Abstract
Purpose
The efficacy of drug-eluting balloons has been demonstrated in clinical trials. The drug predominantly used is paclitaxel because of its lipophilic properties and the rapid onset of action. The aim of the investigation was to evaluate the feasibility and efficacy of an alternative balloon coating with rapamycin that can be applied on site.
Methods
The balloon coating (3.0/18 and 3.0/12 mm, Cathy No. 4, Translumina GmbH) with rapamycin was conducted with a coating machine (Translumina GmbH). Concentrations were 2, 2 × 2, 3, and 4 %. Measurements regarding the amount of substance released to the vessel wall were carried out on explanted porcine coronaries by means of ultraviolet and visible-light spectroscopy. Inflation time varied between 30 and 120 s. The biological effect of the coating was evaluated in a porcine peripheral overstretch and stent implantation model.
Results
The amount of rapamycin on the balloon surface ranged from 558 ± 108 μg for the 2 % solution to 1,441 ± 228 μg in the 4 % solution. An amount of 95 ± 63–193 ± 113 μg was released into the vessel wall. The quantitative measurements of the angiographic examinations 4 weeks after treatment revealed a reduction of diameter stenosis from 20.6 ± 17.4 % in the control group to 11.6 ± 5.5 % in the drug-eluting balloon group.
Conclusion
A balloon coating with rapamycin omitting an excipient is possible with a dose-adjustable coating machine. However, the biological effects are moderate, which make further optimization of the coating process and evaluation of appropriate excipients necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of local drug-delivering techniques for attenuation of restenosis has been widely applied in the form of drug-eluting stents. Several substances have been evaluated for this purpose for coronary as well as peripheral application such as sirolimus, zotarolimus, everolimus, and paclitaxel [1–4]. In coronary intervention, these stents have gained wide acceptance. However, in patients with more complex lesions in bifurcations or risk factors for restenosis such as diabetes, the performance is limited. More than that, stent thrombosis associated with the drug coating limits the use of these devices. Non-stent-based drug delivery by a drug-eluting balloon (DEB) has become an emerging technology to apply a sufficient amount of drug into the vessel wall to limit the process of restenosis while omitting the placement of a stent. Another favorable feature of DEB is the theoretically more homogenous distribution of the drug to the vessel wall compared to the stent struts.
In peripheral vessels, this technique is emerging as well, while requirements differ regarding regions with high movement and torque as well as long lesions in upper leg vessels. The possibility to limit restenosis in superficial femoral artery disease has been demonstrated by Werk et al. and Tepe et al. [5, 6]. The balloon used in the Thunder Trial was a modified Paccocath with paclitaxel used as the effective substance. Also, below-the-knee intervention is a possible field of application for DEB because there is a high prevalence of diabetic patients, a high necessity for repeat interventions with target lesion revascularization. Several studies are underway to define the role of DEB for this application [7].
Other products are also being developed and tested that differ in terms of the carrier substance and drug concentration. There is ongoing discussion about the most efficient carrier to use. At present, less discussion seems to exist regarding the drug of choice for the purpose of balloon coating. Paclitaxel, a highly lipophilic diterpenoid, provides a high local tissue concentration and is potent at low nanomolar concentrations. It promotes the stabilization of microtubules and inhibits cell processes dependent on microtubule turnover [8]. Unlike sirolimus, the drug paclitaxel is able to inhibit smooth muscle cell proliferation even after a short time of incubation. An amount of about 3 μg/mm² of paclitaxel on the currently produced balloons has favorable results in studies that use paclitaxel-coated balloons in coronary and peripheral vessels.
However, some features justify the investigation on alternative substances as sirolimus (rapamycin). Endothelialization of the treated vessel might be more considerably delayed after paclitaxel administration, and there is evidence that the use of 2.0–3.0 μg/mm² of paclitaxel may lead to delayed vascular healing [9]. The migration of endothelial cells is not as thoroughly inhibited by sirolimus [10], while paclitaxel is an inhibitor of smooth muscle cells and endothelial cells via nonspecific inhibition of microtubule disassembly. Rapamycin also demonstrates anti-inflammatory effects next to its antiproliferative features. Therefore, a possible result of the use of rapamycin could be the more moderate impact to the vessel wall in case of sufficient drug deposition. This might be a favorable feature, especially for long lesions in the superficial femoral artery and in the movement section of the popliteal artery. Only limited data exist regarding the optimal inflation time and biological effects of rapamycin as a balloon coating.
The aim of the study was to evaluate a rapamycin coating of a commercially available percutaneous transluminal angioplasty (PTA) balloon in regard to homogeneity, stability, release, substance transfer into the vessel wall, and in vivo effects in porcine peripheral arteries.
Materials and Methods
In Vitro Release Measurements and Tissue Concentration
The balloon coating with rapamycin was conducted with an on-site coating machine (SCM7; Translumina GmbH, Hechingen, Germany). In brief, a compliant Cathy No. 4 percutaneous transluminal coronary angioplasty balloon catheter (Translumina GmbH) is placed into a disposable coating cardridge, which is inserted into the coating device. The spraying function of the second-generation coating device delivers a homogenous film onto the surface of the folded balloon. Balloon sizes used were 3.0 mm in diameter and 12 mm for tests on concentration and duration of inflation, or 18 mm for rinsing time experiments in total length (n = 4 for each concentration). The concentrations of the rapamycin solutions used for the in vitro coating experiments were 2, 2 × 2, 3, and 4 %. The double coating by a repeat 2 % application was included to evaluate the effect of multiple coating layers on the release of the substance. Evaluation of the balloon surface regarding homogeneity in the folded condition and characteristics after inflation was performed by optical microscopy and scanning electron microscopy.
Measurements regarding the release of rapamycin to the vessel wall were carried out on explanted porcine hearts. After explantation, vessel segments were rinsed with saline solution until all blood content was removed; segments were then cut into appropriate sections. After weighting the tissue, coated balloons were introduced and inflated for 30, 60, or 120 s. The segments were placed into tubes containing 25 mL of saline solution and placed in a shaker for 5, 30 min, or 24 h. Vessel segments and balloons were rinsed with a methanol-based excipient and the amount of rapamycin determined by ultraviolet and visible-light spectrophotometry with a measuring range of 200–400 nm (Specord 210, Analytik Jena).
Animal Experiments
The animal studies were conducted after approval of the local committee for animal protection. Ten female domestic pigs with a mean weight of 35.9 ± 6.4 kg were used for the study. Twenty-four hours before the interventional procedure, animals received 300 mg of clopidogrel. Postinterventional medication consisted of 75 mg clopidogrel daily p.o. and 250 mg of acetylsalicylic acid p.o. The medication was maintained until the animals were humanely killed after 28 days.
Premedication for the interventional procedure consisted of atropin 0.05 mg/kg body weight, azaperon 2.0 mg/kg body weight, followed by midazolam 0.2 mg/kg body weight and ketamine 14.0 mg/kg body weight i.m. For intubation, propofol 2.0–5.0 mg/kg body weight was administered. For general anesthesia, isoflurane 1.8–2.5 vol% and fentanyl 0.02–0.15 mg/kg body weight was provided intravenously. Anesthesia was maintained by isofluran 0.8–1.8 vol% and fentanyl 30–100 μg/kg body weight.
After cutdown of the common carotid artery, a 6F sheath (Terumo) was inserted, and a 0.0035-inch guide wire (Terumo) was advanced into the external femoral artery. Heparin 100–200 IU/kg body weight was provided intra-arterially. After placement of a 6F multipurpose angiographic guiding catheter (Cordis, Warren) into the femoral artery an angiographic run was performed by hand injection of 10 mL of iopromide 370 (Ultravist, Bayer Helathcare, Grenzach) and documented digitally on an flouroscopy C arm. A 0.0014-inch guide wire was used for placement of a bare metal stent (Yukon Choice, Translumina GmbH) into the selected vessel segment in the distal femoral/popliteal artery. The stent implantation served as an overstretch model, with a ratio of 1:1.2. Inflation pressure was adjusted according to the diameter measurement of the angiographic run. Subsequently, the monorail balloon (3.5/40 mm) was advanced and inflated for 120 s. The devices were coated by the above-described technology. Postimplantation angiography was used to document absence of vasospasm or dissection. Both hind limbs were treated in one session.
Four weeks after the interventions, repeat angiography was performed and recorded for further quantitative angiographic analysis. After euthanasia, the vessel segments were explanted, rinsed with 0.9 % saline solution, and perfusion fixed with 4 % paraformaldehyde. Part of the stented segments were embedded into methacrylate, which allowes for preparation of the samples including the stent struts and therefore prevents damage to the tissue. Specimens were stained with Masson–Goldner for further morphometric analysis by dedicated image analysis software (Qwin, Leica). For histological examination and immunohistochemical staining, the stent struts were carefully removed before embedding the tissue in paraffin. On these specimen, immunohistochemical staining was conducted for CD41 (endothelial cells) and proliferating cell nuclear antigen/DAPI (4′,6-diamidino-2-phenylindole) to assess proliferating cells. Evaluation of endothelial coverage was performed with a semiquantitative scoring system, with zero correlating with no coverage and three with full coverage. A proliferation index was determined as the proportion of proliferating cells in relation to the total amount of cells in one examined field of vision.
Statistical Analysis
Values are provided as mean ± standard deviation. For statistical analysis, a one-sided t test was conducted. For analysis, JMP 10.0 (SAS Institute, Cary, NC, USA) was used. Graphs were drawn with SigmaPlot 6.0 (Systat Software, San Jose, CA, USA). A p value of 0.05 was considered to be statistically significant.
Results
Balloon Coating
The coating of the balloons was conducted in the folded condition with an on-site coating device with a rotating injector. On scanning electron microscopy, the layer on the surface of the folded balloon appeared relatively homogenous. An accumulation of the applied substance in the folds was visible. After inflation, thin clefts in the layer and small flakes could be seen (Fig. 1). Light microscopy made small clusters of the substance on the surface visible after the balloon was inflated (Fig. 2).
Influence of Coating Concentration
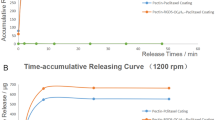
The different concentrations of the solutions used for coating (2, 2 × 2, 3, 4 %) of the 3.0/12 mm balloons (n = 4 for each group) led to a corresponding increase in the amount of substance on the surface of 558 ± 108, 771 ± 212, 1,054 ± 188 and 1,441 ± 228 μg. With an inflation time of 60 s, the higher coating concentrations increased the substance release to the vessel wall from 100 ± 23 μg with a 2 % and 95 ± 63 μg with the 3 % coating solution up to 167 ± 45 μg (4 %) and 193 ± 113 μg with a double coating using the 2 × 2 % rapamycin solution. The influence on the amount released to the vessel walls is shown in Fig. 3.
Influence of the coating concentration on substance transfer. The amount of substance on the balloon increased with the concentration of the coating solution (2, 2 × 2, 3, and 4 %) from 558 ± 108 to 771 ± 212, 1,054 ± 188 and 1,441 ± 228 μg, respectively. The transfer to the tissue was 100 ± 23 μg (2 % solution), 95 ± 63 μg (3 % solution), 167 ± 45 μg (4 % solution), and 193 ± 113 μg in case of the double coating with a 2 % rapamycin solution
Duration of Dilatation
The dilatation time was varied at 30, 60, and 120 s. The balloons (3.0/12 mm, n = 3 in each group) were coated with a 2 % rapamycin solution, which resulted in a mean amount on the surface of 582 ± 157, 558 ± 198 and 819 ± 151 μg, respectively. Under the different dilatation durations, with a contact time of 30 s, only about 4 % (21 ± 8 μg) of the rapamycin was transferred to the vessel wall, while 60 and 120 s resulted in 18 % (100 ± 23 μg) and 10 % (75 ± 25 μg) transfer of the rapamycin coating, respectively. The correlation between the inflation time and the amount released to the tissue can be gathered from Fig. 4.
Alteration of Rinsing Time
After inflation of the 3.0/18 mm balloons, vessel segments were rinsed with saline for different time intervals to simulate blood flow and consecutive removal of the substance from the tissue (n = 2 per setting). The mean amount of rapamycin applied to the surface of the balloons in the 5, 30 min, and 24 h groups during the coating process was 708 ± 75, 737 ± 76, and 872 ± 54 μg, respectively. The remaining rapamycin levels on the balloons after the inflation of 60 s were 633 ± 74, 588 ± 22, and 466 ± 166 μg.
After the specified rinsing time, the fluid contained 11 ± 5, 68 ± 23, and 296 ± 75 μg of rapamycin that was washed off from the vessel wall. The transfer into the wall of the explanted vessels was measured as 64 ± 4, 81 ± 31, and 109 ± 38 μg.
In Vivo Experiments
There was no direct procedure-related death. Of ten animals, three died during the observation period. The remainder of the animals survived until repeat angiography.
Quantitative Angiography
Repeat angiography was conducted on day 28 for quantitative evaluation. The reference diameter in the control group was larger than in the rapamycin-coated balloon group, with 2.85 ± 0.55 and 2.57 ± 0.54 mm, respectively. Therefore, a similar minimal diameter resulted in a different stenosis grade. The percentual stenosis regarding the diameter was 20.6 ± 17.4 % in the control group and 11.6 ± 5.5 % in the rapamycin-coated balloon group, although this did not reveal a statistically significant difference at an alpha level of 0.05 (Fig. 5). Representative angiograms preceding sacrifice of the animals are shown in Fig. 6.
Morphometric and Histological Analysis
The morphometric measurements revealed a slightly larger luminal area in case of the rapamycin group (4.18 ± 2.05 mm²) compared to the control group (3.59 ± 2.83 mm²). The neointimal area in the control group was 0.6 ± 0.05 mm² and was 0.54 ± 0.2 mm² in the rapamycin-coated balloon group, whereas only one slice per stented segment was investigated, possibly missing the maximal stenosis grade. Methacrylate sections from both groups are shown in Fig. 7. Immunohistochemical staining revealed a mean endothelial score of 2.7 in the vessel segments treated with an uncoated balloon versus 2.4 in the group receiving a rapamycin-coated balloon treatment. A further trend was visible in case of the proliferation index representing the fraction of proliferating cells in the intimal layer identified by proliferating cell nuclear antigen staining compared to the total cell count. A proportion of 0.52 of cells proliferated in the PTA-only group, while the vessels treated with rapamycin-coated balloons had a proportion of 0.39.
Discussion
During the initial use of antiproliferative drugs as device coatings, rapamycin has been on par with paclitaxel, with studies on these two far outnumbering the ones that use other substances. Many studies directly comparing the two substances as a coating for stent devices have demonstrated superiority of rapamycin eluting stent over paclitaxel eluting stent regarding, e.g., major adverse cardiac events, stent thrombosis, and outcome in diabetic patients, but these results can only be applied for the coronary use. There are data suggesting a lower in-stent restenosis rate after implantation of Cypher than with Taxus stents [11]. However, with coating of balloon catheters, paclitaxel became the more interesting substance as a result of a number of features, especially the effectiveness at low concentrations. Paclitaxel with a slightly lower molecular weight of 853.92 g/mol stabilizes microtubule polymers in the dividing cell, while rapamycin (MW 914.17 g/mol) acts via the intracellular mTOR (mammalian target of rapamycin) by association with the intracellular receptor FKBP12 and thereby blocking progression of the cell cycle from the G1 to the S phase. In vitro and in vivo studies demonstrated that sirolimus prevents T cell proliferation, as well as the migration and proliferation of smooth muscle cells. Its potential to inhibit neointimal hyperplasia was first reported by Gallo et al. [12] in a porcine coronary stent restenosis model.
Both rapamycin and paclitaxel are highly lipophilic substances that are transferred to the vessel wall even after a short contact duration with paclitaxel, with an irreversible effect after short exposure [13]. Twenty-five percent of the substance is supposed to be retained 48 h after dilatation. Our experiments demonstrated a remaining amount of rapamycin of 109 ± 38 μg in the vessel wall with 872 ± 54 μg initially loaded onto the balloon after being washed for 24 h.
The favorable results of larger scale clinical evaluations of the paclitaxel-coated balloon catheters in the coronary and peripheral vessels underline the potential of this drug, particularly because thrombosis does not seem to be of major concern with balloon coating; the substance is not retained over a comparably long period of time, as with stents.
However, as the use of these catheters is increasing and they are used in long lesions and infrapopliteal arteries, the aim of this investigation was to test whether a rapamycin solution applied to a standard balloon with an on-site coating device would suffice to transport a nameable amount of the substance to the vessel wall and induce a biological effect.
The relevance of a shielding substance and an excipient to transport the substance to the arterial tissue has been highlighted since the first attempt to coat balloons directly with paclitaxel. There is up to 80 % loss of substance according to early studies with this balloon [14]. The use of excipients does decrease this amount; however, the long-term effects are not completely known in the currently used substances. The paccocath-technology used in the SeQuent Please balloon (B.Braun) loaded with 3 μg/mm² uses the radiological contrast agent iopromide as carrier substance also acting as a spacer between the paclitaxel molecules. Cotavance DEB with Paccocath technology (MedRad/Bayer Healthcare) 3 μg/mm², also applies iopromide. It has the advantage of being approved for intra-arterial use and is eliminated quickly. Shellac (Dior II, Eurocor), 3 μg/mm², is used in cosmetics, food coating, and drug encapsulation in tablets, but it has not been used so far as an adjunct in intravenous or intra-arterial injection; it is also approved by the U.S. Food and Drug Administration. Butyryl-triheyl-citrate (BTHC) as used in the PanteraLux (Biotronik) balloon; 3 μg/mm² is usually applied in blood transportation bags as a plasticizer. The freepac technology used in the in.pact drug-eluting balloon (Medtronic/Invatec) uses urea as hydrophilic separator molecules for the 3 μg/mm² paclitaxel to balance lipophilic and hydrophilic features of the coating and increase the transfer into the tissue. Only elutax does get along without the use of an excipient, but the exact formulation of the coating solution remains unknown. There is a substantial difference in the performance of the different formulations of coatings between the above-mentioned combinations with paclitaxel [15]. In a dose–response study, Kelsch et al. [16] found a paclitaxel coated balloon catheter with urea to result in less loss on inflation and passage than an iopromide coating. Comparing two other paclitaxel-coated balloons, Cremers et al. [17] found the first-generation Dior balloon and a PTA control balloon to perform inferior to the Paccocath technique. The release of a Dior balloon has been reported to be approximately 35–70 % [18]; however, when different methods are used, the amount of the substance applied to the vessel wall with early coating strategies was 6–8 % [19, 20]. Depending on the coating concentration and the duration of inflation, the proportion transferred to the surrounding tissue reached between 10 and 18 % in our in vitro setting.
Because no direct conclusion can be drawn from the relation of drug-eluting stent to the balloon coating, the necessary amount of rapamycin on a DEB to induce a biological effect is hard to estimate and is more dependent on release and tissue retention than the total amount on the balloon. There was a substantial difference in the total amount of substance in our tests; however, we were able to apply a maximum of 1,441 ± 228 μg of rapamycin onto the folded surface. With a balloon 3 mm in diameter and 12 mm long, this correlates with an amount per square millimeter of 12.8 μg/mm² in the case of the highest coating concentration and 4.9 μg/mm² for the standard coating with the 2 % rapamycin–ethanol coating solution, with the latter used in the animal model.
Regarding use as a stent coating, Wessely et al. [21] reported on an amount of rapamycin by a single coating of 195 ± 33 and 317 ± 45 μg/cm² with a double coating placed onto a stent surface with the coating technique used in this study. In a similar setting, Hausleiter et al. [22] coated Yukon stents with a 0.5–2 % rapamycin solution, receiving 138 ± 14–479 ± 26 μg rapamycin/cm². The Cypher stent has a surface concentration of 140 μg of rapamycin/cm², while the amount of paclitaxel on the Taxus stent is about 100 μg/cm² [23].
According to our measurements of rapamycin in the explanted vessels, a 2 × 2 % coating resulted in a higher tissue transfer despite a smaller total amount than a single 4 % dilution. This might be the result of different layers of rapamycin with a double coating, possibly producing a more durable layer using the rotating injector technology, which has to be further investigated. The variation of contact time revealed a markedly better release of the drug to the vessel wall after 60 s compared to an inflation time of 30 s. A longer inflation duration did not improve the tissue concentration, which matches the observations made with the paclitaxel eluting balloons, where most of the substance is released within the first 60 s [24].
The observed biological effect in our animal model was rather moderate with respect to neointimal formation and attenuation of restenosis. Because of the segmenting of the stented vessel segments for further morphometric and histological analysis, we were not able to systematically correlate the diameter stenosis on angiography to the maximum stenosis on morphometric evaluation. Effects of the substance were also visible on histologic examination regarding the amount of reendothelialization and the proliferation index, suggesting a transport of rapamycin into the tissue up to a certain amount. Although a further aim of this rapymacin coating is an increase of the released amount, the necessary quantity remains unclear. A balanced effect on the prevention of neointimal hyperplasia and healing of the vessel is desirable [25].
To date, the results can solely be compared with other animal models. Albrecht et al. [26] investigated the use of paclitaxel-coated balloon catheters (excipient iopromide) in femoropopliteal arteries of 20 swine with concomitant implantation of a stent with an amount of the drug of 480 μg paclitaxel, with positive results for the paclitaxel-coated balloons. By using zotarolimus-coated balloon catheters, Cremers et al. [27] found the effectiveness of inhibiting neointimal hyperplasia in a manner similar to that of paclitaxel-coated devices in coronary arteries. Other positive results with zotarolimus were demonstrated by a study conducted by Granada et al. [28] that used zotarolimus-coated balloons (300 μg/cm²) in injured superficial femoral arteries in hypercholesterolemic swine. This suggests the feasibility of alternative coatings to paclitaxel and encourages further investigations regarding the use of the described method to apply a coating with rapamycin or other substances using an on-site device.
Limitations of the study are as follows. Next to being a preliminary study, the investigation did not address the issue of the time course of drug retention in the in vivo setting. Further, additive substances in the coating solution to control release into the tissue were not analyzed. However, as in vitro and in vivo data suggest, a successful transport of rapamycin to the site of dilatation, next to the use of excipients the future improvements with this coating technique will include different formulations to control the configuration of the coating layer on the balloon surface.
References
Werner M, Schmidt A, Freyer M et al (2012) Sirolimus-eluting stents for the treatment of infrapopliteal arteries in chronic limb ischemia: long-term clinical and angiographic follow-up. J Endovasc Ther 19:12–19
Mehilli J, Byrne RA, Wieczorek A, Intracoronary stenting, angiographic restenosis investigators et al (2008) Test efficacy of rapamycin-eluting stents with different polymer coating strategies (ISAR-TEST-3). Randomized trial of three rapamycin-eluting stents with different coating strategies for the reduction of coronary restenosis. Eur Heart J 29:1975–1982
de Waha A, Cassese S, Park DW et al (2012) Everolimus-eluting versus sirolimus-eluting stents: an updated meta-analysis of randomized trials. Clin Res Cardiol 101:461–467
Dake MD, Ansel GM, Jaff MR, Zilver PTX investigators et al (2011) Paclitaxel-eluting stents show superiority to balloon angioplasty and bare metal stents in femoropopliteal disease: 12-month Zilver PTX randomized study results. Circ Cardiovasc Interv 4:495–504
Werk M, Langner S, Reinkensmeier B et al (2008) Inhibition of restenosis in femoropopliteal arteries: paclitaxel-coated versus uncoated balloon: femoral paclitaxel randomized pilot trial. Circulation 118:1358–1365
Tepe G, Zeller T, Albrecht T et al (2008) Local delivery of paclitaxel to inhibit restenosis during angioplasty of the leg. N Engl J Med 358:689–699
Zeller T, Schmitmeier S, Tepe G et al (2011) Drug-coated balloons in the lower limb. J Cardiovasc Surg (Torino) 52:235–243
Finn AV, John M, Nakazawa G et al (2009) Differential healing after sirolimus, paclitaxel, and bare metal stent placement in combination with peroxisome proliferator-activator receptor gamma agonists: requirement for mTOR/Akt2 in PPARgamma activation. Circ Res 105:1003–1012
Radke PW, Joner M, Joost A et al (2011) Vascular effects of paclitaxel following drug-eluting balloon angioplasty in a porcine coronary model: the importance of excipients. EuroIntervention 30(7):730–737
Liuzzo JP, Ambrose JA, Coppola JT (2005) Sirolimus- and taxol-eluting stents differ towards intimal hyperplasia and re-endothelialization. J Invasive Cardiol 17:497–502
Silber S (2005) Cypher versus taxus: are there differences? J Interv Cardiol 18:441–446
Gallo R, Padurean A, Jayaraman T et al (1999) Inhibition of intimal thickening after balloon angioplasty in porcine coronary arteries by targeting regulators of the cell cycle. Circulation 99:2164–2170
De Labriolle A, Pakala R, Bonello L et al (2009) Paclitaxel-eluting balloon: from bench to bed. Catheter Cardiovasc Interv 73:643–652
Scheller B, Hehrlein C, Bocksch W et al (2006) Treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. N Engl J Med 355:2113–2124
Joner M, Byrne RA, Lapointe JM et al (2011) Comparative assessment of drug-eluting balloons in an advanced porcine model of coronary restenosis. Thromb Haemost 105:864–872
Kelsch B, Scheller B, Biedermann M et al (2011) Dose response to paclitaxel-coated balloon catheters in the porcine coronary overstretch and stent implantation model. Investig Radiol 46:255–263
Cremers B, Biedermann M, Mahnkopf D et al (2009) Comparison of two different paclitaxel-coated balloon catheters in the porcine coronary restenosis model. Clin Res Cardiol 98:325–330
Pósa A, Nyolczas N, Hemetsberger R et al (2010) Optimization of drug-eluting balloon use for safety and efficacy: evaluation of the 2nd generation paclitaxel-eluting DIOR-balloon in porcine coronary arteries. Catheter Cardiovasc Interv 76:395–403
Scheller B, Speck U, Abramjuk C et al (2004) Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation 110:810–814
Speck U, Scheller B, Abramjuk C et al (2006) Neointima inhibition: comparison of effectiveness of non-stent-based local drug delivery and a drug-eluting stent in porcine coronary arteries. Radiology 240:411–418
Wessely R, Hausleiter J, Michaelis C et al (2005) Inhibition of neointima formation by a novel drug-eluting stent system that allows for dose-adjustable, multiple, and on-site stent coating. Arterioscler Thromb Vasc Biol 25:748–753
Hausleiter J, Kastrati A, Wessely R et al (2005) Investigators of the individualizable durg-eluting stent system to abrogate restenosis project. Prevention of restenosis by a novel drug-eluting stent system with a dose-adjustable, polymer-free, on-site stent coating. Eur Heart J 26:1475–1481
Silber S (2003) Paclitaxel-eluting stents: are they all equal? An analysis of six andomized controlled trials in de novo lesions of 3, 319 patients. J Interv Cardiol 16:485–490
Waksman R, Pakala R (2009) Drug-eluting balloon: the comeback kid? Circ Cardiovasc Interv 2:352–358
van der Giessen WJ, Sorop O, Serruys PW et al (2009) Lowering the dose of sirolimus, released from a nonpolymeric hydroxyapatite coated coronary stent, reduces signs of delayed healing. JACC Cardiovasc Interv 2:284–290
Albrecht T, Speck U, Baier C et al (2007) Reduction of stenosis due to intimal hyperplasia after stent supported angioplasty of peripheral arteries by local administration of paclitaxel in swine. Investig Radiol 42:579–585
Cremers B, Milewski K, Clever YP et al (2012) Long-term effects on vascular healing of bare metal stents delivered via paclitaxel-coated balloons in the porcine model of restenosis. Catheter Cardiovasc Interv 80:603–610
Granada JF, Milewski K, Zhao H et al (2011) Vascular response to zotarolimus-coated balloons in injured superficial femoral arteries of the familial hypercholesterolemic Swine. Circ Cardiovasc Interv 4:447–455
Acknowledgments
The study was supported by the BMBF, support code 0313745.
Conflict of interest
Isabelle Braun and Boris Behnisch are employees of Translumina GmbH, which provided the devices used in this study. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmehl, J., von der Ruhr, J., Dobratz, M. et al. Balloon Coating with Rapamycin Using an On-site Coating Device. Cardiovasc Intervent Radiol 36, 756–763 (2013). https://doi.org/10.1007/s00270-013-0583-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-013-0583-5