Abstract
Background
Hepatic epithelioid hemangioendothelioma (HEH) is a rare tumor that can affect multiple organs. Little is known about the pathophysiology, clinical course and management of this disease. The aim of this study is to determine survival rates and elucidate the role of various prognostic factors and therapeutic modalities as compared to surgery on patients with HEH.
Methods
A retrospective analysis on patients diagnosed with HEH between 2004 and 2016 was performed utilizing the SEER database. Kaplan–Meier curves were constructed to determine overall and cancer-specific survival, and the log-rank test was used to compare between groups. To explore prognostic factors and treatment outcomes, univariable and multivariable Cox proportional hazard models were developed.
Results
A total of 353 patients with HEH (median age: 50.4 years) were identified. The most common surgery performed was liver resection (90.8%). One-year OS in the surgical group and non-surgical group was 86.6% and 61.0%, respectively, while 5-year OS was 75.2% and 37.4%, respectively. On multivariable analysis, surgery emerged as a favorable prognostic factor [HR (95%CI): 0.404 (0.215–0.758) p value = 0.005]. Age > 65 years [HR (95%CI): 2.548 (1.442–4.506) p value = 0.001] and tumor size > 10 cm [HR (95%CI): 2.401 (1.319–4.37) p value = 0.004] were shown to be poor survival prognostic factors.
Conclusion
HEH is a rare disease that is poorly understood. Surgical intervention is associated with improved survival rates. Multicenter prospective collaborations are needed to improve our limited knowledge about this neoplasm and determine the optimal treatment strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epithelioid hemangioendothelioma is a rare tumor that can affect multiple organs [1]. It was first described by Weiss and Enzinger in 1982 as a rare vascular tumor that was often mistaken for metastatic carcinoma [2]. These neoplasms most commonly arise in the liver, lungs and bones [3]. Of these, the liver is the most commonly involved organ and the incidence rate of hepatic epithelial hemangioendothelioma (HEH) is as low as 1 per 1 000 000 [1, 4].
HEH is a low-grade neoplasm with pathology ranging between benign hemangioma and aggressive angiosarcoma [5]. While some patients are asymptomatic, others report right upper quadrant pain, weight loss, jaundice as well as general gastrointestinal symptoms such as nausea and anorexia. These neoplasms have been associated with multiple diseases including: Kasabach–Merritt syndrome and Budd–Chiari syndrome, although their association still remains rare [6]. Little is known about the pathophysiology, clinical course and management of this disease because of its low incidence rate. Although different treatment modalities have been utilized, a consensus for the single best has not been established yet [7]. Treatment options include medical therapy with propranolol and prednisone, chemo/immunotherapy with different suggested regimens, radiotherapy and radiofrequency ablation, as well as different surgical interventions including liver resection and liver transplantation [8,9,10].
Due to relatively low number of cases, studies investigating therapeutic outcomes are conflicting and limited. Chemotherapy has been associated with remission induction in some studies, while it has also been associated with disease progression in others [10,11,12]. Similarly, surgical resection has been associated with promising results often leading to partial or even complete response [13]. The ELTR study, the largest case series on the surgical management of HEH, has also shown a significant value for liver transplantation [14]. However, other studies have shown no significant difference in survival between patients undergoing surgery and those treated medically [13, 15].
Accordingly, the literature on the management of HEH is mostly comprised of case reports and small case series. The principle goal of this study is to determine survival rates and elucidate the role of various prognostic factors and therapeutic modalities as compared to surgical approach on patients with HEH leveraging the large US population-based Surveillance, Epidemiology, and End Results (SEER) Program database.
Materials and methods
Data retrieval
The SEER registry is a well-established and reliable database for cancer research. The registry includes data from 17 regions in the USA, involving around 28% of the entire US population. The information collected and added to the SEER registry contains patient demographics, primary cancer site, grade/stage of disease, utilization of surgical procedures or radiation therapy and follow-up on vital status [16]. Data also include whether death was due to the cancer or due to another cause, allowing to calculate cancer-specific survival (CSS) and overall survival (OS), respectively. All data concerning HEH were retrieved from the SEER registry between 2004 and 2016. Patients from earlier years (1973–2003) were excluded due to missing variables and in order to reflect more contemporary trends in the survival of HEH patients.
The International Classification of Disease (ICD) and 3rd edition histology codes (9130 for hemangioendothelioma and 9133 for epithelioid hemangioendothelioma) were combined with the code C22.0 (for liver) to retrieve the data from patients with HEH. Patient baseline characteristics included age, gender and race. Tumors were divided by size into ≤ 10 or > 10 cm. Tumor stage was defined as localized (confined to the liver), regional (either direct extension or regional lymph nodes) or distant (metastatic to distant lymph nodes or distant organs). Treatment modalities included chemotherapy, radiotherapy and surgery. The SEER database does not provide details on the chemotherapy administered. Surgical treatment included wedge/segment resection (codes 20–29), lobectomy (codes 30–59), liver transplantation (codes 60–89) or surgery not otherwise specified (code 90).
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) (version 24.0, IBM Corp., Armonk N.Y., USA). Continuous data were reported as means and standard deviations (SD) with comparisons made using the independent t test. Categorical data were reported as counts and proportions, with comparisons made using the Chi-square test, or the Fisher's exact test, as appropriate. Kaplan–Meier curves were constructed to determine OS and CSS, and the log-rank test was used to compare between groups. To explore prognostic factors, univariable and multivariable Cox proportional hazard models were developed. Variables significant on univariable analysis were included in the multivariable model. Risk-adjusted hazard ratios (HRs) with corresponding 95% confidence intervals (95% CI) were calculated. A two-sided p value < 0.05 was used to indicate statistical significance.
Results
Study population
A total of 353 patients with HEH were identified (Table 1). The mean age of all patients was 50.4 ± 18.8 years with 42.4% aged between 40 and 60 years. The mean age of patients undergoing surgery was significantly lower (48.3 vs 52.7, p value = 0.03) with around half of patients in the 40- to 60-year age category. Most patients were female (n = 196, 55.5%) and white (n = 280, 79.0%), and there was no difference in gender or ethnic distribution between the two groups. Patients in the surgery group mostly comprised of localized (n = 89, 48.1%) and regional (n = 55, 29.7%) malignancy, while those not receiving surgery most often had distant (n = 81, 48.2%) or unstaged (n = 40, 23.8%) malignancy. Similarly, most patients (n = 112, 60.5%) had tumor size ≤ 10 cm in the surgery group, while 69.0% (n = 115) of patients were had tumor size > 10 cm in the non-surgical group. The overall median follow-up time for all patients was 29 months (IQR: 6–80).
Treatment modalities
Chemotherapy was administered to 84.9% (n = 157) of patients undergoing surgery, compared to 56.5% (n = 95) of those who were not. Radiotherapy was used in treating 25.7% (n = 47) of the patients in the surgical group, while it was only used in treating one patient (0.6%) in the non-surgical group. The most common surgery performed was wedge/segment resection (n = 86, 47.0%), followed by major liver resection (n = 82, 44.8%) and transplant (n = 15, 8.2%). Table 2 presents the different combinations in treatment modalities in patients undergoing surgery. Radiotherapy was administered to 22 patients (25.6%) undergoing wedge/segment resection, 23 patients (12.6%) undergoing major liver resection and 2 patients (13.3%) undergoing transplant.
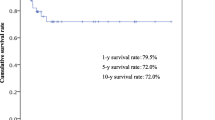
Survival
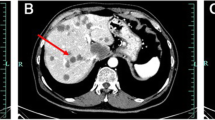
In the overall study population, the OS rates at 1 and 5 years were 74.6% and 57.6%, respectively, while CSS rates were 80.1% and 66.8%, respectively. OS and CSS between the surgical and non-surgical groups were statistically different (p value < 0.001). One-year OS in the surgical group and non-surgical group was 86.6% and 61%, respectively, while 5-year OS was 75.2% and 37.4%, respectively (Fig. 1). One-year CSS in the surgical group and non-surgical group was 90.8% and 67.6%, respectively, while 5-year CSS was 83.7% and 46.2%, respectively.
On subgroup analysis, patients with localized and regional disease had significantly higher overall survival when undergoing surgery (Figs. 2, 3). Overall survival was not different between the surgical and non-surgical groups in patients with distant metastasis (Fig. 4). Table 3 displays the 1- and 5-year OS for each disease stage.
Prognostics factors
Using univariable analysis, surgery was associated more favorable outcomes [HR (95%CI): 0.339 (0.241–0.478), p-value < 0.001]. Distant malignancy as compared to localized [HR (95%CI): 3.46 (2.248–5.324), p value < 0.001], tumor size > 10 cm [HR (95%CI): 2.664 (1.531–4.636), p value = 0.001] and chemotherapy [HR (95%CI): 2.083 (1.489–2.916), p value < 0.001] were shown to be poor survival prognostic factors (Table 4).
On multivariate analysis, surgery retained its significance as a favorable prognostic factor [HR (95%CI): 0.404 (0.215–0.758), p value = 0.005], while age > 65 years [HR (95%CI): 2.548 (1.442–4.506), p value = 0.001] and tumor size > 10 cm [HR (95%CI): 2.401 (1.319–4.37), p value = 0.004] retained their significance as poor prognostic factors (Table 5). On subgroup analysis, chemotherapy [HR (95%CI): 3.51 (1.023–12.042), p value = 0.046] was also shown to be a poor survival prognostic factor in patients with localized disease in the multivariable regression model (Table 6).
Discussion
Hepatic endothelial hemangioendothelioma remains one of the less understood neoplasms of the liver with limited consensus regarding its management. In this study, the national scale SEER database was employed to elucidate the prognosis of patients with this malignancy as well as the factors associated with survival outcomes. Specifically, we investigated the role of surgery in the treatment of this neoplasm.
Various case reports and series have suggested different clinical outcomes in HEH, from spontaneous complete regression (reported once in the literature) to aggressive rapid progression and poor survival [17,18,19]. Reported survival rates vary between studies due to dissimilarities in patient characteristics and differences in treatment strategies. As a low-grade neoplasm, prognosis of HEH is better than that of benign liver hemangioma but worse than the prognosis of malignant liver hemangiosarcoma [20, 21]. Table 7 summarizes survival outcomes based on the interventions performed in different reports [8, 13,14,15, 21,22,23,24,25,26,27,28].
Two SEER studies about HEH were previously published. In the first study with limited number of patients (n = 56), 1-year OS rate of HEH was 57% in patients undergoing surgical resection, 67% in patients not undergoing surgery and 80% for patients undergoing liver transplant [21]. In the more recent study, yet limited (n = 79), analysis of the SEER database, 1- and 5-year CSS was reported to be 74.1% and 57.8%, respectively, regardless of disease stage and treatment modality [29]. In this study, which includes only patients diagnosed after 2004, CSS rates were higher reaching 80.1% and 66.8% at 1 and 5 years, respectively. This reflects an improvement in the understanding and management of the disease and might be explained by both diagnosis at earlier stages and by the different treatment modalities adopted over time. In this cohort, 31.4% of patients had distant metastasis compared to 39.2% in the former cohort. Similarly, only 26.9% of patients had no treatment and 52.4% underwent surgery as compared to 39.2% with no treatment and 25.7% undergoing surgery in the previous study [29].
Data on prognostic factors predicting outcomes of HEH are conflicting. Previous studies have suggested multi-organ involvement, male gender, ascites and age above 55 years to be associated with worse prognoses, while suggesting chemotherapy and surgery to be associated with improved outcomes [22, 27, 30]. In this analysis, while considering the different patient characteristics and after risk adjustment, age > 65 years and tumor size > 10 cm were associated with worse prognosis, while surgical intervention was associated with better prognosis. Gender and tumor stage were not associated with difference in survival. In patients with localized tumor, chemotherapy was associated with poor survival outcomes, shedding light on the importance of patient selection before chemotherapy administration.
Surgical intervention is considered as one of the therapeutic options for HEH. Hepatic artery ligation, hepatic resection and liver transplantation have all been utilized [31]. Resection is mainly reserved for localized single lesions while transplantation for multiple bilobar disease [32]. In a retrospective review of 30 HEH patients treated at the Mayo Clinic, a similar pattern of surgical intervention selection was observed; patients with lower number of nodules and liver segments involvement underwent resection as compared to those with higher numbers who underwent transplantation [26]. Most patients undergoing surgery (82%) had no extrahepatic involvement at the time of surgery. However, Grotz et al. found that OS was not different between patients with and without extrahepatic involvement and argued that metastases may not be a contraindication for surgery [26]. This observation was also made in the ELTR study [14].
Survival analysis in this study is partially in agreement with the previous argument. OS rates were higher in patients undergoing surgery compared to no surgery both if the malignancy was localized or if it was regional. When metastasis was distant, OS was not different between the surgical and the non-surgical group. However, it is important to note that of the 30 patients with distant metastatic disease undergoing surgery, most patients underwent liver resection, while only three underwent liver transplantation.
The ELTR study, and in-depth study of 210 patients and the world’s largest transplantation series for patients with HEH, showed that distant extrahepatic disease was not a risk factor for worse survival outcomes. In this series, which included 40 patients with extrahepatic disease, liver transplantation resulted in a 5-year survival of 71.6% in this patient category, remarkably higher than the 39.6% survival in this study’s patient cohort undergoing surgery [14]. Our study further supports the algorithm proposed by the ELTR study, suggesting liver transplantation as the treatment modality in patients with unresectable tumor or contained extrahepatic disease.
However, the question that remains to be answered is whether to perform tumor resection or liver transplantation when regional but no extrahepatic disease is present. One- and 5-year survival rates of this patient category from the ELTR study were 91.5% and 84.2% after transplantation, higher than those reported from this study (86.8% and 76.8%, respectively). While this could be due to difference in patient characteristics, such difference cannot be established due to the limitations on variables in the SEER database. A prospective study comparing surgical strategies taking relevant patient characteristics is needed. Due to the low incidence of HEH, collaborations between different medical institutions and multicenter randomized controlled trials conducted over the different continents might be the only way to provide a confident answer to this question and establish an evidence-based treatment algorithm.
Novel treatment modalities are always emerging for rare diseases such as HEH. One novel technique in the management of this disease was presented by Lau et al. where they utilized a combination of capecitabine and bevacizumab in treating a patient with metastatic HEH. Their results showed significant regression in the tumor sizes and present a new approach for patients who are awaiting liver transplantation or are non-surgical candidates [7]. Along the same line, ongoing clinical trials are utilizing different chemo and immune therapy agents against HEH. A phase II trial is currently exploring the potential of Trametinib (MEK inhibitor) in patients with locally advanced, metastatic or unresectable tumor [33]. Another phase II trial is studying Eribulin (microtubule growth inhibitor) as a possible treatment for metastatic or locally advanced HEH [34].
To the best of our knowledge, this is the largest study and one of the most contemporary reports comparing the treatment outcomes of patients with HEH. It further supports the recommendations for surgical intervention for patients with HEH when possible. As a SEER-based study with patients representing a large national scale, the results of this study have relatively high external validity and can be generalized. However, it is a retrospective study with several limitations. First, the SEER database entails a limited number of patients’ variables and characteristics. No data exist on disease free survival, number of nodules, localization of tumor and liver lobes involved, lymph nodes involved, vascular invasion, sites of distant metastasis, chemotherapy regimen details and completeness of resection (R0-R1-R2). Data on the specific type of liver resection are also limited. Second, treatment of patients might have been based on physicians’ assessment of patient’s performance status and specific comorbidities not captured by the database, which may lead to a selection bias in the patients referred to surgery. Finally, limited by the small number of patients undergoing transplantation in our cohort, a comparison between tumor resection and transplantation was not performed. While the value of liver transplantation has been clearly shown in different reports, liver resection still occupies its role in the treatment of HEH depending on number of lesions and localization. Further investigations are merited to decide on the better treatment strategy for the different presentations of HEH.
Conclusion
Hepatic hemangioendothelioma is a rare disease that is poorly understood. Surgical intervention, whether liver resection or liver transplantation, might be warranted regardless of disease stage. Multicenter collaborations are needed to improve our limited knowledge about this neoplasm and determine the best treatment strategy.
References
Lau K, Massad M, Pollak C et al (2011) Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: insights from an internet registry in the study of a rare cancer. Chest 140:1312–1318
Weiss SW, Enzinger FM (1982) Epithelioid hemangioendothelioma: a vascular tumor often mistaken for a carcinoma. Cancer 50:970–981
Sardaro A, Bardoscia L, Petruzzelli MF et al (2014) Epithelioid hemangioendothelioma: an overview and update on a rare vascular tumor. Oncol Rev 8:259
Virarkar M, Saleh M, Diab R et al (2020) Hepatic Hemangioendothelioma: An update. World J Gastrointest Oncol 12:248–266
Makhlouf HR, Ishak KG, Goodman ZD (1999) Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer 85:562–582
Frider B, Bruno A, Selser J et al (2005) Kasabach–Merrit syndrome and adult hepatic epithelioid hemangioendothelioma an unusual association. J Hepatol 42:282–283
Lau A, Malangone S, Green M et al (2015) Combination capecitabine and bevacizumab in the treatment of metastatic hepatic epithelioid hemangioendothelioma. Ther Adv Med Oncol 7:229–236
Cardinal J, de Vera ME, Marsh JW et al (2009) Treatment of hepatic epithelioid hemangioendothelioma: a single-institution experience with 25 cases. Arch Surg 144:1035–1039
Bostancı EB, Karaman K, Turhan N et al (2014) Selective internal radiotherapy for hepatic epithelioid hemangioendothelioma. Turk J Gastroenterol Off J Turk Soc Gastroenterol 25(1):252–253
Emad A, Fadel S, El Wakeel M et al (2020) Outcome of children treated for infantile hepatic hemangioendothelioma. J Pediatr Hematol Oncol 42:126–130
Lakkis Z, Kim S, Delabrousse E et al (2013) Metronomic cyclophosphamide: an alternative treatment for hepatic epithelioid hemangioendothelioma. J Hepatol 58:1254–1257
Sangro B, Iñarrairaegui M, Fernández-Ros N (2012) Malignant epithelioid hemangioendothelioma of the liver successfully treated with Sorafenib. Rare Tumors 4:e34
Mehrabi A, Kashfi A, Fonouni H et al (2006) Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer 107:2108–2121
Lai Q, Feys E, Karam V et al (2017) Hepatic epithelioid hemangioendothelioma and adult liver transplantation: proposal for a prognostic score based on the analysis of the ELTR-ELITA registry. Transplantation 101:555–564
Wang LR, Zhou JM, Zhao YM et al (2012) Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg 36:2677–2683https://doi.org/10.1007/s00268-012-1714-x
Gloeckler Ries LA, Reichman ME, Lewis DR et al (2003) Cancer survival and incidence from the Surveillance, Epidemiology, and End Results (SEER) program. The Oncologist 8:541–552
Otrock ZK, Al-Kutoubi A, Kattar MM et al (2006) Spontaneous complete regression of hepatic epithelioid haemangioendothelioma. Lancet Oncol 7:439–441
Kitaichi M, Nagai S, Nishimura K et al (1998) Pulmonary epithelioid haemangioendothelioma in 21 patients, including three with partial spontaneous regression. Eur Respir J 12:89–96
Komatsu Y, Koizumi T, Yasuo M et al (2010) Malignant hepatic epithelioid hemangioendothelioma with rapid progression and fatal outcome. Intern Med 49:1149–1153
Boukerrouche A (2017) Management of giant liver hemangioma. J Gastroenterol Dig Dis 2(3):12–16
Groeschl RT, Miura JT, Oshima K et al (2014) Does histology predict outcome for malignant vascular tumors of the liver? J Surg Oncol 109:483–486
Lerut JP, Orlando G, Adam R et al (2007) The place of liver transplantation in the treatment of hepatic epitheloid hemangioendothelioma: report of the European liver transplant registry. Annal Surg 246:949–957 (discussion 957)
Rodriguez JA, Becker NS, O’Mahony CA et al (2008) Long-term outcomes following liver transplantation for hepatic hemangioendothelioma: the UNOS experience from 1987 to 2005. J Gastrointest Surg Offi J Soc Surg Aliment Tract 12:110–116
Nudo CG, Yoshida EM, Bain VG et al (2008) Liver transplantation for hepatic epithelioid hemangioendothelioma: the Canadian multicentre experience. Can J Gastroenterol. https://doi.org/10.1155/2008/418485
Mosoia L, Mabrut JY, Adham M et al (2008) Hepatic epithelioid hemangioendothelioma: Long-term results of surgical management. J Surg Oncol 98:432–437
Grotz TE, Nagorney D, Donohue J et al (2010) Hepatic epithelioid haemangioendothelioma: is transplantation the only treatment option? HPB (Oxford) 12:546–553
Thomas RM, Aloia TA, Truty MJ et al (2014) Treatment sequencing strategy for hepatic epithelioid haemangioendothelioma. HPB (Oxford) 16:677–685
Krasnodębski M, Grąt M, Morawski M et al (2020) Hepatic Epithelioid Hemangioendothelioma: A Rare Disease With Favorable Outcomes After Liver Transplantation. Transplant Proc 52:2447–2449
Noh OK, Kim SS, Yang MJ et al (2020) Treatment and prognosis of hepatic epithelioid hemangioendothelioma based on SEER data analysis from 1973 to 2014. Hepatobiliary Pancreat Dis Int HBPD INT 19:29–35
Lazăr DC, Avram MF, Romoșan I et al (2019) Malignant hepatic vascular tumors in adults: characteristics, diagnostic difficulties and current management. World J Clin Oncol 10:110–135
Bachmann R, Genin B, Bugmann P et al (2003) Selective hepatic artery ligation for hepatic haemangioendothelioma: case report and review of the literature. Eur J Pediatr Surg Offi J Austrian Assoc Pediatr Surg 13:280–284
Ben-Haim M, Roayaie S, Ye MQ et al (1999) Hepatic epithelioid hemangioendothelioma: resection or transplantation, which and when? Liver Transpl Surg Off Publ Am Assoc Study Liver Dis Int Liver Transpl Soc 5:526–531
National Cancer Institute (2021) Trametinib in Treating Patients With Epithelioid Hemangioendothelioma That is Metastatic, Locally Advanced, or Cannot Be Removed by Surgery (ClinicalTrials.gov Identifier NCT03148275). Retrieved from https://clinicaltrials.gov/ct2/show/NCT03148275
Massachusetts General Hospital (2017) Eribulin in Angiosarcoma and Epithelioid Hemangioendothelioma (EHE) (ClinicalTrials.gov Identifier: NCT03331250). Retrieved from https://clinicaltrials.gov/ct2/show/NCT03331250
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chahrour, M.A., Khachfe, H.H., Habib, J.R. et al. Treatment and Prognosis of Hepatic Epithelioid Hemangioendothelioma: A SEER Database Analysis. World J Surg 45, 2886–2894 (2021). https://doi.org/10.1007/s00268-021-06165-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06165-6