Abstract
Purpose
The purpose of the study was to evaluate the angiographic findings and results of embolotherapy in the management of lumbar artery trauma.
Methods
All patients with lumbar artery injury who underwent angiography and percutaneous embolization in a state trauma center within a 10-year period were retrospectively reviewed. Radiological information and procedural reports were reviewed to assess immediate angiographic findings and embolization results. Long-term clinical outcome was obtained by communication with the trauma physicians as well as with chart review.
Results
In a 10-year period, 255 trauma patients underwent abdominal aortography. Eleven of these patients (three women and eight men) suffered a lumbar artery injury. Angiography demonstrated active extravasation (in nine) and/or pseudoaneurysm (in four). Successful selective embolization of abnormal vessel(s) was performed in all patients. Coils were used in six patients, particles in one and gelfoam in five patients. Complications included one retroperitoneal abscess, which was treated successfully. One patient returned for embolization of an adjacent lumbar artery due to late pseudoaneurysm formation.
Conclusions
In hemodynamically stable patients, selective embolization is a safe and effective method for immediate control of active extravasation, as well as to prevent future hemorrhage from an injured lumbar artery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Retroperitoneal vascular injury from blunt and penetrating trauma must be promptly addressed. The early use of computed tomography (CT) and angiography is imperative to diagnose and manage these patients in the setting of trauma. Posttraumatic retroperitoneal hemorrhage most often involves actively bleeding pelvic vessels that require embolization. Rarely, the retroperitoneal hemorrhage can be the result of lumbar arterial injury. Lumbar arteries are difficult to control operatively. Both the anterior or posterior surgical approaches put the ureter and lumbar plexus at risk [1]. Abdominal and pelvic arteriography is routinely performed in patients with a retroperitoneal hematoma in the effort to localize and treat a suspected arterial injury, by the use of percutaneous transcatheter embolization. CT and angiographic findings of lumbar artery injury have been previously described in a small number of prior publications [2–8]. In this work, we describe our experience in the angiographic diagnosis and percutaneous embolotherapy in the management of lumbar arterial trauma.
Materials and Methods
Institutional review board approval was obtained for this retrospective study, designed to evaluate the angiographic findings and percutaneous management of arterial trauma in our interventional radiology section, serving a level 1 State Trauma center. Between November 1991 and November 2001, 255 patients underwent arteriography, for evaluation of suspected intra-abdominal arterial trauma. The study enrolled 148 males, (age range: 14–77 years) and 107 females (age range: 15–70 years). All patients underwent an initial-contrast enhanced CT examination of the abdomen and pelvis. From January 1991 to February 1997, CT scans were performed on a GE High Speed Advantage Scanner (GE Medical Systems, Milwaukee, WI) with 150 cc of intravenous contrast, employing 5-mm scans through the abdomen and pelvis using a 10-mm interval. From February 1997 to August 1999, CT scans were performed on a GE High Speed CTI scanner using 5-mm images at 8-mm intervals. Delayed images of the lower abdomen and pelvis were obtained in 2/11 patients (Table 1, patients 3 and 9).
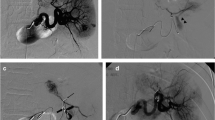
Retrospective review identified 11/255 (4.3%) patients who underwent arteriography and percutaneous embolization for the management of lumbar arterial injury. Arteriograms and corresponding procedural reports were reviewed to assess immediate angiographic findings and embolization results. All procedures were performed under intravenous antibiotic coverage. This was given as a prophylactic one dose (Ancef 1 g during the procedure; Table 1, patients 3, 5, 6, and 8–11) or as part of their global care (Ancef 1 g intravenously every 8 h; Table 1, patients 1, 2, 4, and 7). Indications for arteriography in trauma victims were as follows: (1) clinical symptomatology suggestive of internal hemorrhage: hypotension and or tachycardia; (2) blood transfusion requirements; (3) diminishing hemoglobin and hematocrit; (4) flank and/or low abdominal/pelvic pain accompanied by retroperitoneal hematoma demonstrated on CT (Fig. 1a) and/or exploratory laparotomy.
Short and long-term clinical outcomes and complications of embolization were recorded by patient chart review and after direct communication with the referral trauma physicians.
Technique
Arteriography was performed using the standard percutaneous technique via the common femoral artery (CFA) in all patients. A 5.5F–6F sheath with a hemostasis valve was advanced via the CFA and positioned so that the tip was at the level of the external iliac artery (EIA). Initially, an abdominal and pelvic aortogram (Fig. 1b) was performed with the use of a 5F multiple side hole angiographic catheter (Omniflush or pigtail; Angiodynamics, Glenn Falls, NY). The catheter was exchanged over a 0.035-in. wire for a selective angiographic catheter (Sos Omni 2, C-2, H-1,; Angiodynamics, Glenn Falls, NY), which was used to identify the origin of the lumbar artery. Selective catheterization of the vessel was performed in all cases. This was most commonly achieved by a Sos Omni 2 catheter (Angiodynamics, Glenn Falls, NY) via which selective diagnostic arteriography was performed. In all cases, a coaxial microcatheter (Renegade, Boston Scientific, Cork Ireland, or Tracker, Boston Scientific/Target Therapeutics, Fremont CA, USA) was introduced via the 5 F catheter. The catheter was advanced into the area of extravasation and, when possible, past the area of extravasation over an appropriate guidewire (Transcend EX floppy, Taper 16; Boston Scientific/Target Therapeutics). Embolization was performed with the Vortex microcoils (Boston Scientific, Cork, Ireland). Prior to the deployment of the microcoil, a Transend EX floppy wire (Boston Scientific/ Target Therapeutics) was advanced via the microcatheter and into the area of extravasation to confirm secure position prior to coil delivery. The coils were usually flushed via the catheter with the use of a 1–3-cc syringe filled with saline. If this was not possible, the microcoil wire pusher was utilized. In cases where microcoil delivery was thought to be unsafe (microcatheter moving out from the vessel when a wire is advanced), embolization was performed with the use of Surgifoam (gelatin sponge) pledgets (Ethicon, Somerville, NJ) and or contour particles (Boston Scientific, Fremont, CA) using flow-directed techniques. When gelfoam was used, it was cut in small pledgets that were placed in the end hole of a 1-cc syringe and flushed into the area of extravasation via the microcatheter. Postembolization arteriography confirmed occlusion of the embolized vessel (Fig. 1c). Adjacent caudal and cranial lumbar arteries were evaluated prior to the termination to the procedure.
Definitions
Angiographic findings suggestive of arterial trauma included active extravasation, abrupt arterial vessel cutoff, severe arterial spasm, arterial wall irregularity, abnormal arteriovenous communication, and aneurysm.
-
Immediate technical success of embolotherapy was defined as immediate cessation of flow into the area of extravasation and/or the abnormal arterial branch.
-
Immediate clinical success was defined as the sustained cessation of symptomatology suggestive of hemorrhage.
-
Long-term clinical success was defined as the persistent absence of symptomatology suggestive of hemorrhage, preservation of hematocrit levels within normal limits, and no evidence of delayed complication.
-
Technical failures were defined as the inability to perform embolization of a bleeding artery; persistent bleeding/extravasation after embolization; repeated or delayed extravasation, aneurysm, or arteriovenous fistula formation at the embolized site and the inability to identify an injured lumbar artery.
-
Immediate complications were defined as nontarget vessel embolization, including embolization of the artery of Adamkiewicz, resulting in spinal cord infarction and paralysis, and vascular injury, including puncture-site hematoma and rhabdomyolysis from lumbar muscle infarction.
-
Delayed complications were defined as infection, including abscess formation, loss of muscular mass/volume from the embolized area, and neurologic defects from the embolized area.
Results
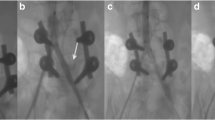
Eleven trauma patients (three women and eight men) were found to suffer a lumbar artery injury that required arteriography and embolization. All 11 patients had a retroperitoneal hematoma, demonstrated by CT (Fig. 1A). A blush in the retroperitoneum was seen in 2 and a pseudoaneurysm was identified in 1 (Fig. 2A) of the 11 CT examinations. Arteriography demonstrated active extravasation (Fig. 1B) involving 10 sites in 8 patients and pseudoaneurysms (Fig. 2B) in 4 patients (Table 1). One technical failure was recorded in a patient who developed a pseudoaneurysm 4 days after the initial arteriogram. This patient had a bleeding lumbar artery that was embolized successfully in the initial study. He complained of persistent back pain and had a decreasing hemoglobin and hematocrit level (Table 1, patient 2). He returned for repeat arteriography that demonstrated delayed pseudoaneurysm formation in an adjacent lumbar artery. This vessel was evaluated during the initial procedure by selective arteriography and no abnormality was appreciated, even retrospectively. All patients had distal lumbar artery injury. There was no extravasation or injury demonstrated near the origin (2 cm) of the lumbar vessel from the aorta. Successful selective embolization of all abnormal vessel(s) was performed. Immediate technical success was documented in all 11 patients (12 procedures). Microcoils were used in six patients and gelfoam was used in four patients. A combination of particles and gelfoam was used in one patient. Microcoils were placed beyond (one patient), across (two ptients), or just proximal (one patient) to a pseudoaneurysm (Fig. 2C). Follow-up ranged from 21 days to 72 months (Table 1). Mean and median follow-up was 23 and 19 months, respectively.
A 36-year-old male who was stabbed in the right flank. (A) CT scan shows a pseudoaneurysm in the right retroperitoneum. (B) Selective right first lumbar artery injection showing a pseudoaneurysm and no evidence of the artery of Adamkiewicz. (C) Selective right first lumbar artery injection showing successful coil embolization of the pseudoaneurysm.
There was no nontarget embolization. No case of rhabdomyolysis or paralysis was seen. In a patient with multiple intra-abdominal injuries, a retroperitoneal abscess developed 4 days after embolization of the right second and third lumbar arteries. The abscess was successfully treated percutaneously and the patient was doing well on his last follow-up 5 months after the embolization procedure (Table 1, patient 5). Three patients died during the follow-up period, but no death was related to the procedure. One of the three deaths had a long, complicated course after the initial trauma (Table 1, patient 2). The patient suffered a motor vehicle accident with multiple intraabdominal trauma and underwent many intra-abdominal procedures after embolization, including many surgical debridements for decubiti ulcers. He died 90 days after the embolization procedure due to staphylococcal sepsis attributed to his decubiti ulcers. One patient was discharged and was in good condition at 30 days after the embolization procedure (Table 1, patient 3). When we attempted to obtain further follow-up, we found a notification that he had expired outside the institution and from unknown cause. The third death occurred 3 years and 3 months after the procedure as a result of myocardial infarction complicated by cardiac arrhythmia and fatal asystole (Table 1, patient 4).
Discussion
The retroperitoneum is a relatively vascular region. Many collateral vessels supply any particular region of the retroperitoneum [5]. This can explain why once a bleeding artery is under control, collateral supply to the same region could result in new bleeding [5]. This is one of the major reasons why the surgeons avoid exploration of the retroperitoneum in the setting of trauma [5]. Thus, it is extremely important to evaluate vessels above and below an identified injured lumbar artery during arteriography. Nearby vessels should be selectively evaluated due to a high probability of multiple injuries during the initial trauma and in order to identify a collateral supply to or distal to the area of the previously embolized lumbar artery [2]. Sclafani et al. reported how multiple vessels could supply the same bleeding site [2]. Similarly, a low intercostal vessel from above can supply the first lumbar artery, or the most inferior lumbar artery might have collaterals from iliac vessels. We, therefore, advocate performing selective injections of all arterial branches in the vicinity of an identified traumatized lumbar artery. An aortogram alone is not sufficient to evaluate collateral flow or demonstrate adjacent arterial injury. Thus, selective arteriography of all arterial branches must be performed in the area of the injury.
Another concern in embolizing lumbar arteries is the artery of Adamkiewicz. The main arterial supply of the dorso-lumbar spinal cord is usually derived from a single anterior radiculo-medullary artery called the artery of Adamkiewicz. It has a characteristic hairpin turn inferiorly to supply the anterior spinal artery. Embolization of the artery of Adamkiewicz might result in spinal cord infarction and paralysis. This complication must be conveyed to the patient and/or his family while discussing the procedure and its benefits and risks. Although the artery of Adamkiewicz did not originate from any of the damaged vessels in our series, in up to 19% of patients, the artery of Adamkiewicz was supplied from a first or second lumbar artery [9]. It rarely originates from a lumbar vessel below the second lumbar artery [9, 10]. The vessel usually originates from the proximal portion of the lumbar artery. Therefore, it is important to identify the presence of an artery of Adamkiewicz and to embolize an injured vessel as distal from the origin of the lumbar artery as possible. Lumbar artery embolization might also result in retroperitoneal infarction [11]. This can result in a number of complications. Acutely, the patient might experience rhabdomyolysis from lumbar muscle infarction. Creatine kinase and potassium levels must be followed closely in these patients. If these levels rise acutely, renal failure can ensue. A late complication of retroperitoneal infarction is infection. This occurred in one of the patients who were embolized with gelfoam. In a prior publication, it was discussed that particles might go distally and, theoretically at least, are at increased risk for tissue infarction [3, 11]. Since the advent of coaxial microcatheters that can safely deliver microcoils in the majority of cases, we suggest their use in lumbar artery embolization as the treatment of choice.
No cases of proximal lumbar artery injury (within 2 cm from origin of the vessel from the aorta) were seen in this series. In a proximal lumbar artery injury, the pressure in the vessel is high and could result in rapid bleeding. Although we could not find any documentation in the literature, we assume that individuals who have an injury close to the origin of a lumbar artery from the aorta succumb in the field secondary to rapid, uncontrolled, and fatal bleeding.
Patients might stabilize after an initial lumbar artery embolization only to rebleed from a late pseudoaneurysm formation or from a nearby nondetected injured artery [12, 13]. This known late complication of trauma [12, 13] was seen in one patient in this study. This lumbar artery was injured in the initial trauma; however, the vessel was not identified as injured during arteriography. The resultant aneurysm formed a short time after the first angiogram and embolization. This finding demonstrates the value of performing selective arteriography in all adjacent vessels especially in stable patients, where the clinical situation affords the additional time needed. Alternatively, hemodynamically unstable patients can be aggressively managed in the intensive care unit after arteriography and embolization, whereas preservation of the arterial sheath for a short period might prove life-saving, in cases where there are clinical findings and high level of suspicion for possible persistent or recurrent bleeding which was not identified angiographically. This permits fast repeat arteriography and embolization as needed. The value of arteriography and embolization in hemodynamically stable trauma victims has been established [1–2, 4, 7, 14–16]. The value of the technique has also been shown in hemodynamically metastable patients prior to or after exploratory laparotomy [14–17]. We certainly follow and advocate this approach in a level 1 State Trauma center where close coordination and multidisciplinary management of the trauma victim between trauma surgeons and interventional radiologists exists. In hemodynamically stable and metastable or controlled trauma patients, selective embolization is a safe and effective method to control active extravasation, as well as to prevent future hemorrhage and delayed complications from an injured lumbar artery. We believe that a superselective technique and a thorough evaluation of the lumbar arteries and nearby vessels in the region of trauma followed by transcatheter embolization is the treatment of choice in the management of lumbar artery trauma.
The role of angioembolization in trauma is evolving. The larger question of whether embolotherapy affects outcome in comparison to surgery alone or conservative management cannot be definitively addressed by any retrospective observational study. This and similar studies [14–17] can, however, form the basis for considering a future prospective evaluation of outcome in arterial trauma. In general, embolotherapy in trauma requires a multimodality approach with close coordination between the trauma surgeon and the interventional radiologist. Thus, in institutions with appropriately trained interventional radiologist and supporting trauma service, arteriography and embolization is the treatment of choice.
References
Fisher RG, Ben-Menachem T (1985) Embolization procedures in trauma: the abdomen-extraperitoneal. Semin Intervent Radiol 2:148–157
Sclafani SJ, Florence LO, Phillips TF, et al. (1987) Lumbar arterial injury: radiologic diagnosis and management. Radiology 165(3):709–714
Armstrong NN, Zarvon NP, Sproat IA, et al. (1997) Lumbar artery hemorrhage: unusual cause of shock treated by angiographic embolization. J Trauma 42(3):544–545
Chang J, Katzen B, Sullivan K (1978) Transcatheter gelfoam embolization of posttraumatic bleeding pseudoaneurysms. Am J Roentgenol 131:645–650
Marty B, Sanchez L, Wain R, et al. (1998) Endovascular treatment of a ruptured lumbar artery aneurysm: case report and review of the literature. Ann Vasc Surg 12(4):379–383
Kalangos A, Walder B, Faidutti B (1998) Ruptured artery pseudoaneurysm: a diagnostic dilemma in retroperitoneal hemorrhage after abdominal trauma. J Trauma 45(4):829–832
Maull K, Rozycki G, Vinsant O, et al. (1987) Retroperitoneal injuries: pitfalls in diagnosis and management. South Med J 80(9):1111–1115
Hulnick D, Naidich D, Balthazar E, et al. (1984) Lumbar artery pseudoaneurysm: CT demonstration. J Comput Assist Tomogr 8(3):570–572
Takase K, Sawamura Y, Igarashi K, et al. (2002) Demonstration of the artery of Adamkiewicz at multi-detector row helical CT. Radiology 223(1):39–45
Lo D, Vallee JN, Spelle L, et al. (2002) Unusual origin of the artery of Adamkiewicz from the fourth lumbar artery. Neuroradiology 44(2):153–157
Doppman J, Chiro G (1976) Paraspinal muscle infarction. Radiology 119:609–613
Siablis D, Panagopoulos C (2003) Delay diagnosis of false aneurysm after lumbar arterial injury: Treatment with endovascular embolization: ACSE report. Spine 28(4):E71–E73
Haydu P, Chang J (1978) Transcatheter arterial embolization of a traumatic lumbar artery false aneurysm. Surgery 84(2):228–291
Kushimpto S, Arai M (2003) The role of interventional radiology in patient’s requiring damage control laparotomy. J Trauma-Injury Infect Crit Care 54(1):171–176
Sofocleous CT, Hinrichs C, Hubbi B, et al. (2005) Angiographic findings and embolotherapy in renal arterial trauma. Cardiovasc Intervent Radiol 28(1):39–47
Mohr AM, Lavery RF, Barone A, et al. (2003) Angiographic embolization for liver injuries: low mortality, high morbidity. J Trauma 55(6):1077–1081; discussion 1081–1082
Dinkel H-P, Danuser H, Triller J (2002) Blunt renal trauma: minimally invasive management with microcatheter embolization: experience in nine patients. Radiology 223:723–730
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sofocleous, C.T., Hinrichs, C.R., Hubbi, B. et al. Embolization of Isolated Lumbar Artery Injuries in Trauma Patients. Cardiovasc Intervent Radiol 28, 730–735 (2005). https://doi.org/10.1007/s00270-003-0117-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-003-0117-7