Abstract
Background
This multicenter-based retrospective study aimed to investigate the prognostic factors and report our experiences with the diagnosis and treatment of hepatic epithelioid hemangioendothelioma (HEHE), a rare malignant vascular tumor.
Methods
A total of 33 patients with HEHE from two centers between 2004 and 2011 were retrospectively reviewed with respect to their clinical, radiologic, and pathologic characteristics; treatment modalities and outcomes; and potential prognostic factors.
Results
A total of 17 patients underwent liver resections (LRs) alone, 12 patients had transcatheter arterial chemoembolization (TACE) alone, three patients had LR followed by TACE, and one patient underwent liver transplantation (LT). The difference of overall survival (OS) between LR and TACE was not significant (p = 0.499). Older patients [≥47 years, n = 17; p = 0.035, hazard ratio (HR) = 7.0), those with symptoms (n = 17; p = 0.001, HR = 86.5], and those with an elevated serum CA19-9 level (>37 U/ml, n = 5; p = 0.018, HR = 5.0) had a poorer OS, according to univariate analysis. The presence of symptoms was validated as a prognostic factor (p = 0.012) by multivariate analysis.
Conclusions
Liver resection and TACE have comparable outcomes in HEHE patients. The presence of symptoms indicates a poor prognosis. Older age and elevated serum CA19-9 are potential negative impact factors on outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatic epithelioid hemangioendothelioma (HEHE) was first described by Ishak et al. [1] as a group of rare borderline vascular tumors with primary liver involvement characterized by the presence of epithelioid endothelial cells. The incidence and etiology remain uncertain, and the female-to-male ratio is approximately 1.5:1.0 to 1.6:1.0 [2, 3]. Chronic liver disease is not considered a significant cause of HEHE [2, 4–6]. Although many patients (25–42 %) are asymptomatic at the time of diagnosis [2, 3], the most frequent symptoms include unspecific right upper quadrant pain, weight loss, fatigue, and jaundice [2, 3, 7]. Imaging findings are commonly nonspecific. Diagnosis of HEHE is based on its characteristic histologic structures and positive staining for factor VIII-related antigen (FVIIIAg), CD34, and CD31 [6].
Several treatment strategies have been explored, including liver resection (LR), liver transplantation (LT), systemic/regional chemotherapy, and radiotherapy [3]. Favorable outcomes of LT were observed in several studies [8–11]. The Mayo Clinic reported comparable results for LR (11 cases) and LT (11 cases) [10]; however, the effectiveness of transcatheter arterial chemoembolization (TACE), one of the main treatments for primary liver malignancies, is not clear; and comparisons between TACE and surgical treatments have not been performed.
Here we report 33 patients from two centers with and aim of comparing the therapeutic options. We also investigated the prognostic factors for HEHE.
Materials and methods
Patients and follow-up
A retrospective study was performed on 33 patients who received treatment for HEHE at the Liver Cancer Institute and Zhongshan Hospital, Fudan University (n = 22), and at Eastern Hepatobiliary Surgery Hospital, Second Military Medical University (n = 11) between March 2004 and June 2011. All of the patients had serum tests and at least one of the following imaging examinations: ultrasonography (US), computed tomography (CT), and/or magnetic resonance imaging (MRI). The diagnosis of HEHE was based on histologic features (including cellularity, fibrosis status, and sinusoid infiltration) and positive immunohistochemical (IHC) staining for CD34, CD31, and FVIIIAg. Therapeutic modalities included LR, TACE, LR followed by TACE, and LT.
All patients were followed through August 2011, with a median follow-up time of 17 months (range 0.25–80.0 months). Following surgery, disease status was monitored by abdominal US or CT every 2–6 months. Overall survival (OS) was defined as the interval between surgery and death.
Statistical analysis
Data were expressed as medians, ranges, and 95 % confidence intervals (95 % CIs). Quantitative variables were compared using the Mann–Whitney U-test. Proportions were compared using the χ2 test or Fisher’s exact test. Survival estimates were calculated using Kaplan–Meier methods, and survival comparisons were performed using the log-rank test. The Cox regression model was used to identify risk and to perform a multivariate analysis. The data were analyzed using statistical software (SPSS 16; SPSS, Chicago, IL, USA). We considered p < 0.05 statistically significant.
Results
Clinical characteristics
The study consisted of 16 men (48.5 %) and 17 women (51.5 %), with a median age of 47 years (range 20–80 years) at the time of diagnoses. In all, 16 patients (48.5 %) were asymptomatic and incidentally diagnosed for HEHE. Another 12 patients (36.4 %) presented with abdominal pain or discomfort in the right upper quadrant. Rare symptoms included chest pain (n = 3), weight loss (n = 1), and jaundice (n = 1). Metastases were found in six patients (18.2 %) (four cases of lung metastases and two of diaphragm/abdominal-wall metastases). Serum α-fetoprotein (AFP) and carcinoembryonic antigen (CEA) levels were normal in all patients. Serum CA19-9 was elevated in five patients. All patients were hepatitis B surface antigen (HBsAg)-negative, and only one patient had mild liver cirrhosis (Supplementary Table 1).
Imaging findings
Imaging tests prior to treatment found multinodular lesions in 22 patients (66.6 %) and mononodular lesions in 11 patients (33.3 %). The median tumor diameter was 3.6 cm (range 1.5–15.0 cm). The radiologic diagnosis concurred with the histologic diagnosis in only three patients. The other 30 patients were initially diagnosed with metastatic tumor (n = 13), cholangiocellular carcinoma (n = 9), hepatocellular carcinoma (n = 2), benign neoplasm (n = 3), hemangioma (n = 2), or hemangiosarcoma (n = 1).
Ultrasonography was performed in 31 patients. It revealed hypoechoic lesions in 28 of these patients and hyperechoic lesions in the other 3 patients. Color Doppler flow imaging results were heterogeneous in various patients; they revealed blood flow distribution, including punctiform or filiform arterial spectra as well as an absence of blood flow.
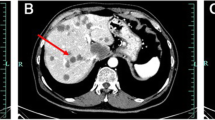
Computed tomography was performed in 20 patients. They all had hypodense lesions on the plain scans, with slight peripheral or partial enhancement at the arterial phase and different degrees of enhancement at the portal venous phase or lag phase (Fig. 1a–c).
Computed tomography scan shows hypodense lesions in the plain scan (a) and partial enhancement at the arterial phase (b) and the portal venous phase (c). Magnetic resonance imaging scans show d hypointensity on T1-weighted imaging (T1WI), e high signal intensity on T2-weighted imaging (T2WI), and f peripheral enhancement in the portal venous phase
The MRI scans, performed in 14 patients, showed hypointensity on T1-weighted imaging (T1WI) and intermediate to high signal intensity on T2-weighted imaging (T2WI) and diffusion-weighted imaging (DWI). Lesions in 13 patients were enhanced in 10 patients either in the arterial or portal venous phase and in three patients in both phases (Fig. 1d–f).
Histological findings
A total of 21 patients underwent postoperative histologic tests, and the other 12 were examined by core needle biopsy. Microscopically, fibrous tissue hyperplasia with a sprinkling of epithelioid cells with atypical nuclei and characteristic intracytoplasmic lumens containing red blood cells, which resembled signet ring-like structures, were observed. Immunohistochemically, CD31, CD34, and FVIIIAg staining were positive in most cases (CD31, 28/30; CD34, 28/30; FVIIIAg, 24/25; (Fig. 2). Positive vimentin, S-100, α-SMA, and CK8 staining was also found in some patients (Table 1).
Treatment and clinical outcomes
Severe postoperative complications (i.e., liver failure, multiple organ dysfunction syndrome) occurred in only one patient. The patient with bilobed disease and multinodular lesions was treated with TACE; he died 7 days after the operation as a result of liver failure. Common complications in patients who underwent LR were temporary hepatic dysfunction (41 %) and hydrothorax (12 %). Common complications in patients who underwent TACE were fever (92 %), temporary hepatic dysfunction (42 %), abdominal pain (42 %), and gastrointestinal disorders—anorexia, nausea, vomiting, and/or diarrhea (33 %). All common complications could be treated and lasted no more than 2 weeks.
The 3-year survival rate of all patients in this study was 73.3 %. Eight patients died before the end of the study: seven of primary disease and one of liver failure after TACE. The only patient who underwent LT survived for 12 months after surgery, and the 3 patients who underwent LR followed by TACE survived for 16, 27, and 80 months respectively. There was no significant difference in OS between the 17 patients who underwent LR alone (3-year survival rate 74.1 %) and the 12 who underwent TACE alone (3-year survival rate 81.6 %; p = 0.499). The LR group had significantly more female patients (P = 0.025), and significantly fewer patients with multiple lesions (p = 0.001) and lesions invading both lobes of the liver (p = 0.001) (Table 2). To avoid statistical bias from these factors, we performed analyses in subgroups stratified according to sex, tumor number, and distribution. After this stratification, there were still no significant differences in OS between the subgroups (Table 3).
We evaluated the prognostic values of clinicopathologic characteristics in all patients by univariate analyses and found that the following factors were associated with poorer OS: (1) older age (≥47 years): the 3-year survival rate was 56.1 versus 93.8 % [older age versus younger age (<47 years)]: p = 0.035, hazard ratio (HR) = 7.0, 95 % confidence interval (CI) 0.9–55.5; (2) presence of symptoms: the 3-year survival rates were 47.4 versus 100 % (symptomatic versus no symptoms): p = 0.001, HR = 86.5, 95 % CI 0.3–2.8 × 104; (3) elevated serum CA 19-9 (≥37 U/ml): 3-year survival rates were 40.0 versus 80.1 % [high versus low (<37 U/ml) CA19-9]: p = 0.018, HR = 5.0, 95 % CI 1.1–21.9 (Fig. 3). When these three factors were analyzed using a multivariate analysis, only the presence of symptoms was validated as an independent prognostic factor (p = 0.012) (Table 4).
Discussion
By and large, the characteristics of the patients in this study were consistent with those in previous investigations; however, this study also revealed some interesting findings. In terms of symptoms, chest pain was a complaint in three patients. Each of these patients had multiple lesions involving both liver lobes. One patient had hydrothorax, one had lung metastasis, and one had both. The suspected reasons for the chest pain were nerve invasion or reactive inflammation caused by lung metastases and primary tumors distributed close to the diaphragm, causing inflammation and pain. In-depth imaging examinations would be particularly important for such patients to find all primary and secondary tumors. Another interesting finding was the elevation of serum CA19-9 in five patients, which could be a prognostic marker, as discussed later. Histopathologic study remained the most reliable diagnostic method, and we found vimentin-, S-100-, α-SMA-, and CK8-positive staining in most of those who had underwent this testing. Further study in a large sample size is needed to confirm these results.
The therapeutic modalities of HEHE included LT, LR, chemotherapy, radiotherapy, hormone therapy, ablation, and surveillance alone. LT remained the most common therapeutic modality, and the results were satisfactory. According to Mehrabi et al. [3], after reviewing 101 patients who underwent LT and had available follow-up data, the 5-year survival rate was 54.5 %. The Europe Liver Transplant Registry and the United Network for Organ Sharing Registry reported 5-year survival rates of 83 and 64 % in 59 and 110 patients, respectively [9, 11]. A single-institution study reported that the mean OS in 17 patients who underwent LT was 172 months (95 % CI 124–220 months) [8]. However, LT was limited in practicality because of donor shortages, high cost, lifelong immunosuppressant therapy, and patient willingness in that study.
The Mehrabi review reported that the 5-year survival rates after LR (22 patients), chemotherapy/radiotherapy (60 patients), and surveillance (70 patients) were 75.0, 30.0, and 4.5 %, respectively [3]. The Mayo Clinic reported comparable results for LT (11 patients) and LR (11 patients), with 5-year survival rates of 73 and 86 %, respectively [10]. However, whether extrahepatic involvement should be a contraindication for surgical treatments is still under debate [8–10].
The role of single nonsurgical therapies (e.g., systemic/regional chemotherapy, radiotherapy, hormone therapy, immunotherapy) has been studied in only a limited number of small series studies [12, 13]. It is therefore difficult to assess the outcomes because of the limited data. Despite this, systemic/regional chemotherapy and radiotherapy are recommended adjuncts to LT—or the best therapeutic choices when LT is excluded [3, 8].
To our knowledge, the present study is the largest one to date comparing the outcomes of LR (17 patients) and TACE (12 patients). The OSs of the two approaches were comparable. Although there were more male patients, bilobed involvement, and multinodular lesions involved in the TACE group, the differences did not affect the statistical comparisons between the two groups.
Given our findings, LR and TACE are both acceptable treatments in patients with resectable intrahepatic lesions. Also, TACE is recommended if the lesions are unresectable. According to previous findings [3, 8–13], LT has favorable outcomes in HEHE patients, yet its indications are not well defined. Additional investigations in larger studies are needed to compare further the differences between LT and other treatments.
The prognostic factors of HEHE remain unclear. The presence of extrahepatic disease beyond regional portal nodes had been reported as a negative predictor of outcome [8], although it was not confirmed in our study. Rather, we found, through univariate analyses, that the presence of symptoms, older age, and elevated serum CA19-9 were negative predictors of patient outcomes. The disagreements with the multivariate analysis regarding the latter two are likely a result of the influence of patient number on the model’s stability. These factors should be further investigated in studies with larger patient numbers to characterize the interactions among the parameters.
The presence of symptoms is a commonly accepted sign of disease progression in patients with liver malignancies. The symptoms we report (abdominal pain/discomfort, chest pain, jaundice, weight loss) could be caused by progressive disease hallmarks such as increased tumor size, increasing numbers of lesions, and either detectable or latent metastasis. Although the number of patients in the present study was not sufficient to show differences in disease progression between symptomatic and asymptomatic patients, the association could not be excluded.
In the present study, we report, for the first time, the elevation of serum CA19-9 as a negative prognostic factor. Serum CA19-9 level is a widely accepted biomarker for colon cancer and pancreatic cancer [14]. CA19-9 is also elevated in some benign liver diseases and biliary obstruction [15]. Normal biliary epithelial cells secrete mucins carrying the epitope of CA19-9. Unspecific elevation of serum CA19-9 could reflect both inflammatory hypersecretion and leakage of biliary mucins into serum [16]. Moreover, high serum levels of CA19-9 are reported to be associated with distant or lymph node metastasis in such malignancies as gastric and colorectal cancer [17, 18]. Thus, potential reasons for the elevation of serum CA19-9 in HEHE patients are (1) obstruction caused by the larger mass or increased number of lesions, (2) inflammation that results in local accumulation and leakage of CA19-9 into the circulation, and/or (3) latent metastases. Any of these conditions could lead to poorer outcomes in patients with liver tumors [19], but direct relations between them and OS in HEHE were not confirmed in the present study and so warrant further study. Additionally, CA19-9 is found to be a potent ligand for endothelial cell leukocyte adhesion molecule-1 (ELAM-1) and may block leukocyte interactions with ELAM-1. Thus, circulating CA19-9 containing mucins in serum could cause pathologic immune depression through this pathway [20]. Therefore, we hypothesize that CA19-9 may be not only an indicator of but also a contributor to the poor prognosis for patients with HEHE. The underlying mechanism and role of elevated serum CA19-9 in HEHE patients needs further investigation.
As this study was retrospective, a selection bias existed regarding the different characteristics of patients in the LR and TACE treatment groups. Additionally, the small numbers of patients limited statistical analysis of the prognostic factors. We look forward to larger, prospective studies of HEHE, which will be able to better estimate the treatment outcomes, define prognostic parameters, and examine the interactions between them.
Conclusions
Our finding that HEHE patients treated with LR and TACE had similar outcomes brings new understanding to the therapeutic guidelines. Furthermore, we determined that the presence of symptoms was a negative prognostic factor and that older age and elevated serum CA19-9 levels were potentially negative impact factors on patient outcomes. Thus, these findings can provide a reference for estimating the prognosis of HEHE.
References
Ishak KG, Sesterhenn IA, Goodman ZD et al (1984) Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study of 32 cases. Hum Pathol 15:839–852
Makhlouf HR, Ishak KG, Goodman ZD (1999) Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer 85:562–582
Mehrabi A, Kashfi A, Fonouni H et al (2006) Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer 107:2108–2121
Dail DH, Liebow AA, Gmelich JT et al (1983) Intravascular, bronchiolar, and alveolar tumor of the lung (IVBAT): an analysis of twenty cases of a peculiar sclerosing endothelial tumor. Cancer 51:452–464
Miller WJ, Dodd GD III, Federle MP et al (1992) Epithelioid hemangioendothelioma of the liver: imaging findings with pathologic correlation. AJR Am J Roentgenol 159:53–57
Lin J, Ji Y (2010) CT and MRI diagnosis of hepatic epithelioid hemangioendothelioma. Hepatobiliary Pancreat Dis Int 9:154–158
Läuffer JM, Zimmermann A, Krähenbühl L et al (1996) Epithelioid hemangioendothelioma of the liver: a rare hepatic tumor. Cancer 78:2318–2327
Cardinal J, de Vera ME, Marsh JW et al (2009) Treatment of hepatic epithelioid hemangioendothelioma: a single-institution experience with 25 cases. Arch Surg 144:1035–1039
Lerut JP, Orlando G, Adam R et al (2007) The place of liver transplantation in the treatment of hepatic epitheloid hemangioendothelioma: report of the European Liver Transplant Registry. Ann Surg 246:949–957
Grotz TE, Nagorney D, Donohue J et al (2010) Hepatic epithelioid haemangioendothelioma: is transplantation the only treatment option? HPB (Oxford) 12:546–553
Rodriguez JA, Becker NS, O’Mahony CA et al (2008) Long-term outcomes following liver transplantation for hepatic hemangioendothelioma: the UNOS experience from 1987 to 2005. J Gastrointest Surg 12:110–116
Simpson ND, Ahmed AM, Simpson PW et al (2003) Living donor liver transplantation in a patient with hepatic epithelioid hemangioendothelioma. J Clin Gastroenterol 37:349–350
Galvão FH, Bakonyi-Neto A, Machado MA et al (2005) Interferon alpha-2B and liver resection to treat multifocal hepatic epithelioid hemangioendothelioma: a relevant approach to avoid liver transplantation. Transplant Proc 37:4354–4358
Maciej U, Anna L (2002) Sialyl Lewisa: a tumor-associated carbohydrate antigen involved in adhesion and metastatic potential of cancer cells. Acta Biochim Pol 49:304–308
Robertson AG, Davidson BR (2007) Mirizzi syndrome complicating an anomalous biliary tract: a novel cause of a hugely elevated CA19-9. Eur J Gastroenterol Hepatol 19:167–169
von Ritter C, Eder MI, Stieber P et al (1997) Biliary mucin secreted by cultured human gallbladder epithelial cells carries the epitope of CA 19–9. Anticancer Res 17:2931–2934
Nakagoe T, Sawai T, Tsuji T et al (2001) Circulating sialyl Lewis(x), sialyl Lewis(a), and sialyl Tn antigens in colorectal cancer patients: multivariate analysis of predictive factors for serum antigen levels. J Gastroenterol 36:166–172
Nakagoe T, Sawai T, Tsuji T et al (2002) Predictive factors for preoperative serum levels of sialyl Lewis(x), sialyl Lewis(a) and sialyl Tn antigens in gastric cancer patients. Anticancer Res 22:451–458
Budhu A, Forgues M, Ye QH et al (2006) Prediction of venous metastases, recurrence, and prognosis in hepatocellular carcinoma based on a unique immune response signature of the liver microenvironment. Cancer Cell 10:99–111
Berg EL, Robinson MK, Mansson O et al (1991) A carbohydrate domain common to both sialyl Le(a) and sialyl Le(x) is recognized by the endothelial cell leukocyte adhesion molecule ELAM-1. J Biol Chem 266:14869–14872
Acknowledgments
We thank Wei-De Zhang for his active contribution to this article. This study was jointly supported by the National Natural Science Funds of China (No. 30973499), the National S&T Major Project (No. 2008ZX10002-026), and the Dawn Program of the Shanghai Education Commission (No. 07SG04).
Disclosure
There are no financial disclosures from any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Long-Rong Wang, Jia-Min Zhou, Yi-Ming Zhao, and Hong-Wei He contributed equally to this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, LR., Zhou, JM., Zhao, YM. et al. Clinical Experience with Primary Hepatic Epithelioid Hemangioendothelioma: Retrospective Study of 33 Patients. World J Surg 36, 2677–2683 (2012). https://doi.org/10.1007/s00268-012-1714-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1714-x