung [15, 34] in the same manner that it has been reported in liver tumors [35, 36]. The so-called heat sink effect, which is convection cooling by the vessel of the ablated zone, is probably responsible for this increase in rate of incomplete ablation. Because vascular occlusion of the hepatic vein or the portal branch in contact with the liver tumor during RF ablation in liver has been described to improve rate of complete ablation [37], we have performed technically and clinically successful percutaneous balloon occlusion of the pulmonary artery branch during lung RFA in a very small group of patients. The procedure was poorly tolerated, with three of five patients readmitted to the hospital within the 15 days after treatment. As reported in a lung animal study, percutaneous balloon occlusion allows an increase in the volume of ablation and renders a more spherical zone of ablation [38]. The use of new energy such as MWA, which has a better thermal profile because it works at higher temperatures and consequently is less subject to convection cooling, could be a valid answer to these difficulties in ablation for tumor close to large vessels. Compared to RFA, which produces heating in the tissue by resistive heating with current at 365–480 kHz, MWA emits electromagnetic radiation at a frequency of 900 MHz to 2.45 GHz, with theoretical advantages of higher temperature, more rapid increase in temperature, no carbonization, and less distortion of the spherical geometry. Such theoretical advantages have been confirmed in liver animal models, where less deflection of the ablation zone in contact with the large vessels has been demonstrated with MWA than with RFA [39]. To our knowledge, this advantage has never been confirmed in clinical practice, either in the liver or the lung, by demonstrating a decrease in the rate of incomplete ablation of tumor close to large vessels fro MWA vs. RFA.
In an animal model, RFA of lung parenchyma close to the heart and even myocardium has been demonstrated to be quite safe, with no damage to the myocardium when ablating close to the heart and with reversible ventricular tachycardia and extrasystoles on discontinuation of RF current [40]. In clinical practice, complete ablation rate at 12 months was significantly different for tumor located 1 to 9 mm from the heart and tumor in contact with the heart with 69.3 and 8.6%, respectively [41]. This difference may be due to the heat sink effect from the heart or to the radiologist’s fear of placing the RF probe in contact with the heart. This difficulty in ablating close to the heart can be overcome by inducing a pneumothorax with a Veress needle (Endopath; Ethicon-endosurgery, Cincinnati, OH) that allows separation of the lung from the heart [42]. Such pneumothorax is obtained by puncture of the parietal pleura without puncture of the visceral pleura, and it consequently never recurred after the manual aspiration performed at the end of the procedure.
Besides size, ablation margins, and tumor location close to a large vessel, the type of needle has been demonstrated to be predictive of complete ablation, with lower success rate for straight, internally cooled electrodes vs. expandable ones (hazard ratio, 2.32; 95% confidence interval [95% CI], 1.10–4.90; P = 0.027) [24]. Straight needles were used for tumor in difficult situations; close to the hilum, only 2-cm active-tip needles were used, which probably had an impedance profile that was not as good as the 3-cm needles.
Local control rates varied among the tumor types, and metastatic colorectal cancer showed significantly (P = 0.023) higher local control rates than those of primary lung cancer, renal-cell carcinoma, or hepatocellular carcinoma on the univariate analysis, but multivariate analysis indicated that the relative risk of local progression for a given tumor type was comparable to the risks for the four other types [43].
Survival
Survival data for RFA are scarce and not mature, with few series providing survival beyond 3 years. This is due to the infancy of the technique, which was first reported in the year 2000 [44]. There is thus no comparative study of RFA and surgery, either for small-size (stage I) NSCLC or lung metastases. Studies comparing RFA and other local ablative therapies or radiotherapy do not exist. Although early reports of survival rates after RFA seem close to rates after surgery, the data are preliminary. Ideally, comparative randomized studies are needed in patients treated with curative intent.
Non-small-cell Lung Cancer
A series of 75 primary NSCLC (75% stage IA and 25% stage IB) patients demonstrated a median survival of 29 months (95% CI, 20–30) with a 1-, 2-, 3-, 4-, and 5-year overall survival of 78, 57, 36, 27, and 27% [45]. Median survival for stage IA was 30 months and 25 months for stage IB. Better survival was reported for tumors ≤3 cm in size, with a survival rate close to 50% at 5 years [45].
Grieco et al. [46] combined radiotherapy and RFA in 41 patients with NSCLC (stage IA, 21; stage IB, 17; stage IIB, 3). The 27 patients with the largest tumors received external-beam radiation (66 Gy), and the 14 patients with tumors <3 cm received brachytherapy through the puncture tract used for RFA. Combination treatment seems to improve results in NSCLC, with 57% survival at 3 years. The median survival was 34.6 ± 7 months for tumors >3 cm and 44.4 ± 5.4 months for tumors ≤3 cm (P = 0.08). Difference between overall survival (70% [95% CI, 51–83] at 1 year and 48% [95% CI, 30–65] at 2 years) and cancer-specific survival (92% [95% CI, 78–98] at 1 year and 73% [95% CI, 54–86] at 2 years) in patients with NSCLC highlight the comorbidities in the NSCLC patients treated with RFA [26].
Metastases
Similar overall survival has been reported by four different teams in colorectal cancer lung metastases with an overall survival of 64 to 78% at 2 years [5, 15, 47, 48]. Extrapulmonary metastasis and tumor size were significantly independent prognostic factors in the multivariate analysis for Yamakado et al. [47], and extrapulmonary metastasis was predictive of survival for Hiraki et al. [43]. For Yan et al. [48], univariate analysis demonstrated the largest size of lung metastasis (P < 0.001) and location of lung metastases (P = 0.032), and repeat percutaneous RFA for pulmonary recurrence (P = 0.024) was statistically significant for overall survival. Multivariate analysis demonstrated that the largest size of lung metastasis of >3 cm was independently associated with a reduced overall survival (P = 0.003).
Tolerance
Many patients will experience mild to moderate postprocedural pain during the 2 to 7 days after ablation. This pain can be managed with oral analgesics. Mild dyspnea is common symptoms and may warrant nasal or mask administration of oxygen. A temperature up to 38°C is common the week after ablation. Most patients are discharged the next day if no drain is present.
Pneumothoraces are found on CT immediately after ablation in approximately 50% of treatment sessions among RF lung publications. However, in approximately 30% of the procedures, they are small enough not to require any treatment. Approximately 20% need to be expelled manually with a small-bore needle catheter inserted while the patient is still lying on the CT table immediately during or after RF ablation. Finally, chest tube drainage is necessary in 4 to 16% of patients. Requirement of chest tube placement after lung biopsy has been described to significantly increase parallel to the increased of volume air manually aspirated with the small bore needle. A cutoff level of 543 ml of aspirated air with a small-bore needle was defined by receiver operating characteristic curve analysis as optimal to abandon manual aspiration alone and resort to chest tube placement [49]. In clinical practice, most teams start with small-bore aspiration as soon as it is possible to safely insert a needle in the pneumothorax under CT guidance, and then convert it to a small-caliber chest tube if pneumothorax recurs during the 15 min after aspiration. The rate of delayed and recurrent pneumothoraces is reported to be 10.3 and 6.7%, respectively, in the only study focusing specifically on this complication [50]. The mean duration before confirmation of the recurrent or delayed pneumothorax was 24 ± 66 h, but only 4 of the 33 the recurrent or delayed pneumothoraces required treatment, which means that overall, <2% of lung RFA had a delayed pneumothorax requiring treatment. The only predictive factor of recurrent or delayed pneumothorax is contact of the ground-glass opacity related to the ablation with the pleura.
Subcutaneous emphysema has been reported in a very few cases. It can be isolated or associated with pneumoperitoneum. More severe subcutaneous emphysema seems linked with lesions that are fixed to the pleura and with occurrence of a bronchosubcutaneous fistula through the ablated tumor [51]. Usually it will self-control: although it may take several weeks to disappear, it will resolve spontaneously. Quite unusual are the cases that will required fibrin sealant [51] or endobrachial one-way valve [52].
Postprocedural minor hemoptysis can occur in approximately 15% of patients. They are usually minor, made of brownish blood, and last from 2 to 7 days without requiring treatment. The reports of severe hemorrhage during ablation concern tumors in contact with the hilum [53, 54]. Delayed major hemorrhage have been reported as a result of false aneurysm of the pulmonary artery [33, 55] successfully treated with coil embolization in one case.
Mean hospital stay was two nights in patients who did not have complications from treatment.
Pulmonary parenchymal complications are mostly pneumonia and pulmonary abscess. Risks of infectious complications are higher in primary disease in compromised lung parenchyma and in previously irradiated lung. Prophylactic antibiotics have not been proven to improve infectious outcome, even if most teams report the use of antibiotics from 1 day to 1 week after treatment.
Tolerance of the technique in terms of respiratory function has been reported to be excellent, with no changes in postablation respiratory test when evaluated prospectively at 1 month by de Baere et al. [5] and at 12 months by Lencioni et al. [26]. Most of the series report uneventful treatment for patients with a forced expiratory volume in the first second superior to 1.2 l. Obviously, some compromised patients will have temporary worsening of respiratory function and will require oxygen therapy from 1 day to 3 weeks. To our knowledge, no patients required long-term or permanent oxygen therapy as a result of RFA. Consequently, it is difficult to place a clear lower threshold of respiratory function for lung RFA. Patients with forced expiratory volume in the first second down to 0.8 l/s have been treated with no post-RFA complications or worsening of respiratory function [5]. A major benefit of lung RFA to treatment of NSCLC is that the excellent tolerance of the treatment allows curative treatment in nonsurgical early NSCLC. Single-lung patients have been targeted with RFA with variable reports in outcome. Simon et al. [45] reported 2.6% (4 of 153) deaths related to RFA, and it is noteworthy that two of four patients who died were single-lung patients. Our group reported at the 2009 Cardiovascular and Interventional Radiological Society of Europe meeting a multicenter experience of 15 single-lung patients, including 11 NSCLC cases treated without major complication. We had 12% minor hemoptysis and 6% pulmonary infection; 37% of patients had a pneumothorax and a chest tube. The median overall hospital stay was 3 days [56].
Asymptomatic microbubble embolism depicted by duplex ultrasound has been reported during lung RFA in humans [57]. Nonfatal major air embolism has been reported as a consequences of RF probe placement in two case reports [58, 59]. Embolism was not linked with RFA delivery but to the electrode insertion itself creating bronchovascular path. Only one case of cerebral infarction after lung RFA can be found [60].
Needle-tract seeding can occur in the same manner that it can occur after any tumor needle puncture. The rate of seeding is evaluated to be 0.2% of RF ablation in an extensive experience of 661 lung RFA procedures [61]. Track ablation, often reported as an antiseeding maneuver in liver ablation, has never been proved to result in decreasing seeding. In the lung, most of the team do not perform track ablation up to the pleura for fear of creating a bronchopleural fistula.
Regarding the excellent tolerance of the treatment, it is difficult to define an absolute contraindication to lung RFA. The major risk during the procedure seems to be tumor close to the hilum due to hemorrhage. Anticoagulation or antiplatelet therapies should be discontinued as much as possible, but we have treated a few patients who received low-dose aspirin, without complications.
Conclusion
RFA is a promising treatment, with high success rates of complete ablation in small primary and metastatic lung tumors that allow curative treatment in patients who are not candidates for surgery or in borderline surgical candidates. Ideal follow-up imaging to determine early treatment failure remains to be improved, probably including functional imaging and CT.
As a potentially curative treatment in nonsurgical candidates, RFA should be compared with sophisticated external-beam radiation, such as tomotherapy and gamma knife, in the treatment of small-size NSCLC. RFA warrants evaluation vs. surgery for treatment of small-size metastases and primary NSCLC in a subset of patient who remained to be defined; however, a randomized trial would be difficult to conduct because of the anticipated difficulties of obtaining patient consent to be randomized among so different treatments. The role as RFA in palliation or debulking of larger tumor or of more widespread disease must be defined.
References
Ahmed M, Liu Z, Afzal KS et al (2004) Radiofrequency ablation: effect of surrounding tissue composition on coagulation necrosis in a canine tumor model. Radiology 230:761–767
Goldberg SN, Gazelle GS, Compton CC, McLoud TC (1995) Radiofrequency tissue ablation in the rabbit lung: efficacy and complications. Acad Radiol 2:776–784
Miao Y, Ni Y, Bosmans H et al (2001) Radiofrequency ablation for eradication of pulmonary tumor in rabbits. J Surg Res 99:265–271
Hakime H, Hines-Peralta A, Peddi H et al (2007) Combination of radiofrequency ablation with antiangiogenics therapy for tumor ablation efficacy: study in mice. Radiology 244:464–470
de Baere T, Palussiere J, Auperin A et al (2006) Mid-term local efficacy and survival after radiofrequency ablation of lung tumors with a minimum follow-up of 1 year: prospective evaluation. Radiology 240:587–596
Lee JM, Han JK, Chang JM et al (2006) Radiofrequency ablation in pig lungs: in vivo comparison of internally cooled, perfusion and multitined expandable electrodes. Br J Radiol 79:562–571
de Baere T, Rehim MA, Teriitheau C et al (2006) Usefulness of guiding needles for radiofrequency ablative treatment of liver tumors. Cardiovasc Intervent Radiol 29:650–654
Hoffmann RT, Jakobs TF, Lubienski A et al (2006) Percutaneous radiofrequency ablation of pulmonary tumors—is there a difference between treatment under general anaesthesia and under conscious sedation? Eur J Radiol 59:168–174
Mulier S, Ni Y, Jamart J et al (2005) Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg 242:158–171
Yasui K, Kanazawa S, Sano Y et al (2004) Thoracic tumors treated with CT-guided radiofrequency ablation: initial experience. Radiology 231:850–857
Lee JM, Jin GY, Goldberg SN et al (2004) Percutaneous radiofrequency ablation for inoperable non–small cell lung cancer and metastases: preliminary report. Radiology 230:125–134
Antoch G, Kuehl H, Vogt FM et al (2002) Value of CT volume imaging for optimal placement of radiofrequency ablation probes in liver lesions. J Vasc Interv Radiol 13:1155–1161
Gupta S, Krishnamurthy S, Broemeling LD et al (2005) Small (≤2-cm) subpleural pulmonary lesions: short- versus long-needle-path CT-guided biopsy—comparison of diagnostic yields and complications. Radiology 234:631–637
Tanaka J, Sonomura T, Shioyama Y et al (1996) “Oblique path”—the optimal needle path for computed tomography-guided biopsy of small subpleural lesions. Cardiovasc Intervent Radiol 19:332–334
Gillams AR, Lees WR (2008) Radiofrequency ablation of lung metastases: factors influencing success. Eur Radiol 18:672–677
Tominaga J, Miyachi H, Takase K et al (2005) Time-related changes in computed tomographic appearance and pathologic findings after radiofrequency ablation of the rabbit lung: preliminary experimental study. J Vasc Interv Radiol 16:1719–1726
Bojarski JD, Dupuy DE, Mayo-Smith WW (2005) CT imaging findings of pulmonary neoplasms after treatment with radiofrequency ablation: results in 32 tumors. AJR Am J Roentgenol 185:466–471
Jin GY, Lee JM, Lee YC et al (2004) Primary and secondary lung malignancies treated with percutaneous radiofrequency ablation: evaluation with follow-up helical CT. AJR Am J Roentgenol 183:1013–1020
Okuma T, Matsuoka T, Yamamoto A et al (2009) Assessment of early treatment response after CT-guided radiofrequency ablation of unresectable lung tumours by diffusion-weighted MRI: a pilot study. Br J Radiol 82:989–994
Beland MD, Wasser EJ, Mayo-Smith WW, Dupuy DE (2010) Primary non-small cell lung cancer: review of frequency, location, and time of recurrence after radiofrequency ablation. Radiology 254:301–307
Ruers TJ, Joosten JJ, Wiering B et al (2007) Comparison between local ablative therapy and chemotherapy for non-resectable colorectal liver metastases: a prospective study. Ann Surg Oncol 14:1161–1169
Zhu JC, Yan TD, Morris DL (2008) A systematic review of radiofrequency ablation for lung tumors. Ann Surg Oncol 15:1765–1774
Nguyen CL, Scott WJ, Young NA et al (2005) Radiofrequency ablation of primary lung cancer: results from an ablate and resect pilot study. Chest 128:3507–3511
Hiraki T, Sakurai J, Tsuda T et al (2006) Risk factors for local progression after percutaneous radiofrequency ablation of lung tumors: evaluation based on a preliminary review of 342 tumors. Cancer 107:2873–2880
Okuma T, Matsuoka T, Yamamoto A et al (2009) Determinants of local progression after computed tomography-guided percutaneous radiofrequency ablation for unresectable lung tumors: 9-year experience in a single institution. Cardiovasc Intervent Radiol [Epub ahead of print]
Lencioni R, Crocetti L, Cioni R et al (2008) Response to radiofrequency ablation of pulmonary tumours: a prospective, intention-to-treat, multicentre clinical trial (the RAPTURE study). Lancet Oncol 9:621–628
Anderson EM, Lees WR, Gillams AR (2009) Early indicators of treatment success after percutaneous radiofrequency of pulmonary tumors. Cardiovasc Intervent Radiol 32:478–483
Shiono S, Ishii G, Nagai K et al (2005) Predictive factors for local recurrence of resected colorectal lung metastases. Ann Thorac Surg 80:1040–1045
Lee JM, Han JK, Kim HC et al (2007) Switching monopolar radiofrequency ablation technique using multiple, internally cooled electrodes and a multichannel generator: ex vivo and in vivo pilot study. Invest Radiol 42:163–171
Tacke J, Mahnken A, Roggan A, Gunther RW (2004) Multipolar radiofrequency ablation: first clinical results. Rofo 176:324–329
Brace CL, Hinshaw JL, Laeseke PF et al (2009) Pulmonary thermal ablation: comparison of radiofrequency and microwave devices by using gross pathologic and CT findings in a swine model. Radiology 25:705–711
Wright AS, Lee FT Jr, Mahvi DM (2003) Hepatic microwave ablation with multiple antennae results in synergistically larger zones of coagulation necrosis. Ann Surg Oncol 10:275–283
Wolf FJ, Grand DJ, Machan JT et al (2008) Microwave ablation of lung malignancies: effectiveness, CT findings, and safety in 50 patients. Radiology 247:871–879
Hiraki T, Gobara H, Takemoto M et al (2006) Percutaneous radiofrequency ablation combined with previous bronchial arterial chemoembolization and followed by radiation therapy for pulmonary metastasis from hepatocellular carcinoma. J Vasc Interv Radiol 17:1189–1193
Elias D, Baton O, Sideris L et al (2004) Local recurrences after intraoperative radiofrequency ablation of liver metastases: a comparative study with anatomic and wedge resections. Ann Surg Oncol 11:500–505
Lu DS, Raman SS, Limanond P et al (2003) Influence of large peritumoral vessels on outcome of radiofrequency ablation of liver tumors. J Vasc Interv Radiol 14:1267–1274
de Baere T, Deschamps F, Briggs P et al (2008) Hepatic malignancies: percutaneous radiofrequency ablation during percutaneous portal or hepatic vein occlusion. Radiology 248:1056–1066
Anai H, Uchida BT, Pavcnik D et al (2006) Effects of blood flow and/or ventilation restriction on radiofrequency coagulation size in the lung: an experimental study in swine. Cardiovasc Intervent Radiol 29:838–845
Wright AS, Sampson LA, Warner TF et al (2005) Radiofrequency versus microwave ablation in a hepatic porcine model. Radiology 236:132–139
Steinke K, Arnold C, Wulf S, Morris DL (2003) Safety of radiofrequency ablation of myocardium and lung adjacent to the heart: an animal study. J Surg Res 114:140–145
Iguchi T, Hiraki T, Gobara H et al (2007) Percutaneous radiofrequency ablation of lung tumors close to the heart or aorta: evaluation of safety and effectiveness. J Vasc Interv Radiol 18:733–740
de Baere T, Dromain C, Lapeyre M et al (2005) Artificially induced pneumothorax for percutaneous transthoracic radiofrequency ablation of tumors in the hepatic dome: initial experience. Radiology 236:666–670
Hiraki T, Gobara H, Mimura H et al (2010) Does tumor type affect local control by radiofrequency ablation in the lungs? Eur J Radiol 74:136–141
Dupuy DE, Zagoria RJ, Akerley W et al (2000) Percutaneous radiofrequency ablation of malignancies in the lung. AJR Am J Roentgenol 174:57–59
Simon CJ, Dupuy DE, Dipetrillo TA et al (2007) Pulmonary radiofrequency ablation: long-term safety and efficacy in 153 patients. Radiology 243:268–275
Grieco CA, Simon CJ, Mayo-Smith WW et al (2006) Percutaneous image-guided thermal ablation and radiation therapy: outcomes of combined treatment for 41 patients with inoperable stage I/II non-small-cell lung cancer. J Vasc Interv Radiol 17:1117–1124
Yamakado K, Hase S, Matsuoka T et al (2007) Radiofrequency ablation for the treatment of unresectable lung metastases in patients with colorectal cancer: a multicenter study in Japan. J Vasc Interv Radiol 18:393–398
Yan TD, King J, Sjarif A et al (2006) Percutaneous radiofrequency ablation of pulmonary metastases from colorectal carcinoma: prognostic determinants for survival. Ann Surg Oncol 13:1529–1537
Yamagami T, Kato T, Iida S et al (2005) Efficacy of manual aspiration immediately after complicated pneumothorax in CT-guided lung biopsy. J Vasc Interv Radiol 16:477–483
Yoshimatsu R, Yamagami T, Terayama K et al (2009) Delayed and recurrent pneumothorax after radiofrequency ablation of lung tumors. Chest 135:1002–1009
Radvany MG, Allan PF, Frey WC et al (2005) Pulmonary radiofrequency ablation complicated by subcutaneous emphysema and pneumomediastinum treated with fibrin sealant injection. AJR Am J Roentgenol 185:894–898
Abu-Hijleh M, Blundin M (2010) Emergency use of an endobronchial one-way valve in the management of severe air leak and massive subcutaneous emphysema. Lung 188(3):253–257
Vaughn C, Mychaskiw G 2nd, Sewell P et al (2002) Massive hemorrhage during radiofrequency ablation of a pulmonary neoplasm. Anesth Analg 94:1149–1151
Herrera LJ, Fernando HC, Perry Y et al (2003) Radiofrequency ablation of pulmonary malignant tumors in nonsurgical candidates. J Thorac Cardiovasc Surg 125:929–937
Yamakado K, Takaki H, Takao M et al (2010) Massive hemoptysis from pulmonary artery pseudoaneurysm caused by lung radiofrequency ablation: successful treatment by coil embolization. Cardiovasc Intervent Radiol 33:410–412
Hess A, Palussier J, Goyers J et al (2009) Lung radiofrequency in single lung patients: feasibility, tolerance and efficacy (abstract 1207). In: Paper presented at Cardiovascular and Interventional Radiological Society of Europe
Rose SC, Fotoohi M, Levin DL, Harrell JH (2002) Cerebral microembolization during radiofrequency ablation of lung malignancies. J Vasc Interv Radiol 13:1051–1054
Ghaye B, Bruyere PJ, Dondelinger RF (2006) Nonfatal systemic air embolism during percutaneous radiofrequency ablation of a pulmonary metastasis. AJR Am J Roentgenol 187:W327–W328
Okuma T, Matsuoka T, Tutumi S et al (2007) Air embolism during needle placement for CT-guided radiofrequency ablation of an unresectable metastatic lung lesion. J Vasc Interv Radiol 18:1592–1594
Jin GY, Lee JM, Lee YC, Han YM (2004) Acute cerebral infarction after radiofrequency ablation of an atypical carcinoid pulmonary tumor. AJR Am J Roentgenol 182:990–992
Hiraki T, Mimura H, Gobara H et al (2009) Two cases of needle-tract seeding after percutaneous radiofrequency ablation for lung cancer. J Vasc Interv Radiol 20:415–418
Acknowledgments
We declare honoraria for Boston Scientific Corporation for RF ablation workshops, and a research grant from Covidien.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Baère, T. Lung Tumor Radiofrequency Ablation: Where Do We Stand?. Cardiovasc Intervent Radiol 34, 241–251 (2011). https://doi.org/10.1007/s00270-010-9860-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-010-9860-8