Abstract
Background
Access to timely and quality surgical care is limited in low- and middle-income countries (LMICs). Telemedicine, defined as the remote provision of health care using information, communication and telecommunication platforms have the potential to address some of the barriers to surgical care. However, synthesis of evidence on telemedicine use in surgical care in LMICs is lacking.
Aim
To describe the current state of evidence on the use and distribution of telemedicine for surgical care in LMICs.
Methods
This was a scoping review of published and relevant grey literature on telemedicine use for surgical care in LMICs, following the PRISMA extension for scoping reviews guideline. PubMed-Medline, Web of Science, Scopus and African Journals Online databases were searched using a comprehensive search strategy from 1 January 2010 to 28 February 2021.
Results
A total of 178 articles from 53 (38.7%) LMICs across 11 surgical specialties were included. The number of published articles increased from 2 in 2010 to 44 in 2020. The highest number of studies was from the World Health Organization Western Pacific region (n = 73; 41.0%) and of these, most were from China (n = 69; 94.5%). The most common telemedicine platforms used were telephone call (n = 71, 39.9%), video chat (n = 42, 23.6%) and WhatsApp/WeChat (n = 31, 17.4%). Telemedicine was mostly used for post-operative follow-up (n = 71, 39.9%), patient education (n = 32, 18.0%), provider training (n = 28, 15.7%) and provider-provider consultation (n = 16, 9.0%). Less than a third (n = 51, 29.1%) of the studies used a randomised controlled trial design, and only 23 (12.9%) reported effects on clinical outcomes.
Conclusion
Telemedicine use for surgical care is emerging in LMICs, especially for post-operative visits. Basic platforms such as telephone calls and 2-way texting were successfully used for post-operative follow-up and education. In addition, file sharing and video chatting options were added when a physical assessment was required. Telephone calls and 2-way texting platforms should be leveraged to reduce loss to follow-up of surgical patients in LMICs and their use for pre-operative visits should be further explored. Despite these telemedicine potentials, there remains an uneven adoption across several LMICs. Also, up to two-thirds of the studies were of low-to-moderate quality with only a few focusing on clinical effectiveness. There is a need to further adopt, develop, and validate telemedicine use for surgical care in LMICs, particularly its impact on clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery can ameliorate up to one-third of the global burden of disease, yet access to safe and quality surgical care is limited, especially in low- and middle-income countries (LMICs) [1]. According to the World Bank, low-income countries are those with a gross national income (GNI) per capita of $1045 or less in 2020, lower-middle-income countries are those with GNI per capita between $1046 and $4095, upper-middle-income countries are those with GNI per capita of $4096 and $12,695 while high-income countries (HICs) are those with a GNI per capita of $12,696 or more [2]. Compared to HICs, persons requiring surgery in LMICs experience longer delays to care and have worse peri-operative mortality [3]. These delays and poor peri-operative outcomes may result from multiple barriers including lack of surgical care providers, long travel distances to health facilities, and limited means of transportation [4,5,6]. Thus, efforts aimed at addressing these barriers could facilitate improvement in access to surgical care and outcomes in LMICs.
Telemedicine, defined as the remote provision of healthcare services using information communication and technology platforms, is a rapidly evolving and expanding component of healthcare services [7]. It has the potential to address various barriers to health care provision by improving access to clinical services and facilitating continuity of care and education [7, 8]. Surgery was historically considered a specialty where face-to-face care was a necessity. However, telemedicine is increasingly utilized for various aspects of surgical care including patient and provider education [9,10,11,12]. In fact, the ongoing COVID-19 pandemic, and the need for social distancing to minimize transmission, has accelerated the use of telemedicine for various health care services globally [13], including surgery [14].
Studies in HICs have demonstrated the use of telemedicine to triage persons with surgical conditions for in-person visits, reduce unnecessary transfers and provision of more timely care [15,16,17,18]. The potential of telemedicine to overcome some of the surgical barriers such as lack of access to surgical specialists and long travel distances to health care facilities have also been widely shown in HICs [15, 19, 20]. However, the surgical burden of disease, barriers to care, health care infrastructure and resources, as well as technological advancement level in LMICs, differ from that of HICs. Thus, available evidence from HICs cannot be directly translated to LMICs. Synthesis of evidence on the potential and extent of use of telemedicine for surgical care in LMICs is essential but lacking. Therefore, the objective of this review is to describe the current state of evidence about the use and distribution of telemedicine for surgical care in LMICs. These results can be used to identify aspects of telemedicine use for surgical care with strong available evidence, existing knowledge gaps and to provide direction for future studies.
Methods
The methodological framework for scoping reviews by Arksey and O’Malley was utilized [21]. The reporting of the study findings was guided by Preferred Reporting Items for Systematic Reviews and Meta-analysis Extension for Scoping Review (PRISMA-ScR) [22].
Search strategy
Peer-reviewed articles on the use of telemedicine in surgery in LMICs published from 1 January 2010 to 28 February 2021 were identified from five databases: PubMed-Medline, Scopus, Web of Science, Cochrane library, and African Journals Online. A search strategy was formulated in consultation with an experienced university medical librarian and the senior authors (JD and KC). The search strategy included a combination of Medical Search Headings (MeSH) terms and keywords for the three key concepts: telemedicine, surgery, and LMICs. Keywords were derived from title, abstract and keywords of relevant studies identified during an initial preliminary review. Similar or different concepts were merged using Boolean operators “OR” and “AND”, respectively (Appendix 1). Lastly, references of identified reviews were hand-searched for additional articles.
Eligibility criteria
Published studies on telemedicine by any surgical specialty and during any part of the patient care pathway in LMICs were included. All study types, including observational and experimental studies, qualitative, quantitative, and mixed-method studies, were included. Case reports, commentaries, books, blog posts, conference abstracts, and studies focusing on robotic surgery (due to the complexities and limitations around its use in LMICs) were excluded. Studies that were not performed in a LMIC, and not written in English or where full-text translation using Google Translate was not possible, were also excluded.
Study selection
Duplicates were excluded after importing the studies into Covidence review software (Veritas Health Innovation, Melbourne, Australia). Titles and abstract screening for inclusion or exclusion were independently conducted by two reviewers. Where there were disagreements between the two reviewers, a consensus was reached with the opinion of a third reviewer. Studies included by the reviewers proceeded for full-text screening, following the same format.
Quality of evidence
The mixed-method appraisal tool was adopted for the critical appraisal of the included studies. This validated tool is used to assess the methodological quality of interventional, observational, and qualitative studies, paying specific attention to the study objectives, design, sampling, data collection, results, and study limitations [23].
Data extraction and charting
Data from included studies were extracted into a standardized Microsoft Excel form by two independent reviewers with discrepancies in the extracted information resolved through discussion and consensus. Data extracted included study details such as the publication year, country, setting (rural, urban), aim, study design, study population, surgical specialty, and telemedicine platforms. Telemedicine platforms were categorized into telephone calls, video platforms (video calls/conferencing, i.e., Zoom, Microsoft Teams, Skype), instant messaging (all forms of communications on WeChat and/or WhatsApp), texts (including SMS, 2-way texting, audio messages), emails, mHealth applications, and online communication platforms (web-based applications that facilitated blogging, image upload, private messaging). The types of study outcomes were also extracted including implementation (usability, feasibility, acceptability), health systems effectiveness (accuracy of consultation, waiting time, cost, cancellation rate), and clinical outcomes (length of stay, morbidity, mortality).
Data analysis
This was a scoping review and the volume of studies, and their characteristics were summarized using descriptive statistics in IBM Statistical Package for Social Science (SPSS) (IBM Corps, Armonk, New York, USA).
Results
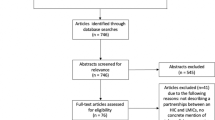
The initial search yielded 5048 studies from which 179 duplicate studies were removed. Title and abstracts of 4869 articles were screened of which 4318 did not meet the eligibility criteria and were removed. Full-text screening was conducted on 551 articles of which 173 were included in the final data extraction. Additional five relevant studies were found through hand searching of references and by performing a Google search engine query using the study search terms. Finally, 178 articles were included (Fig. 1). The total number of participants in the included studies in the review was 204 351. Detailed descriptions of the included studies can be found in Supplementary Table 1.
Characteristics of the included study
Of the 178 included studies, 174 (97.8%) were quantitative, 3 (1.7%) were qualitative, and 1 (0.5%) used mixed methods. Of the quantitative studies, 88 (50.3%) were prospective observational, 51(29.1%) were randomised controlled trials (RCT), 25 (14.3%) were retrospective observational, and 11 (6.3%) were non-randomised trials.
Quality of evidence of included studies
Of the 178 included studies, only 57 (32.0%) met all the five essential criteria for quality based on the appraisal checklist for their respective study designs. Sixty-seven (37.6%) studies lacked one essential component, while 54 (30.3%) studies lacked 2 or more of the essential components.
Geographical distribution of studies
The highest number of studies were from the World Health Organization (WHO) Western Pacific region (n = 73; 41.0%) and of these, most were from China (n = 69; 94.5%). The Eastern Mediterranean region had the lowest number of studies (n = 5; 2.8%) (Fig. 2). The number of studies was not associated with the country population. Some populous countries like Russia and Nigeria had fewer studies compared to less populous countries like Turkey and South Africa which had a higher number of studies.
Time trend
The number of publications increased over time, with the highest number of published studies recorded in 2020 (Fig. 3).
Telemedicine platforms
The three most common forms of technology used were telephone call (n = 71; 39.9%), video (n = 42; 23.6%), and instant messaging (n = 31; 17.4%) (Table 1).
Surgical specialties
Telemedicine was used by 11 surgical specialties. The most common five were general surgery (n = 35; 19.7%), surgical oncology (n = 21; 11.8%), paediatric surgery (n = 18; 10.1%), neurosurgery (n = 18; 10.1%), and plastic and reconstructive surgery (n = 16; 9.0%) (Table 2).
Telemedicine uses in surgery in LMICs
Telemedicine was used in surgery for clinical care, appointment reminders, patient education, and provider training. Clinical care included pre-operative assessment (n = 10, 5.6%) [24,25,26,27,28,29,30,31,32,33], post-operative assessment (n = 71, 39.9%) [34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105], and provider-provider consultations (n = 16, 9.0%) [106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121] (Table 3).
Outcomes
About half (n = 97, 54.5%) of the studies only reported implementation outcomes, including feasibility, usability and satisfaction with various telemedicine platforms. Some studies reported health system effectiveness (or process measures) such as surgery cancellations (n = 1, 0.6%), cost saving (n = 6, 3.4%), follow-up rate (n = 11, 6.2%), length of hospital stay (n = 1, 0.6%) and unnecessary referrals (n = 7, 3.9%). Only 22 (12.3%) studies reported clinical effectiveness; 2(1.1%) on mortality, 5 (2.8%) on morbidity, and 16 (9.0%) on patient anxiety, depression, or quality of life (Table 4).
Of the 23 studies that reported clinical effectiveness, 16 (69.5%) adopted a RCT design, 4 (17.4%) prospective descriptive, 1 (4.3%) non-randomised trial, 1 (4.3%) before and after and 1 (4.3%) retrospective descriptive design. The most common platforms used for these studies were telephone call (n = 10, 43.5%), WeChat (n = 6, 26.1%), Internet-/web-based platform (n = 4, 17.4%) and videoconferencing (n = 2, 8.7%).
Limitations of telemedicine use
Twenty-five (13.7%) studies reported limitations to telemedicine for surgical care in LMICs. These included Internet bandwidth, network instability and coverage [69, 78, 82, 122,123,124], high costs of technology set-up [55, 125], and safety, privacy and confidentiality concerns [117, 118, 126]. Poor image quality for asynchronous (where information transmission and response do not take place in real-time) telemedicine [127], inability to confirm delivery of information by SMS recipients [128, 129], and time zone differences for international collaborations and mentoring [31] were additional limitations that were reported. Another highlighted limitation was the inferiority of remote versus in-person physical examination [77, 81].
Discussion
This scoping review appraised evidence on the use of telemedicine for surgical care in LMICs. The volume of studies identified demonstrates that telemedicine in surgery is emerging in LMICs. However, less than a third of the studies were effectiveness studies adopting RCT design and only a few assessed clinical effectiveness. This corroborates a previous report from 2017 highlighting the scarcity of effectiveness studies of mHealth interventions in LMICs compared to HICs [130]. Although process and implementation measures are important, to truly show the benefit of mHealth interventions requires demonstration of improved or at least not worsened clinical outcomes. Therefore, more studies demonstrating the clinical effectiveness of telemedicine in surgery in LMICs are needed to inform evidence-based practice and appropriate health system responses.
In addition, studies were found in 53 (39%) of the 137 LMICs, with an unequal distribution within and across geographic regions. In this review, 41% of the studies were from the WHO Western Pacific region and 95% of those were conducted in China. A study by Abaza et al. reported similar findings to our study, with a significant concentration of studies in Asian countries [130]. There are several factors that could have contributed to the high usage of telemedicine for surgical care in China which include a higher rate of internet penetration, or the regulated cost of internet subscriptions [131]. Perhaps increasing Internet access and regulating and reducing the cost of Internet subscriptions may further encourage the adoption of telemedicine for surgical care in other LMICs.
Telemedicine usage in LMICs included provider-to-provider consultations, provider education, and remote patient assessments through simple technologies such as telephone calls, video conferencing and instant messaging. However, similar to what has been found in HICs, telemedicine was most commonly used for post-operative patient follow-up [132, 133]. Remote patient follow-up is increasingly being adopted as a strategy to reduce health care facility traffic and to prevent unnecessary travel by patients. In 2020, remote post-operative follow-up increased in both HICs [134] and LMICs due to the COVID-19 pandemic, evidenced by the volume of studies during this year. Future studies should further explore the clinical effectiveness of remote post-operative patient follow-up. Also, studies on the implementation and effectiveness of telemedicine use for pre-operative visits and providers’ education are required.
The lack and uneven distribution of surgical providers are significant barriers to surgical care in LMICs [4]. Our findings demonstrate that various telemedicine modalities were used to create regional and international platforms for provider education and clinical care. Communications between providers within and across countries can help clinicians deliver improved patient care. However, more studies demonstrating the clinical effectiveness of regional and international remote consultations and collaborations are needed in LMICs to inform evidence-based practice.
Strengths and limitations
Our conclusions on the extent of use of telemedicine for surgical care in LMICs were based on published studies. However, not all LMIC institutions publish their telemedicine practices. We did not assess the full text of some studies due to language restrictions and unavailability of full text. Also, studies focusing on robotic surgery were excluded. Therefore, we may have underestimated the scope and reach of surgical telemedicine in LMICs. Studies were of uneven geographical distribution; thus, the findings of this study may not be generalizable to all LMIC settings. Likewise, two studies were translated by Google Translate which may influence the accuracy of some findings. However, to the best of our knowledge, this scoping review is the first of its kind to describe telemedicine use in surgical care in LMICs. Our results can be used to inform future research and surgical health system strengthening.
Conclusion
This scoping review showed that telemedicine use for surgical care is emerging in LMICs, especially for post-operative visits. Basic platforms such as telephone calls and 2-way texting were successfully used for post-operative follow-up and education. In addition, file sharing and video chatting options were added when a physical assessment was required. Telephone calls and 2-way texting platforms such as WhatsApp and WeChat are easy-to-use, cheap and accessible and should be leveraged to reduce loss to follow-up of surgical patients in LMICs. There is a need to further explore the use and effectiveness of these basic platforms for pre-operative visits. Despite these telemedicine potentials, there remains an uneven adoption across several LMICs, evidenced by the unequal geographical distribution of studies. Likewise, up to two-third of the studies were of low-to-moderate quality with only a few focusing on clinical effectiveness. The ongoing COVID-19 pandemic presents a pressing context to further adopt, develop, and validate telemedicine use for surgical care in LMICs, particularly its impact on clinical outcomes.
Data availability
Not applicable.
References
Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624
The World Bank (2022) World Bank Country and Lending Groups [cited 2022 January 20]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups#:~:text=%EF%BB%BF%EF%BB%BF%20For%20the%20current,those%20with%20a%20GNI%20per
Biccard BM, Madiba TE, Kluyts H-L, Munlemvo DM, Madzimbamuto FD, Basenero A et al (2018) Perioperative patient outcomes in the African surgical outcomes study: a 7 day prospective observational cohort study. Lancet 391(10130):1589–1598
Holmer H, Lantz A, Kunjumen T, Finlayson S, Hoyler M, Siyam A et al (2015) Global distribution of surgeons, anaesthesiologists, and obstetricians. Lancet Glob Health 3:S9–S11
Ozgediz D, Jamison D, Cherian M, McQueen K (2008) The burden of surgical conditions and access to surgical care in low-and middle-income countries. Bull World Health Organ 86:646–647
Iddriss A, Shivute N, Bickler S, Cole-Ceesay R, Jargo B, Abdullah F et al (2011) Emergency, anaesthetic and essential surgical capacity in the Gambia. Bull World Health Organ 89:565–572
World Health Organisation (2010) Telemedicine: opportunities and developments in member states [cited 2021 14 August]. Available from: https://www.who.int/goe/publications/goe_telemedicine_2010.pdf
Williams AM, Bhatti UF, Alam HB, Nikolian VC (2018) The role of telemedicine in postoperative care. Mhealth 4:11
Harting MT, Wheeler A, Ponsky T, Nwomeh B, Snyder CL, Bruns NE et al (2019) Telemedicine in pediatric surgery. J Pediatr Surg 54(3):587–594
Park ES, Boedeker BH, Hemstreet JL, Hemstreet GP (2011) The initiation of a preoperative and postoperative telemedicine urology clinic. Medicine meets virtual reality, vol 18. IOS Press, pp 425–427
Vyas KS, Hambrick HR, Shakir A, Morrison SD, Tran DC, Pearson K et al (2017) A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg 78(6):736–768
Urquhart AC, Antoniotti NM, Berg RL (2011) Telemedicine—an efficient and cost-effective approach in parathyroid surgery. Laryngoscope 121(7):1422–1425
Bhaskar S, Bradley S, Chattu VK, Adisesh A, Nurtazina A, Kyrykbayeva S et al (2020) Telemedicine across the globe-position paper from the COVID-19 pandemic health system resilience PROGRAM (REPROGRAM) international consortium (Part 1). Front Public Health 8:644
Chao GF, Li KY, Zhu Z, McCullough J, Thompson M, Claflin J et al (2021) Use of telehealth by surgical specialties during the COVID-19 pandemic. JAMA Surg 156:620
Maurice AP, Punnasseril JEJ, King SE, Dodd BR (2020) Improving access to bariatric surgery for rural and remote patients: experiences from a state-wide bariatric telehealth service in Australia. Obes Surg 30(11):4401–4410
Schroeder C (2019) Pilot study of telemedicine for the initial evaluation of general surgery patients in the clinic and hospitalized settings. Surg Open Sci 1(2):97–99
Tolone S, Gambardella C, Brusciano L, Del Genio G, Lucido FS, Docimo L (2020) Telephonic triage before surgical ward admission and telemedicine during COVID-19 outbreak in Italy. effective and easy procedures to reduce in-hospital positivity. Int J Surg 78:123–125
Wallace DL, Jones SM, Milroy C, Pickford MA (2008) Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg 61(1):31–36
Gunter RL, Chouinard S, Fernandes-Taylor S, Wiseman JT, Clarkson S, Bennett K et al (2016) Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg 222(5):915–927
Bullard TB, Rosenberg MS, Ladde J, Razack N, Villalobos HJ, Papa L (2013) Digital images taken with a mobile phone can assist in the triage of neurosurgical patients to a level 1 trauma centre. J Telemed Telecare 19(2):80–83
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8(1):19–32
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P et al (2018) The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 34(4):285–291
Aoki L, Pereira IC, Matayoshi S (2019) Comparative study between conventional camera images and smartphone images for eyelid tumor telediagnosis. Revista do Colegio Brasileiro de Cirurgioes. https://doi.org/10.1590/0100-6991e-20192083
Dogan I, Eroglu U, Ozgural O, Al-Beyati ESM, Kilinc MC, Comert A et al (2018) Visualization of superficial cerebral lesions using a smartphone application. Turk Neurosurg 28(3):349–355
Latifi R, Mora F, Bekteshi F, Rivera R (2014) Preoperative telemedicine evaluation of surgical mission patients: should we use it routinely? Bull Am Coll Surg 99(1):17–23
Hughes C, Campbell J, Mukhopadhyay S, McCormack S, Silverman R, Lalikos J et al (2017) Remote digital preoperative assessments for cleft lip and palate may improve clinical and economic impact in global plastic surgery. Cleft Palate Craniofac J 54(5):535–539
Iyengar K, Paul M, Iyengar SD, Klingberg-Allvin M, Essén B, Bring J et al (2015) Self-assessment of the outcome of early medical abortion versus clinic follow-up in India: a randomised, controlled, non-inferiority trial. Lancet Glob Health 3(9):e537–e545
Shalabi HT, Price MD, Shalabi ST, Rodas EB, Vicuña AL, Guzhñay B et al (2017) Mobile gastrointestinal and endoscopic surgery in rural ecuador: 20 years’ experience of Cinterandes. Surg Endosc 31(12):4964–4972
Utriyaprasit K, Moore SM, Chaiseri P (2010) Recovery after coronary artery bypass surgery: effect of an audiotape information programme. J Adv Nurs 66(8):1747–1759
Ambroise B, Benateau H, Prevost R, Traore H, Hauchard K, Dia H et al (2018) The contribution of telemedicine to humanitarian surgery. J Cranio Maxillofac Surg 46(8):1368–1372
Fan KL, Avashia YJ, Dayicioglu D, DeGennaro VA, Thaller SR (2014) The efficacy of online communication platforms for plastic surgeons providing extended disaster relief. Ann Plast Surg 72(4):457–462
Furr MC, Larkin E, Blakeley R, Albert TW, Tsugawa L, Weber SM (2011) Extending multidisciplinary management of cleft palate to the developing world. J Oral Maxillofac Surg 69(1):237–241
Toefy Y, Skinner D, Thomsen S (2016) “Please don’t send us spam!” a participative, theory-based methodology for developing an mHealth intervention. JMIR mHealth uHealth 4(3):e6041
Phaff M, Aird J, Rollinson PD (2015) Delayed implants sepsis in HIV-positive patients following open fractures treated with orthopaedic implants. Injury 46(4):590–594
Uluer M, Sargin M, Akin F, Uluer E, Sahin O (2019) A randomized study to evaluate post-dural puncture headache after cesarean section: Comparison with median and paramedian approaches. Niger J Clin Pract 22(11):1564–1569
Liu X, Wang Z, Ren H, Ren A, Wang W, Yang X et al (2020) Evaluating postoperative anal fistula prognosis by diffusion-weighted MRI. Eur J Radiol 132:109294
Peng L, Ren L, Qin P, Su M (2016) The impact of patient-controlled analgesia on prognosis of patients receiving major abdominal surgery. Minerva Anestesiol 82(8):827–838
Li P, Wang W, Liu Y, Zhong Q, Mao B (2012) Clinical outcomes of 114 patients who underwent gamma-knife radiosurgery for medically refractory idiopathic trigeminal neuralgia. J Clin Neurosci 19(1):71–74
Wei SY, Li Q, Li SK, Zhou CD, Li FY, Zhou Y (2015) A new surgical technique of hymenoplasty. Int J Gynecol Obstet 130(1):14–18
Wang Q, Peng HL, He L, Zhao X (2015) Reproductive outcomes after previous cesarean scar pregnancy: follow up of 189 women. Taiwan J Obstet Gynecol 54(5):551–553
Gao Q, Yuan L, Wang WP, Shi H, Chen LQ (2014) Factors influencing response enthusiasm to telephone follow-up in patients with oesophageal carcinoma after oesophagectomy. Eur J Cancer Care 23(3):310–316
Du M, Liu B, Li M, Cao J, Liu D, Wang Z et al (2019) Multicenter surveillance study of surgical site infection and its risk factors in radical resection of colon or rectal carcinoma. BMC Infect Dis. https://doi.org/10.1186/s12879-019-4064-6
Jiang QL, Huang XH, Chen YT, Zhang JW, Wang CF (2016) Prognostic factors and clinical characteristics of patients with primary duodenal adenocarcinoma: a single-center experience from China. BioMed Res Int 2016:6491049
Jiang Y, Jia N, Zhu M, He Y, Che X, Lv T et al (2019) Comparison of survival and perioperative outcomes following simple and radical hysterectomy for stage II endometrial cancer: a single-institution, retrospective, matched-pair analysis. J Int Med Res 47(9):4469–4481
Wang Y, Ma JX, Yin T, Han Z, Cui SS, Liu ZP et al (2019) Correlation between reduction quality of femoral neck fracture and femoral head necrosis based on biomechanics. Orthop Surg 11(2):318–324
Bian Y, Xiang Y, Tong B, Feng B, Weng X (2020) Artificial intelligence-assisted system in postoperative follow-up of orthopedic patients: exploratory quantitative and qualitative study. J Med Internet Res 22(5):16896
Wang S, Li Y, Fei M, Zhang H, Wang J (2020) Clinical analysis of the effects of different anesthesia and analgesia methods on chronic postsurgical pain in patients with uniportal video-assisted lung surgery. J Cardiothorac Vasc Anesth 34(4):987–991
Gushchin AG, Crum AV, Limbu BB, Quigley EP, Seward MS, Tabin GC (2017) Simbu ptosis: an outreach approach to myogenic ptosis in eastern highlands of papua new guinea-experience and results from a high-volume oculoplastic surgical camp. Ophthalmic Plast Reconstr Surg 33(2):139–143
Tiwari D, Surianarayanan G, Sundararajan V, Karthikeyan P (2020) Virtual Telephonic follow-up for patients undergone septoplasty amid the COVID pandemic. Indian J Otolaryngol Head Neck Surg 73(1):30–32
Wang X, Xu B, Liang H, Jiang S, Tan H, Wang X et al (2018) Distribution characteristics and factors influencing oral warfarin adherence in patients after heart valve replacement. Patient Prefer Adherence 12:1641–1648
Starr N, Gebeyehu N, Tesfaye A, Forrester JA, Bekele A, Bitew S et al (2020) Value and feasibility of telephone follow-up in ethiopian surgical patients. Surg Infect 21(6):533–539
Babigumira JB, Barnhart S, Mendelsohn JM, Murenje V, Tshimanga M, Mauhy C et al (2020) Cost-effectiveness analysis of two-way texting for post-operative follow-up in Zimbabwe’s voluntary medical male circumcision program. PLoS ONE 15:e0239915
Thakar S, Rajagopal N, Mani S, Shyam M, Aryan S, Rao AS et al (2018) Comparison of telemedicine with in-person care for follow-up after elective neurosurgery: results of a cost-effectiveness analysis of 1200 patients using patient-perceived utility scores. Neurosurg Focus 44(5):E17
Ashry AH, Alsawy MF (2020) Doctor-patient distancing: an early experience of telemedicine for postoperative neurosurgical care in the time of COVID-19. Egypt J Neurol Psychiatry Neurosurg 56(1):1–8
Aiken AM, Wanyoro AK, Mwangi J, Mulingwa P, Wanjohi J, Njoroge J et al (2013) Evaluation of surveillance for surgical site infections in Thika hospital. Kenya J Hosp Infect 83(2):140–145
Nguhuni B, De Nardo P, Gentilotti E, Chaula Z, Damian C, Mencarini P et al (2017) Reliability and validity of using telephone calls for post-discharge surveillance of surgical site infection following caesarean section at a tertiary hospital in Tanzania. Antimicrob Resist Infect Control 6:43
Wang Y, Xu M, Li W, Mao Y, Da J, Wang Z (2020) It is efficient to monitor the status of implanted ureteral stent using a mobile social networking service application. Urolithiasis 48(1):79–84
Li C, Huang S, Su X, Zhang T, Jiang K (2019) Monitoring of home recovery using the 317-nursing mobile application following day-case surgery in children: perspectives from both nurses and patients. Medicine 98:31
Zhang QL, Huang ST, Xu N, Wang ZC, Cao H, Chen Q (2020) Application of remote follow-up via the WeChat platform for patients who underwent congenital cardiac surgery during the COVID-19 epidemic. Braz J Cardiovasc Surg 36(4):530–534
Chen M, Li P, Lin F (2016) Influence of structured telephone follow-up on patient compliance with rehabilitation after total knee arthroplasty. Patient Prefer Adherence 10:257–264
Ding XX, Zhao LQ, Cui XG, Yin Y, Yang HA (2020) Clinical observation of soft palate-pharyngoplasty in the treatment of obstructive sleep apnea hypopnea syndrome in children. World J Clin Cases 8(4):679–688
Zhang C, Zhu K, Lin Z, Huang P, Pan Y, Sun B et al (2020) Utility of deep brain stimulation telemedicine for patients with movement disorders during the COVID-19 outbreak in China. Neuromodulation 24:337–342
Li D, Zhang C, Gault J, Wang W, Liu J, Shao M et al (2017) Remotely programmed deep brain stimulation of the bilateral subthalamic nucleus for the treatment of primary parkinson disease: a randomized controlled trial investigating the safety and efficacy of a novel deep brain stimulation system. Stereotact Funct Neurosurg 95(3):174–182
Young S, Banza LN, Hallan G, Beniyasi F, Manda KG, Munthali BS et al (2013) Complications after intramedullary nailing of femoral fractures in a low-income country. Acta Orthop 84(5):460–467
Machado TMD, Santana RF, Vaqueiro RD, Santos CTBD, Alfradique de Souza P (2020) Telephone follow-up of the elderly after cataract surgery. Br J Vis Impair 38(2):184–195
Li LL, Gan YY, Zhang LN, Wang YB, Zhang F, Qi JM (2014) The effect of post-discharge telephone intervention on rehabilitation following total hip replacement surgery. Int J Nurs Sci 1(2):207–211
Rapp DE, Colhoun A, Morin J, Bradford TJ (2018) Assessment of communication technology and post-operative telephone surveillance during global urology mission. BMC Res Notes. https://doi.org/10.1186/s13104-018-3256-2
Wang J, Tong Y, Jiang Y, Zhu H, Gao H, Wei R et al (2018) The effectiveness of extended care based on internet and home care platform for orthopaedics after hip replacement surgery in China. J Clin Nurs 27(21–22):4077–4088
Li L, Ma Z, Wang W (2020) Influence of transitional care on the self-care ability of kidney transplant recipients after discharge. Ann Palliat Med 9(4):1958–1964
Zheng X, Zhao J, Wang Z, Jia B, Zhang Z, Guo J et al (2020) Postoperative online follow-up improves the quality of life of patients who undergo extraction of impacted madibular third molars: a randomized controlled trial. Clin Oral Investig 25:993–999
Wang QQ, Zhao J, Huo XR, Wu L, Yang LF, Li JY et al (2018) Effects of a home care mobile app on the outcomes of discharged patients with a stoma: a randomised controlled trial. J Clin Nurs 27(19–20):3592–3602
Xu LW, Vaca SD, Nalwanga J, Muhumuza C, Vail D, Lerman BJ et al (2018) Life after the neurosurgical ward in Sub-Saharan Africa: neurosurgical treatment and outpatient outcomes in Uganda. World Neurosurg 113:e153–e160
Feldacker C, Murenje V, Holeman I, Xaba S, Makunike-Chikwinya B, Korir M et al (2020) Reducing provider workload while preserving patient safety: a randomized control trial using 2-way texting for postoperative follow-up in Zimbabwe’s voluntary medical male circumcision program. J Acquir Immune Defic Syndr 83(1):16–23
Madsen C, Lough D, Lim A, Harshbarger RJ, Kumar AR (2015) Cleft and craniofacial care during military pediatric plastic surgery humanitarian missions. J Craniofac Surg 26(4):1097–1101
Zhang Z, Li F, Zhang H, Miao Z, Wei Y, Wang L et al (2019) Development and testing of a mobile phone app for risk estimation of gas volume expansion and intraocular pressure elevation in patients with intravitreous gas or air tamponade: interobserver assessment study. JMIR Mhealth Uhealth 7(6):e14592
Pan Y, Chen H, Chen H, Jin X, Zhu Y, Chen G (2020) Is electronic follow-up using a mobile phone application after mid-urethral sling placement feasible and efficient? World J Urol 39:863–869
Zhang P, Zhang YG, Liao LM, Shen JW, Yang YB, Zhang JZ et al (2019) Application of internet+-based Tsinghua PINS remote tech to improve sacral neuromodulation programming procedure. Int Urol Nephrol 51(4):627–632
Xu X, Cao Y, Luan X (2014) Application of 4G wireless network-based systemfor remote diagnosis and nursing of stomal complications. Int J Clin Exp Med 7(11):4554–4561
Shi Z, Jiang M, Zhao M, Zhang J, Zhang S, Li L et al (2020) A follow-up study on urodynamics of children after surgery for hypospadias. Chin J Pediatr Surg 41(9):819–823
Ma Y, Miao S, Zhou R, Zhang Q, Chen H, Liang Y (2021) Application of remote deep brain stimulation programming for parkinson’s disease patients. World Neurosurg 147:e255–e261
Lin Z, Zhang C, Zhang Y, Dai L, Voon V, Li D et al (2020) Deep brain stimulation telemedicine programming during the COVID-19 pandemic: treatment of patients with psychiatric disorders. Neurosurg Focus 49(6):1–5
Pathak A, Sharma S, Sharma M, Mahadik VK, Lundborg CS (2015) Feasibility of a mobile phone-based surveillance for surgical site infections in rural India. Telemed e-Health 21(11):946–949
Yadav SK, Jha CK, Mishra SK, Mishra A (2020) Smartphone-based application for tele-follow-up of patients with endocrine disorders in context of a LMIC: a compliance, satisfaction, clinical safety and outcome assessment. World J Surg 44(2):612–616. https://doi.org/10.1007/s00268-019-05212-7
Kiranantawat K, Sitpahul N, Taeprasartsit P, Constantinides J, Kruavit A, Srimuninnimit V et al (2014) The first smartphone application for microsurgery monitoring: silparamanitor. Plast Reconstr Surg 134(1):130–139
Zhang JE, Wong FKY, You LM, Zheng MC, Li Q, Zhang BY et al (2013) Effects of enterostomal nurse telephone follow-up on postoperative adjustment of discharged colostomy patients. Cancer Nurs 36(6):419–428
Santana RF, Pereira SK, Carmo TG, Freire V, Soares TDS, Amaral DM et al (2018) Effectiveness of a telephone follow-up nursing intervention in postsurgical patients. Int J Nurs Pract 24(4):e12648
Da Silva SR, Santana RF, Dos Santos CTB, Faleiro TB, Do Amaral Passarelles DM, Hercules ABS et al (2020) Telephonic nursing intervention for laparoscopic cholecystectomy and hernia repair: a randomized controlled study. BMC Nurs. https://doi.org/10.1186/s12912-020-00432-y
Gong S, Shen WW (2011) Telephone follow-up improves quality of life of postoperative patients with severe acute pancreatitis. J Sichuan Univ 42(5):712–715
Demir B, Binnetoglu A, Kersin B, Mammadova U, Kucuk N (2019) Could digital photography be an alternative to postoperative physical examination for pediatric tonsillectomy patients? Int J Pediatr Otorhinolaryngol 123:66–68
Zhang Y, Zhang P, Tian X, Chen G, Li Y, Zhang Y et al (2019) Remotely programmed sacral neuromodulation for the treatment of patients with refractory overactive bladder: a prospective randomized controlled trial evaluating the safety and efficacy of a novel sacral neuromodulation device. World J Urol 37(11):2481–2492
Padmanaban V, Johnston PF, Gyakobo M, Benneh A, Esinam A, Sifri ZC (2020) Long-term follow-up of humanitarian surgeries: outcomes and patient satisfaction in rural Ghana. J Surg Res 246:106–112
Yu L, Zhu Y, Chen W, Bu H, Zhang Y (2020) Incidence and risk factors associated with postoperative stroke in the elderly patients undergoing hip fracture surgery. J Orthop Surg Res 15(1):429
Ashengo TA, Grund J, Mhlanga M, Hlophe T, Mirira M, Bock N et al (2014) Feasibility and validity of telephone triage for adverse events during a voluntary medical male circumcision campaign in Swaziland. BMC Public Health 14(1):1–9
Dresser C, Periyanayagam U, Dreifuss B, Wangoda R, Luyimbaazi J, Bisanzo M (2017) Management and outcomes of acute surgical patients at a district hospital in Uganda with non-physician emergency clinicians. World J Surg 41(9):2193–2199. https://doi.org/10.1177/1054773817729074
Atasayar S, Demir SG (2019) Determination of the problems experienced by patients post-thyroidectomy. Clin Nurs Res 28(5):615–635
Tasa D, Eslami P, Dashti H, Toosi MN, Zarghami SY, Jafarian A (2020) The successful management of thirty-six hepatopancreatobiliary surgeries under the intensive protective arrangements during the COVID-19 pandemic. Acta Biomed 91(3):1–6
Carrillo GM, Mesa ML, Burbano DV (2021) Skills required in the care of cancer patients who undergo surgery in the hospital-home transition. J Cancer Educ. https://doi.org/10.1007/s13187-021-01964-w
Meltzer ME, Congdon N, Kymes SM, Yan X, Lansingh VC, Sisay A et al (2017) Cost and expected visual effect of interventions to improve follow-up after cataract surgery prospective review of early cataract outcomes and grading (precog) study. JAMA Ophthalmol 135(2):85–94
Zhang QL, Xu N, Huang ST, Chen Q, Cao H (2020) Effect of using the WeChat platform on the perioperative health education of parents of children who underwent transthoracic device closure of VSDs. J Cardiothorac Surg. https://doi.org/10.1186/s13019-020-01282-0
Zhang JE, Wong FK, You LM, Zheng MC (2012) A qualitative study exploring the nurse telephone follow-up of patients returning home with a colostomy. J Clin Nurs 21(9–10):1407–1415
Zheng Q, Yang L, Zeng B, Li J, Guo K, Liang Y et al (2021) Artificial intelligence performance in detecting tumor metastasis from medical radiology imaging: a systematic review and meta-analysis. EClinicalMedicine 31:100669
Chen J, Wang X, Qian H, Ye J, Qian J, Hua J (2020) Correlation between common postoperative complications of prolonged bed rest and quality of life in hospitalized elderly hip fracture patients. Ann Cardiothorac Surg 9(3):1125–1133
Lima JLDDA, De Aguiar RALP, Leite HV, Silva HHRM, De Oliveira WM, Sacramento JPTDC et al (2016) Surveillance of surgical site infection after cesarean section and time of notification. Am J Infect Control 44(3):273–277
Dogan SN, Salt V, Korkmazer B, Arslan S, Islak C, Kocer N et al (2020) Intrathecal use of gadobutrol for gadolinium-enhanced MR cisternography in the evaluation of patients with otorhinorrhea. Neuroradiology 62(11):1381–1387
Giorgis AT, Alemu AM, Arora S, Gessesse GW, Melka F, Woldeyes A et al (2019) Results from the first teleglaucoma pilot project in addis ababa. Ethiopia J Glaucoma 28(8):701–707
Akkoyun I (2012) The advantages of using photographs and video images in telephone consultations with a specialist in paediatric surgery. Afr J Paediatr Surg 9(2):128–131
den Hollander D, Mars M (2017) Smart phones make smart referrals: the use of mobile phone technology in burn care - a retrospective case series. Burns 43(1):190–194
Koparal M, Ünsal HY, Alan H, Üçkardeş F, Gülsün B (2019) WhatsApp messaging improves communication in an oral and maxillofacial surgery team. Int J Med Inform 132:103987
Gulacti U, Lok U, Hatipoglu S, Polat H (2016) An analysis of whatsapp usage for communication between consulting and emergency physicians. J Med Syst 40(6):1–7
Morkel RW, Mann TN, du Preez G, du Toit J (2019) Orthopaedic referrals using a smartphone app: uptake, response times and outcome. SAMJ S Afr Med J 109:859–864
Rockwell WT, Agbenorku P, Olson J, Hoyte-Williams PE, Agarwal JP, Rockwell WB (2015) A model for university-based international plastic surgery collaboration builds local sustainability. Ann Plast Surg 74(4):388–391
Wallis LA, Fleming J, Hasselberg M, Laflamme L, Lundin J (2016) A Smartphone app and cloud-based consultation system for burn injury emergency care. PLoS ONE 11(2):e0147253
Bertani A, Launay F, Candoni P, Mathieu L, Rongieras F, Chauvin F (2012) Teleconsultation in paediatric orthopaedics in Djibouti: evaluation of response performance. Orthop Traumatol Surg Res 98(7):803–807
Hasselberg M, Wallis L, Blessing P, Laflamme L (2017) A smartphone-based consultation system for acute burns - methodological challenges related to follow-up of the system. Glob Health Action 10(sup3):1328168
Fuzaylov G, Anderson R, Knittel J, Driscoll DN (2015) Global health: burn outreach program. J Burn Care Res 36(2):306–309
Martinez R, Rogers AD, Numanoglu A, Rode H (2018) The value of whatsapp communication in paediatric burn care. Burns 44(4):947–955
Kauta NJ, Groenewald J, Arnolds D, Blankson B, Omar A, Naidu P et al (2020) WhatsApp mobile health platform to support fracture management by non-specialists in South Africa. J Am Coll Surg 230(1):37–42
Shinn JR, Zuniga MG, Macharia I, Reppart J, Netterville JL, Jayawardena ADL (2019) Community health workers obtain similar results using cell-phone based hearing screening tools compared to otolaryngologists in low resourced settings. Int J Pediatr Otorhinolaryngol 127:109670
Fonseca ASF, Goldenberg DC, Stocchero GF, Costa Luiz AV, Gemperli R (2016) Validation of videoconference with smartphones in telemedicine facial trauma care: analysis of concordance to on-site evaluation. Ann Plast Surg 77(4):433–437
Olldashi F, Latifi R, Parsikia A, Boci A, Qesteri O, Dasho E et al (2019) Telemedicine for neurotrauma prevents unnecessary transfers: an update from a nationwide program in Albania and analysis of 590 patients. World Neurosurg 128:e340–e346
McCullough MC, Kulber L, Sammons P, Santos P, Kulber DA (2018) Google glass for remote surgical tele-proctoring in low- and middle-income countries: a feasibility study from Mozambique. Plast Reconstr Surg Glob Open 6(12):e1999
Datta N, Macqueen IT, Schroeder AD, Wilson JJ, Espinoza JC, Wagner JP et al (2015) Wearable technology for global surgical teleproctoring. J Surg Educ 72(6):1290–1295
Goldstein SD, Papandria D, Linden A, Azzie G, Borgstein E, Calland JF et al (2014) A pilot comparison of standardized online surgical curricula for use in low- and middle-income countries. JAMA Surg 149(4):341–346
Nagengast ES, Ramos MS, Sarma H, Deshpande G, Hatcher K, Magee WP Jr et al (2014) Surgical education through video broadcasting. J Craniofac Surg 25(5):1619–1621
Thapa A, Kc B, Shakya B (2016) Cost effective use of free-to-use apps in neurosurgery (FAN) in developing countries: from clinical decision making to educational courses strengthening health care delivery. World Neurosurg 95:270–275
Voelker HU, Poetzl L, Strehl A, Mueller-Hermelink HK, Stuefe A, Stauch G (2020) Telepathological evaluation of paediatric histological specimens in support of a hospital in Tanzania. Afr Health Sci 20(3):1313–1321
Sanguansak T, Morley KE, Morley MG, Thinkhamrop K, Thuanman J, Agarwal I (2017) Two-way social media messaging in postoperative cataract surgical patients: prospective interventional study. J Med Internet Res 19(12):e413
Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K et al (2014) Effect of text messaging to deter early resumption of sexual activity after male circumcision for HIV prevention: a randomized controlled trial. J Acquir Immune Defic Syndr 65(2):e50–e57
Abaza H, Marschollek M (2017) mHealth application areas and technology combinations. Method Inf Med 56(S 01):e105–e122
The wall street journal (2019) China emerges as global tech, innovation leader. [cited 2021 16 September], Available from: https://deloitte.wsj.com/articles/china-emerges-as-global-tech-innovation-leader-01572483727
Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T (2019) Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare 25(8):451–459
Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL et al (2014) A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare 20(8):427–430
Hakim AA, Kellish AS, Atabek U, Spitz FR, Hong YK (2020) Implications for the use of telehealth in surgical patients during the COVID-19 pandemic. Am J Surg 220(1):48–49
Akoko L, Mwanga A, Chikawe M, Lutainulwa E, Ngoma D, Nshalla A et al (2019) Supervision and support in surgical practice using mobile platform: a case of mass hydrocele surgeries in remote regions. Mhealth 5:41
Baatjes KJ, Keiller AV, Louw AJ, Van Rooyen M (2020) Point-of-view technology to teach surgery. Clin Teach 18(2):147–151
Nyamtema A, Mwakatundu N, Dominico S, Mohamed H, Shayo A, Rumanyika R et al (2016) Increasing the availability and quality of caesarean section in Tanzania. BJOG 123(10):1676–1682
Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K et al (2012) Text messaging to improve attendance at post-operative clinic visits after adult male circumcision for HIV prevention: a randomized controlled trial. PLoS ONE 7(9):e43832
Chaves RO, De Oliveira PAV, Rocha LC, David JPF, Ferreira SC, Santos ADASD et al (2017) An innovative streaming video system with a point-of-view head camera transmission of surgeries to smartphones and tablets: an educational utility. Surg Innov 24(5):462–470
da Mata LRF, Azevedo C, Bernardes MFVG, Chianca TCM, Pereira MG, de Carvalho EC (2019) Effectiveness of a home care teaching program for prostatectomized patients: a randomized controlled clinical trial. Revista da Escola de Enfermagem 53:e03421
Mattos SD, Hazin SMV, Regis CT, de Araujo JSS, Albuquerque FCD, Moser L et al (2015) A telemedicine network for remote paediatric cardiology services in north-east Brazil. Bull World Health Organ 93(12):881–887
Favaro ML, Gabor S, Souza DBF, Araújo AA, Milani ALC, Ribeiro Junior MAF (2020) Quadratus lumborum block as a single anesthetic method for laparoscopic totally extraperitoneal (Tep) inguinal hernia repair: a randomized clinical trial. Sci Rep. https://doi.org/10.1038/s41598-020-65604-x
Justicz N, Dusseldorp JR, Fuller JC, Leandre M, Jean-Gilles PM, Kim J et al (2019) Using mobile text and media to complement teaching in a facial reconstruction training module in Haiti. J Surg Educ 76(3):762–770
Lopez-Magallon AJ, Saenz L, Gutierrez JL, Florez CX, Althouse AD, Sharma MS et al (2018) Telemedicine in pediatric critical care: a retrospective study in an international extracorporeal membrane oxygenation program. Telemed e-Health 24(7):489–496
Nieto-Calvache AJ, López-Girón MC, Messa-Bryon A, Ceballos-Posada ML, Duque-Galán M, Ríos-Posada JGD et al (2019) Urinary tract injuries during treatment of patients with morbidly adherent placenta. J Matern Fet Neonatal Med 34:3140–3146
Sousa CS, Turrini RNT (2019) Development of an educational mobile application for patients submitted to orthognathic surgery. Rev Lat Am Enfermagem. https://doi.org/10.1590/1518-8345.2904.3143
Bikmoradi A, Masmouei B, Ghomeisi M, Roshanaei G (2016) Impact of tele-nursing on adherence to treatment plan in discharged patients after coronary artery bypass graft surgery: a quasi-experimental study in Iran. Int J Med Inf 86:43–48
Murad MF, Ali Q, Nawaz T, Zia N, Jehan F, Rafiq A et al (2014) Teleoncology: improving patient outcome through coordinated care. Telemed e-Health 20(4):381–384
Aydogdu O, Sen V, Yarimoglu S, Aydogdu C, Bozkurt IH, Yonguc T (2019) The effect of additional telerounding on postoperative outcomes, patient and surgeon satisfaction rates in the patients who underwent percutaneous nephrolithotomy. Arch Esp Urol 72(1):69–74
Erdogan Z, Bulut H (2020) Effectiveness of computer assisted training of patients undergoing lumbar disc herniation surgery. Turk Neurosurg 30(1):69–77
Özalp Gerçeker G, Karayağız Muslu G, Yardimci F (2016) Children’s postoperative symptoms at home through nurse-led telephone counseling and its effects on parents’ anxiety: a randomized controlled trial. J Spec Pediatr Nurs 21(4):189–199
Gülşen M, Akansel N (2020) Effects of discharge education and telephone follow-up on cataract patients’ activities according to the model of living. J Perianesth Nurs 35(1):67–74
Güven B, Akyolcu N (2020) Effects of nurse-led education on quality of life and weight loss in patients undergoing bariatric surgery. Bariatr Surg Pract Patient Care 15(2):81–87
Korkmaz S, Iyigun E, Tastan S (2020) An evaluation of the influence of web-based patient education on the anxiety and life quality of patients who have undergone mammaplasty: a randomized controlled study. J Cancer Educ 35(5):912–922
Nemli A, Tekinsoy KP (2019) Effects of exercise training and follow-up calls at home on physical activity and quality of life after a mastectomy. Jpn J Nurs Sci 16(3):322–328
Kizilcik Özkan Z, Ünver S, Yildiz Findik Ü, Albayrak D, Fidan Ş (2020) Effect of short message service use on bowel preparation quality in patients undergoing colonoscopy. Gastroenterol Nurs 43(1):89–95
Sayin Y, Kanan N (2010) Reasons for nursing telephone counseling from individuals discharged in the early postoperative period after breast surgery. Nurs Forum 45(2):87–96
Turk E, Karagulle E, Aydogan C, Oguz H, Tarim A, Karakayali H et al (2011) Use of telemedicine and telephone consultation in decision-making and follow-up of burn patients: initial experience from two burn units. Burns 37(3):415–419
Yanov Y, Kuzovkov V, Sugarova S, Levin S, Lilenko A, Kliachko D (2018) Successful application and timing of a remote network for intraoperative objective measurements during cochlear implantation surgery. Int J Audiol 57(9):688–694
Agrawal R, Mishra SK, Mishra A, Chand G, Agarwal G, Agarwal A et al (2014) Role of telemedicine technology in endocrine surgery knowledge sharing. Telemed e-Health 20(9):868–874
Balachandran R, Kappanayil M, Sen AC, Sudhakar A, Nair SG, Sunil GS et al (2015) Impact of the international quality improvement collaborative on outcomes after congenital heart surgery: a single center experience in a developing economy. Ann Card Anaesth 18(1):52–57
Bansal M, Singh S, Maheshwari P, Adams D, McCulloch ML, Dada T et al (2015) Value of interactive scanning for improving the outcome of new-learners in transcontinental tele-echocardiography (VISION-in-Tele-Echo) study. J Am Soc Echocardiogr 28(1):75–87
Chandrasinghe PC, Siriwardana RC, Kumarage SK, Munasinghe BNL, Weerasuriya A, Tillakaratne S et al (2020) A novel structure for online surgical undergraduate teaching during the COVID-19 pandemic. BMC Med Educ 20(1):1–7
Dadlani R, Mani S, Au JG, Mohan D, Rajgopalan N, Thakar S et al (2014) The impact of telemedicine in the postoperative care of the neurosurgery patient in an outpatient clinic: a unique perspective of this valuable resource in the developing world - an experience of more than 3000 teleconsultations. World Neurosurg 82(3):270–283
Joshi SS, Murali-Krishnan S, Patankar P, Choudhari KA (2018) Neurosurgical referral service using smartphone client whatsapp: preliminary study at a tertiary referral neurosurgical unit. Br J Neurosurg 32(5):553–557
Khanna V, Sambandam SN, Gul A, Mounasamy V (2015) “Whatsapp”ening in orthopedic care: a concise report from a 300-bedded tertiary care teaching center. Eur J Orthop Surg Traumatol 25(5):821–826
Mayadevi M, Thankappan K, Limbachiya SV, Vidhyadharan S, Villegas B, Ouyoung M et al (2018) Interdisciplinary telemedicine in the management of dysphagia in head and neck. Dysphagia 33(4):474–480
Srivastava V, Pandey V, Tiwari P, Patel S, Ansari MA, Shukla VK (2020) Utility of real-time online teaching during covid era among surgery postgraduates. Indian J Surg 82(5):762–768
Sultania M, Muduly DK, Balasubiramaniyan V, Imaduddin M, Ephraim R, Chaudhary I et al (2020) Impact of the initial phase of COVID-19 pandemic on surgical oncology services at a tertiary care center in eastern India. J Surg Oncol 122(5):839–843
Suryaningtyas W, Wahyuhadi J, Turchan A, Subagio EA, Parenrengi MA, Apriawan T et al (2020) Neurosurgery at the epicenter of the COVID-19 pandemic in Indonesia: experience from a surabaya academic tertiary hospital. Neurosurg Focus 49(6):1–8
Uddin MN, Islam FMA (2020) Psychometric evaluation of the modified Kessler seven-item version (K7) for measuring psychological distress using Rasch analysis: a cross-sectional study in a rural district of Bangladesh. BMJ Open 10(2):e034523
Uemura M, Kenmotsu H, Tomikawa M, Kumashiro R, Yamashita M, Ikeda T et al (2015) Novel, high-definition 3-D endoscopy system with real-time compression communication system to aid diagnoses and treatment between hospitals in Thailand. Asian J Endosc Surg 8(2):139–147
Wantanakorn P, Harintajinda S, Chuthapisith J, Anurathapan U, Rattanatamrong P (2018) A new mobile application to reduce anxiety in pediatric patients before bone marrow aspiration procedures. Hosp Pediatr 8(10):643–650
Cheng C, Ho RTH, Guo Y, Zhu M, Yang W, Li Y et al (2020) Development and feasibility of a mobile health-supported comprehensive intervention model (CIMmH) for improving the quality of life of patients with esophageal cancer after esophagectomy: prospective, single-arm, nonrandomized pilot study. J Med Internet Res 22(8):e18946
Davis MC, Can DD, Pindrik J, Rocque BG, Johnston JM (2016) Virtual interactive presence in global surgical education: international collaboration through augmented reality. World Neurosurg 86:103–111
Dong X, Yi X, Gao D, Gao Z, Huang S, Chao M et al (2019) The effects of the combined exercise intervention based on internet and social media software (CEIBISMS) on quality of life, muscle strength and cardiorespiratory capacity in Chinese postoperative breast cancer patients: a randomized controlled trial. Health Qual Life Outcomes 17(1):109
Dong X, Yi X, Ding M, Gao Z, McDonough DJ, Yi N et al (2020) A longitudinal study of a multicomponent exercise intervention with remote guidance among breast cancer patients. Int J Environ Res Public Health 17(10):3425
Dong X, Sun G, Zhan J, Liu F, Ma S, Li P et al (2019) Telephone-based reminiscence therapy for colorectal cancer patients undergoing postoperative chemotherapy complicated with depression: a three-arm randomised controlled trial. Support Care Cancer 27(8):2761–2769
Feng S, Liang Z, Zhang R, Liao W, Chen Y, Fan Y et al (2017) Effects of mobile phone WeChat services improve adherence to corticosteroid nasal spray treatment for chronic rhinosinusitis after functional endoscopic sinus surgery: a 3-month follow-up study. Eur Arch Otorhinolaryngol 274(3):1477–1485
Ferraris KP, Golidtum JP, Zuñiga BKW, Bautista MCG, Alcazaren JC, Seng K et al (2020) Recapitulating the bayesian framework for neurosurgical outpatient care and a costbenefit analysis of telemedicine for socioeconomically disadvantaged patients in the Philippines during the pandemic. Neurosurg Focus 49(6):1–9
Hou J, Yang R, Yang Y, Tang Y, Deng H, Chen Z et al (2019) The effectiveness and safety of utilizing mobile phone-based programs for rehabilitation after lumbar spinal surgery: multicenter, prospective randomized controlled trial. JMIR Mhealth Uhealth 7(2):e10201
Huang G, Crooms R, Chen Q, Congdon N, He M (2012) Compliance with follow-up after cataract surgery in rural China. Ophthalmic Epidemiol 19(2):67–73
Huang J, Luo Q, Tan Q, Lin H, Qian L, Lin X (2014) Initial experience of robot-assisted thoracoscopic surgery in China. Int J Med Robot Comput Assist Surg 10(4):404–409
Li HL, Chan YC, Huang JX, Cheng SW (2020) Pilot study using telemedicine video consultation for vascular patients’ care during the COVID-19 period. Ann Vasc Surg 68:76–82
Li M, Zhang M, Wang H, Pan X, Wu W, Zhang Q et al (2016) The efficacy of internet-based intervention on quality of life for patients with chronic post-surgical pain. Iran J Public Health 45(12):1604–1609
Lin H, Chen W, Luo L, Congdon N, Zhang X, Zhong X et al (2012) Effectiveness of a short message reminder in increasing compliance with pediatric cataract treatment: a randomized trial. Ophthalmology 119(12):2463–2470
Liu J, Zheng X, Chai S, Lei M, Feng Z, Zhang X et al (2018) Effects of using WeChat-assisted perioperative care instructions for parents of pediatric patients undergoing day surgery for herniorrhaphy. Patient Educ Couns 101(8):1433–1438
Liu J, Zheng X, Zhang X, Feng Z, Song M, Lopez V (2020) The evidence and future potential of WeChat in providing support for Chinese parents of pediatric patients undergoing herniorrhaphy. J Transcult Nurs 31(2):114–120
Qiu Y, Liu Y, Ren W, Qiu Y, Ren J (2018) Internet-based and mobile-based general practice: cross-sectional survey. J Med Internet Res 20(9):e266
Qiu Y, Zhang YF, Zhu LR, He JS, Tan JY, Tan ND et al (2020) Impact of COVID-19 on the healthcare of patients with inflammatory bowel disease: a comparison between epicenter vs non-epicenter areas. Front Med. https://doi.org/10.3389/fmed.2020.576891
Qu J, Du J, Rao C, Chen S, Gu D, Li J et al (2021) Effect of a smartphone-based intervention on secondary prevention medication prescriptions after coronary artery bypass graft surgery: the MISSION-1 randomized controlled trial. Am Heart J 237:79–89
Shen Y, Fang Y, Wu D, Bai J, Lin Y (2020) Application of WeChat-assisted peri-operative care in children with congenital megacolon. J Paediatr Child Health 56(10):1551–1556
Shen Z, Zheng F, Zhong Z, Ding S, Wang L (2019) Effect of peer support on health outcomes in patients with cardiac pacemaker implantation: a randomized, controlled trial. Nurs Health Sci 21(2):269–277
Wong IYH, Ni MY, Wong IOL, Fong N (2018) Leung GM 2018 saving sight in china and beyond: the lifeline express model. BMJ Glob Health 3(4):e000766
Xia L (2020) The effects of continuous care model of information-based hospital-family integration on colostomy patients: a randomized controlled trial. J Cancer Educ 35(2):301–311
Xin Y, Li X, Du J, Cheng J, Yi C, Mao H (2019) Efficacy of telephone follow-up in children tonsillectomy with day surgery. Indian J Pediatr 86(3):263–266
Xu L, Jonas JB, Cui TT, You QS, Wang YX, Yang H et al (2012) Beijing eye public health care project. Ophthalmology 119(6):1167–1174
Yang K, Jin L, Li L, Zeng S, Wei R, Li G et al (2016) Interventions to promote follow-up after trabeculectomy surgery in rural southern China: a randomized clinical trial. JAMA Ophthalmol 134(10):1135–1141
Ye J, Zuo Y, Xie T, Wu M, Ni P, Kang Y et al (2016) A telemedicine wound care model using 4G with smart phones or smart glasses: a pilot study. Medicine 95(31):e4198
Ye Y, Wang J, Xie Y, Jiang H, Zhong J, He X et al (2016) Global teleophthalmology with the smartphone for microscopic ocular surgery. Eye Contact Lens 42(5):275–279
Yu C, Liu C, Du J, Liu H, Zhang H, Zhao Y et al (2020) Smartphone-based application to improve medication adherence in patients after surgical coronary revascularization. Am Heart J 228:17–26
Zhang YF, Qiu Y, He JS, Tan JY, Li XZ, Zhu LR et al (2020) Impact of COVID-19 outbreak on the care of patients with inflammatory bowel disease: a comparison before and after the outbreak in South China. J Gastroenterol Hepatol 36:100–709
Zhou K, Li J, Li X (2019) Effects of cyclic adjustment training delivered via a mobile device on psychological resilience, depression, and anxiety in Chinese post-surgical breast cancer patients. Breast Cancer Res Treat 178(1):95–103
Zhou K, Wang W, Zhao W, Li L, Zhang M, Guo P et al (2020) Benefits of a WeChat-based multimodal nursing program on early rehabilitation in postoperative women with breast cancer: a clinical randomized controlled trial. Int J Nurs Stud 106:103565
Zou Q, Zhang G, Liu Y (2018) Health education using telephone and WeChat in treatment of symptomatic uterine myoma with high-intensity focused ultrasound. Med Sci Monit Basic Res 24:127–133
Lovecchio F, Riew GJ, Samartzis D, Louie PK, Germscheid N, An HS et al (2020) Provider confidence in the telemedicine spine evaluation: results from a global study. Eur Spine J 30:2109–2123
Marttos AC Jr, Moscardi MFJ, Fiorelli RKA, Pust GD, Ginzburg E, Schulman CI et al (2018) Use of telemedicine in surgical education: a seven-year experience. Am Surg 84(8):1252–1260
Sciarra AMP, Croti UA, Batigalia F (2014) Information technology implementing globalization on strategies for quality care provided to children submitted to cardiac surgery: international quality improvement collaborative program-IQIC. Braz J Cardiovasc Surg 29:89–92
Funding
None.
Author information
Authors and Affiliations
Contributions
EOO and KMC conceptualized the study. EOO, KC and JID developed the methodology. EOO, TM and JL screened and extracted the studies. EOO analysed the data and made the first draft. KC, JID, TM and JL revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
The study made use of publicly available data; therefore, ethics approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Search strategy
PubMed
#1 | Telemedicine [MeSH Term] |
#2 | Title, Abstract and Keyword: ehealth OR electronic health OR telehealth OR mobile health OR mhealth OR telephone follow-up OR telecare OR telesurgery OR tele assistance OR telepresence OR remote consultation OR teleconsultation OR remote patient monitoring OR tele rehabilitation OR digital health |
#3 | #1 OR #2 |
#4 | General surgery [MeSH Term] |
#5 | Title, Abstract and Keyword: surgery OR intraoperative OR preoperative OR postoperative OR surgical procedures |
#6 | #4 OR #5 |
#7 | Developing countries [MeSH Terms] |
#8 | Title Abstract Keyword: Afghanistan OR Guinea-Bissau OR Sierra Leone OR Burkina Faso OR Haiti OR Somalia OR Burundi OR Democratic People’s Republic of Korea OR South Sudan OR Central African Republic OR Liberia OR Sudan OR Chad OR Madagascar OR Syrian Arab Republic OR Democratic Republic of Congo OR Malawi OR Tajikistan OR Eritrea OR Mali OR Togo OR Ethiopia OR Mozambique OR Uganda OR The Gambia OR Niger OR Republic of Yemen OR Guinea OR Rwanda OR Angola OR Honduras OR Papua New Guinea OR Algeria OR India OR Philippines OR Bangladesh OR Kenya OR São Tomé and Principe OR Benin OR Kiribati OR Senegal OR Bhutan OR Kyrgyz Republic OR Solomon Islands OR Bolivia OR Lao PDR OR Sri Lanka OR Cabo Verde OR Lesotho OR Tanzania OR Cambodia OR Mauritania OR Timor-Leste OR Cameroon OR Federated States of Micronesia OR Tunisia OR Comoros OR Moldova OR Ukraine OR Republic of Congo OR Mongolia OR Uzbekistan OR Côte d’Ivoire OR Morocco OR Vanuatu OR Djibouti OR Myanmar OR Vietnam OR Arab Republic of Egypt OR Nepal OR West Bank and Gaza OR El Salvador OR Nicaragua OR Zambia OR Eswatini OR Nigeria OR Zimbabwe OR Ghana OR Pakistan OR Albania OR Fiji OR Montenegro OR American Samoa OR Gabon OR Namibia OR Argentina OR Georgia OR North Macedonia OR Armenia OR Grenada OR Paraguay OR Azerbaijan OR Guatemala OR Peru OR Belarus OR Guyana OR Russian Federation OR Belize OR Indonesia OR Samoa OR Bosnia and Herzegovina OR Islamic Republic of Iran OR Serbia OR Botswana OR Iraq OR South Africa OR Brazil OR Jamaica OR St. Lucia OR Bulgaria OR Jordan OR St. Vincent and the Grenadines OR China OR Kazakhstan OR Suriname OR Colombia OR Kosovo OR Thailand OR Costa Rica OR Lebanon OR Tonga OR Cuba OR Libya OR Turkey OR Dominica OR Malaysia OR Turkmenistan OR Dominican Republic OR Maldives OR Tuvalu OR Equatorial Guinea OR Marshall Islands OR Venezuela OR RB Ecuador OR Mexico |
#9 | #7 OR #8 |
#10 | #3 AND #6 AND #9 |
Limit to 2010–2021 |
Cochrane library: Similar search strategy used for PubMed was used on this database.
Scopus and web of science: These databases do not use Mesh Terms, keywords similar to those applied on PubMed were applied on these databases as shown below:
#1 | (telemedicine OR ehealth OR “electronic health” OR telehealth OR “mobile health” OR mhealth OR “telephone follow-up” OR telecare OR telesurgery OR “tele assistance” OR telepresence OR “remote consultation” OR teleconsultation OR “remote patient monitoring” OR “tele rehabilitation” OR “digital health”) |
#2 | (“general surgery” OR preoperative OR intraoperative OR postoperative OR “surgical procedure”) |
#3 | (“developing countries” OR Afghanistan OR “Guinea-Bissau” OR “Sierra Leone” OR “Burkina Faso” OR Haiti OR Somalia OR Burundi OR Korea OR “Democratic people’s republic of south Sudan” OR “Central African Republic” OR Liberia OR Sudan OR Chad OR Madagascar OR “Syrian Arab Republic” OR “Democratic Republic of Congo” OR Malawi OR Tajikistan OR Eritrea OR Mali OR Togo OR Ethiopia OR Mozambique OR Uganda OR “The Gambia” OR Niger OR “Republic of Yemen” OR Guinea OR Rwanda OR Angola OR Honduras OR “Papua New Guinea” OR Algeria OR India OR Philippines OR Bangladesh OR Kenya OR “Sao tomé and principe” OR Benin OR Kiribati OR Senegal OR Bhutan OR “Kyrgyz Republic” OR “Solomon Islands” OR Bolivia OR “Lao PDR” OR “Sri Lanka” OR “Cabo Verde” OR Lesotho OR Tanzania OR Cambodia OR Mauritania OR “Timor-leste” OR Cameroon OR “Federated states of micronesia” OR Tunisia OR Comoros OR Moldova OR Ukraine OR “Republic of Congo” OR Mongolia OR Uzbekistan OR “Cote d’ivoire” OR Morocco OR Vanuatu OR Djibouti OR Myanmar OR Vietnam OR “Arab republic of Egypt” OR Nepal OR “West bank and Gaza” OR “El Salvador” OR Nicaragua OR Zambia OR Eswatini OR Nigeria OR Zimbabwe OR Ghana OR Pakistan OR Albania OR Fiji OR Montenegro OR “American Samoa” OR Gabon OR Namibia OR Argentina OR Georgia OR “North Macedonia” OR Armenia OR Grenada OR Paraguay OR Azerbaijan OR Guatemala OR Peru OR Belarus OR Guyana OR “Russian Federation” OR Belize OR Indonesia OR Samoa OR “Bosnia and Herzegovina” OR “Islamic republic of Iran” OR Serbia OR Botswana OR Iraq OR “South Africa” OR Brazil OR Jamaica OR “St. Lucia” OR Bulgaria OR Jordan OR “St. Vincent and the Grenadines” OR China OR Kazakhstan OR Suriname OR Colombia OR Kosovo OR Thailand OR “Costa Rica” OR Lebanon OR Tonga OR Cuba OR Libya OR Turkey OR Dominica OR Malaysia OR Turkmenistan OR “Dominican Republic” OR Maldives OR Tuvalu OR “Equatorial Guinea” OR “Marshall Islands” OR Venezuela OR “Rb Ecuador” OR Mexico) |
#4 | #1 AND #2 AND #3 |
African journal online (AJOL)
Keywords used for Scopus database were applied on AJOL to extract relevant studies.
Rights and permissions
About this article
Cite this article
Owolabi, E.O., Mac Quene, T., Louw, J. et al. Telemedicine in Surgical Care in Low- and Middle-Income Countries: A Scoping Review. World J Surg 46, 1855–1869 (2022). https://doi.org/10.1007/s00268-022-06549-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06549-2