Abstract
Background
Adrenal ganglioneuromas (AGNs) are extremely rare benign neoplasms. This study is to share our experience regarding diagnostic and operative management of these tumors.
Methods
Clinical details as well as follow-up data were retrospectively analyzed in 42 primary AGN patients who received operative resection at a tertiary referral hospital in China between May 2005 and July 2016.
Results
The mean age of the patients at diagnosis was 35.3 years (range 13–59 years). Among the patients, 28 were asymptomatic. The mean preoperative size was 5.3 ± 2.2 cm (range 2.1–14.0 cm), and 17 cases were larger than 5 cm. All patients underwent operative resection as open adrenalectomy in 20 patients and laparoscopy in 22 patients. The mean tumor size on pathologic examination was 6.0 ± 2.6 cm (range 2.2–17.0 cm). Laparoscopic operation showed its advantages over open surgery on the postoperative duration (5.0 vs. 7.3 days, p < 0.001) and estimated blood loss (69.5 vs. 157.5 ml, p = 0.047). No patient had recurrence or metastasis during a median follow-up of 70.5 months (range 3.7–164.3 months).
Conclusions
We describe the largest AGN series reported to date. The preoperative diagnosis of AGN remains difficult despite of the progression of imaging examination. After complete resection, the prognosis of AGN patients is excellent. Laparoscopic approach has its advantages in the resection of AGNs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ganglioneuroma (GN) is a benign neurogenic tumor that originates from primordial neural crest cells, consisting of mature Schwann cells, ganglion cells and nerve fibers [1]. It mainly occurs in the posterior mediastinum and retroperitoneum. Adrenal ganglioneuroma (AGN) is rare, accounting for 20% of the disease entity [2]. Owing to its low incidence, only a few case reports and small case series on AGN have been reported so far.
The small number of patients and heterogeneous groups in these studies limit a comprehensive understanding of AGN. In this study, we share our experience regarding the clinical features, diagnostic imaging, and operative treatment of 42 AGN cases in China. For the first time, we compared the laparoscopic and open approaches in the operation of AGNs.
Materials and methods
This study conformed to Declaration of Helsinki and protocol involving human materials was approved by the Institutional Ethic Committee of Ruijin Hospital. Between May 2005 and July 2016, 2516 patients received an adrenalectomy in our hospital and 42 patients were pathologically diagnosed as AGN. Their clinical, diagnostic, operative findings as well as follow-up data were collected retrospectively from the data base of our department.
Diagnostic work-up
All patients’ demographic parameters, chief complaint, concomitant disease and operative history were analyzed. All patients performed ultrasonography, and 37 patients were evaluated with enhanced computed tomography (CT), 10 patients with magnetic resonance imaging (MRI). The precontrast and postcontrast Hounsfield units (HU), maximum diameter, characteristics and preoperative diagnosis were analyzed. One patient underwent image-guided fine needle aspiration biopsy (FNAB) before operation.
Baseline biochemical and hormonal assessments were performed in 37 patients, which included at least: (1) serum potassium; (2) plasma adrenocorticotrophic hormone (at 8:00 am) and cortisol (at 0:00 am, 8:00 am and 4:00 pm); (3) 24-h urinary free cortisol; (4) plasma renal activity and aldosterone (upright and decubitus); (5) serum metanephrine and normetanephrine; (6) 24-h urinary epinephrine, norepinephrine, dopamine and vanillylmandelic acid; (7) serum dehydroepiandrosterone.
Operations
Indications for surgery were symptoms (discomfort/pain) attributed to AGN, tumor size > 3 cm and radiologic suspicion of malignancy. Traditional open or laparoscopic operations were performed according to the preoperative diagnosis, the willingness of patients and the surgeon’s preference. There were 2 surgeons involved in the operative management of these patients. They performed laparoscopic adrenalectomy expertly after independently accomplishing 20 and 25 laparoscopic adrenalectomy, respectively. Operative time, estimated blood loss (EBL), postoperative hospital stay and complications were assessed in both open and laparoscopic groups.
Histological evaluation and follow-up
Surgical specimens were evaluated by gross pathology and light microscopy, and immunohistochemistry was performed for equivocal cases. The microscopic features of AGN, resection margin status and pathologic diagnosis were reported by 2 experienced pathologists.
Patients were generally followed 1 month after operation, every 3 months for the first year, every 6 months for the second year, and every 12 months thereafter. Biochemical and cortisol assessments were performed routinely. Abdomen and pelvic cavity computed tomography were performed every 6 months for the first year and annually thereafter. The status of each patient was assessed by follow-up or telephone call.
Statistical methods
Continuous variables were presented as the mean and standard deviation. The statistical significance of continuous data was evaluated by t test and a value of p < 0.05 was considered significant. All statistical computations were performed using SPSS, version 21.0.
Results
Clinical and hormonal findings
Adrenal ganglioneuroma accounted for 1.7% (42/2516) of all adrenalectomies that were performed in our hospital between May 2005 and July 2016. Table 1 summarizes essential demographic characteristics and clinical presentations of the 42 patients. There were 24 AGN patients with tumor size < 5 cm,among which 18 (75.0%) were incidentally detected during routine check-ups, 5 (20.8%) presented with abdominal or back discomfort, and 1 (4.2%) with menstrual disorder.
Baseline hormonal work-up was performed in 37 (88.1%) patients. Serum potassium was normal in all the 37 patients and no hormonal secretion was apparent in 34 (91.9%) patients. One patient was found with marginally increased plasma adrenocorticotrophic hormone and 24-h urinary free cortisol, one patient with mildly increased 24-h urinary epinephrine and dopamine, and one patient with significantly elevated level of serum metanephrine (7959.2 pg/ml with normal upper limit < 90 pg/ml) and normetanephrine (2550.9 pg/ml with normal upper limit < 121 pg/ml).
Imaging Findings
All adrenal lesions in this study were unilateral and 22 (52.4%) were right sided, with 17 (40.5%) surrounding or pushing the inferior vena cava. The mean preoperative size was 5.3 ± 2.2 cm (range 2.1–14.0 cm) in the largest diameter, and 17 cases were larger than 5 cm. The tumors were oval in 28 patients and lobulated in the remaining 14 patients. Calcification was noted in 14 (33.3%) patients.
Generally, AGNs were hypoechoic, well-demarcated and with no blood flow signal on ultrasonography images (Fig. 1). In 2 cases, AGNs presented as medium echo masses with a few blood flow.
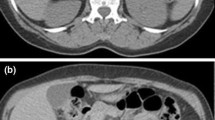
Of the 37 patients undergoing CT scan, Only 7 (18.9%) were diagnosed as AGN, 19 were inconclusive, and 11 were considered as adrenal adenoma. On unenhanced CT images (Fig. 2a), AGNs had a median density of 31.6 HU (range 21–39 HU). Slight enhancement was seen on postcontrast CT images (Fig. 2b), with a median density of 39.8 HU (range 30–54 HU). In the excretory phases (Fig. 2c), AGNs had progressive enhancement, with a median density of 53.2 HU (range 40–70 HU). Moreover, CT images showed homogeneous lesions in 23 (62.2%)patients, with no evidence of surrounding tissue infiltration or regional lymph node enlargement (Fig. 2d).
On MRI (n = 10), AGNs demonstrated hypo-intense signal on T1-weighted images (Fig. 3a) and hyper-intense signal on T2-weighted images (Fig. 3b). Six patients underwent 131I-MIBG and no one showed an increased uptake. One patient received FDG-PET scan, which showed a mildly increased uptake with a maximum standardized uptake value of 2.1. FNAB was performed in one case and was diagnostic.
Treatment and follow-up
All 42 patients underwent operative resection as open adrenalectomy in 20 patients and laparoscopy in the other 22 patients. The mean preoperative tumor size was 5.8 ± 1.6 cm (range 3.5–10 cm) and 4.9 ± 2.5 cm (range 2.1–14.0 cm) for the open and laparoscopic group (p = 0.166), respectively. In the open group, two patients had a history of cesarean before surgery, and one patient had appendectomy. In the laparoscopic group, two patients had a history of endoscopic colon polyps resection, one patient had appendectomy, and one had left thyroidectomy.
For the laparoscopic and open group, the mean EBL was 69.5 vs. 157.5 ml (p = 0.047), the mean operative time was 140.8 versus 129.5 min (p = 0.451), and the mean postoperative duration was 5.0 versus 7.3 days (p < 0.001), respectively. There was no mortality, minor morbidity or complications in our patients. During a median follow-up of 76.5 months (range 12.7–164.3 months), no patients showed recurrence or metastasis on serial imaging evaluations. The abdominal discomfort of 5 patients was relieved after the adrenalectomy, while symptoms of hypertensive, headache, palpitation and menstrual disorder in 4 patients remained.
Histopathology
All patients showed clear resection margins. The mean tumor size on pathologic examination was 6.0 ± 2.6 cm (range 2.2–17.0 cm) on maximum diameter. Grossly, AGNs were firm, well circumscribed nodular masses, with a tan-white or tan-pink section (Fig. 4). No AGNs showed hemorrhage, cystic degeneration or necrosis. Microscopically, the neoplasms had typical GN features, including dispersed well-differentiated ganglion cells and fascicles of spindle cells (Fig. 5). Ganglion cells were characterized by abundant basophilia cytoplasm and hyperchromatic nuclei with obvious nucleoli. Microscopic foci of mature neuroblastic cells and hypercellularity were noticed in 2 patients. No areas of pheochromocytoma, tumor cell necrosis, or mitosis, were seen. Immunohistochemistry staining was employed in 5 patients, and 4 patients showed positive staining for neuron-specific enolase and S-100.
Discussion
The incidence of ganglioneuroma in patients undergoing adrenalectomies ranges from 0.3 to 9.4% [3, 4]. In this study, the incidence of AGN among such patients was 1.7%, similar to another recent research [5]. It was previously reported that AGNs occur more frequently in young adults and older children, the mean ages at diagnosis for patients with AGNs were 31, 39.2, 49, 50 years in America, China, Canada and Greece, respectively [4, 6,7,8]. In our series, the mean age at diagnosis was 35.3 years, and no patient was diagnosed during childhood.
Owing to the indolent behavior and hormonal inactivity, AGN is usually asymptomatic and discovered serendipitously. In some patients, AGN may produce nonspecific symptoms such as abdominal or back pain/discomfort [7], or secrete catecholamine [8]. Less common manifestations include hypertensive crises, VIP-related diarrhea and virilization [9,10,11]. Our results showed routine medical examination, especially ultrasonography, was the main approach leading to the discovery of AGN. Moreover, we noticed that there was no direct correlation between tumor size and the symptoms in AGN patients. For instance, one man with a 3.1 cm AGN complaint with back discomfort for 1 year, while another man with a 14.0 cm tumor was asymptomatic.
Although AGNs are mainly discovered by ultrasonography, the ultrasonic manifestations of AGNs were not well documented in the previous literatures. In this study, we carefully evaluated the ultrasonography images in 42 patients, and thought the clues for AGN was: hypoechoic, well-demarcated adrenal mass, usually > 3 cm and with no blood flow signal. Under some special conditions such as pregnancy, ultrasonography might be a repeatable and feasible method for the monitor of adrenal mass suspected as AGN.
Imaging characteristics of AGN on CT have been described as low attenuated, homogeneous masses which demonstrate slight to moderate enhancement, and with no vascular involvement [12, 13]. The presence of calcifications was reported as another clue [14]. We held the opinion that both homogeneity and calcification were unreliable indicators for AGN. In our study, a considerable part (40.5%) of AGNs presented as heterogeneous and only 33.3% of AGNs showed calcifications. Actually, Bin et al. has pointed out that the homogeneity of GNs varies from tumor to tumor due to the different proportions of ganglions and Schwann cells [15]. Likewise, the proportion of calcifications is also reported to fluctuate greatly, from 0 to 82.4% [5, 16]. Through our observation, we recommended these clues for AGNs on CT: well circumscribed, low attenuated (below 40 HU on precontrast CT), progressive delayed enhancement, surround but not infiltrate peripheral tissues, and with no lymph node enlargement.
On MRI, AGNs generally demonstrate a hypo-intense signal on T1-weighted images and a heterogeneous hyper-intense signal on T2-weighted images [17]. Our results were in accordance with these features. Whole body PET using 18FDG was reported to be highly accurate in the differentiation of malignant adrenal masses [18, 19]. However, it could also misdiagnose primary ganglioneuroma as adrenal metastasis [8]. In this study, one AGN patient underwent FDG-PET and was misdiagnosed as adrenal adenoma, revealing that PET has no significant advantage in the diagnosis of AGN. Although there has been reported positive 131MIBG uptake of AGN in adults [8], the MIBG results of six AGN patients in our hospital were all negative.
The application of FNAB in the diagnosis of adrenal masses has long been reported [20]. However, it remains controversial due to the insufficient material for diagnosis and a few complications [21, 22]. In our series, one AGN patient underwent CT-guided FNAB and obtained accurate diagnosis. Considering its potential risky procedure, we thought FNAB should be avoided when the outcome had no effect on our decision to operate.
Prognosis of AGN is excellent. In a previous study, one AGN patient underwent subtotal resection and had no recurrence during a median follow-up of 50 months; three patients did not have surgery and died from causes unrelated to AGNs [6]. However, the preoperative diagnosis of AGN remains difficult and the potential malignance cannot be completely excluded. In addition, the malignant transformation of AGN has also been reported [23]. Thus, complete resection is strongly recommended for adrenal masses, despite the suspicion of AGN. Open or laparoscopic operations were chosen according to the surgeon’s preference, and tumor size should not be a major factor in the decision. In the past, adrenal mass was removed laparoscopically only when it was < 6 cm. However, as the improvement of laparoscopic apparatus and surgical technique, the size for laparoscopic adrenalectomy has been constantly extended in recent years. It has been reported laparoscopic resection of AGN with the size up to 13 cm [24]. As long as the tumor does not infiltrate peripheral tissues and laparoscopic operation space can be ensured, we think giant adrenal mass can also be removed safely through laparoscopy. In this study, all AGNs were completely resected with no mortality or complications despite the large size of the masses.
Due to the rarity of AGNs, the safety and effectiveness between open and laparoscopic operations have not been compared. We found laparoscopic operation had its advantages over open surgery on the postoperative duration and EBL, with no prolonged operative time. One AGN patient with 17.0 cm mass received laparoscopic operation in our hospital, and discharged from hospital with no complications 6 days after surgery. The postoperative laparoscopic stay in these AGN patients was longer compared to some studies associated with laparoscopic adrenalectomy [25, 26]. Since AGN is a rare entity, we preferred to observe these patients longer to reduce the potential postoperative complication risks in the early stage of laparoscopic technique. As our experience grows, the postoperative laparoscopic duration of AGN is continually shortening and it currently averages approximately 3 days. In previous literature, posterior retroperitoneoscopic adrenalectomy (PRA) is associated with decreased operation time, length of stay, blood loss and complication rates compared to laparoscopic transabdominal technique (LTA) [25,26,27]. Theoretically, PRA eliminates the mobilization of adjacent structures and reduces the risks of complications such as bowel injury and postoperative adhesions. In this study, 13 AGN patients with < 6 cm in size underwent PRA while only 3 AGN with < 6 cm in size received transperitoneal approach. Since it is statistically invalid to compare these 2 groups, the most advantageous laparoscopic approach in AGN with < 6 cm in size still needs further investigation.
In rare tumors, retrospective analysis is often the only feasible method to document the characteristics of these entities. Our study had the inherent shortcomings of retrospective reviews, including detection and selection biases. In addition, AGN patients who did not receive surgery were not enrolled thus could limit the generalization of treatment. Nevertheless, we believe that our data applied valuable information related to AGN.
In conclusion, we describe the largest AGN series reported to date. Adrenal ganglioneuromas are rare benign tumors mostly occurring in young adults. It is mainly discovered by routine medical checkup and the preoperative diagnosis of AGN remains difficult. After complete resection, the prognosis of AGN patients was excellent. Laparoscopic approach had its advantages in the resection of AGNs.
References
Enzinger FM, Weiss SW (1995) Ganglioneuroma. In: Soft tissue tumors, 3rd edn. St Louis, pp 929–964
Geoerger B, Hero B, Harms D et al (2001) Metabolic activity and clinical features of primary ganglioneuromas. Cancer 91:1905–1913
Kasperlik-Zaluska AA, Roslonowska E, Slowinska-Srzednicka J et al (2006) 1,111 patients with adrenal incidentalomas observed at a single endocrinological center: incidence of chromaffin tumors. Ann N Y Acad Sci 1073:38–46
Qing Y, Bin X, Jian W et al (2010) Adrenal ganglioneuromas: a 10-year experience in a Chinese population. Surgery 147:854–860
Lee JH, Chai YJ, Kim TH et al (2016) Clinicopathological features of ganglioneuroma originating from the adrenal glands. World J Surg 40:2970–2975. https://doi.org/10.1007/s00268-016-3630-y
Shawa H, Elsayes KM, Javadi S et al (2014) Adrenal ganglioneuroma: features and outcomes of 27 cases at a referral cancer centre. Clin Endocrinol 80:342–347
Rondeau G, Nolet S, Latour M et al (2010) Clinical and biochemical features of seven adult adrenal ganglioneuromas. J Clin Endocrinol Metab 95:3118–3125
Linos D, Tsirlis T, Kapralou A et al (2011) Adrenal ganglioneuromas: incidentalomas with misleading clinical and imaging features. Surgery 149:99–105
Erem C, Kocak M, Cinel A et al (2008) Dopamine-secreting adrenal ganglioneuroma presenting with paroxysmal hypertension attacks. Saudi Med J 29:122–125
Koch CA, Brouwers FM, Rosenblatt K et al (2003) Adrenal ganglioneuroma in a patient presenting with severe hypertension and diarrhea. Endocr Relat Cancer 10:99–107
Diab DL, Faiman C, Siperstein AE et al (2008) Virilizing adrenal ganglioneuroma in a woman with subclinical cushing syndrome. Endocr Pract 14:584–587
Maweja S, Materne R, Detrembleur N et al (2007) Adrenal ganglioneuroma. A neoplasia to exclude in patients with adrenal incidentaloma. Acta Chir Belg 107:670–674
Rha SE, Byun JY, Jung SE et al (2003) Neurogenic tumors in the abdomen: tumor types and imaging characteristics. Radiographics 23:29–43
Guo YK, Yang ZG, Li Y et al (2007) Uncommon adrenal masses: CT and MRI features with histopathologic correlation. Eur J Radiol 62:359–370
Bin X, Qing Y, Linhui W et al (2011) Adrenal incidentalomas: experience from a retrospective study in a Chinese population. Urol Oncol 29:270–274
Li L, Shao J, Gu J et al (2014) Adrenal ganglioneuromas: experience from a retrospective study in a Chinese population. Urol J 11:1485–1490
Zhang Y, Nishimura H, Kato S et al (2001) MRI of ganglioneuroma: histologic correlation study. J Comput Assist Tomogr 25:617–623
Metser U, Miller E, Lerman H et al (2006) 18F-FDG PET/CT in the evaluation of adrenal masses. J Nucl Med 47:32–37
Tessonnier L, Sebag F, Palazzo FF et al (2008) Does 18F-FDG PET/CT add diagnostic accuracy in incidentally identified non-secreting adrenal tumours? Eur J Nucl Med Mol Imaging 35:2018–2025
Katz RL, Shirkhoda A (1985) Diagnostic approach to incidental adrenal nodules in the cancer patient. Results of a clinical, radiologic, and fine-needle aspiration study. Cancer 55:1995–2000
Harisinghani MG, Maher MM, Hahn PF et al (2002) Predictive value of benign percutaneous adrenal biopsies in oncology patients. Clin Radiol 57:898–901
Paulsen SD, Nghiem HV, Korobkin M et al (2004) Changing role of imaging-guided percutaneous biopsy of adrenal masses: evaluation of 50 adrenal biopsies. AJR Am J Roentgenol 182:1033–1037
Hayashi Y, Iwato M, Hasegawa M et al (2001) Malignant transformation of a gangliocytoma/ganglioglioma into a glioblastoma multiforme: a molecular genetic analysis. J Neurosurg 95:138–142
Zografos GN, Kothonidis K, Ageli C et al (2007) Laparoscopic resection of large adrenal ganglioneuroma. JSLS 11:487–492
Marek-Safiejko M, Safiejko K, Łukaszewicz J et al (2016) A comparison of two approaches to laparoscopic adrenalectomy: lateral transperitoneal versus posterior retroperitoneal approach. Adv Clin Exp Med 25:829–835
Lairmore TC, Folek J, Govednik CM et al (2016) Improving minimally invasive adrenalectomy: selection of optimal approach and comparison of outcomes. World J Surg 40:1625–1631. https://doi.org/10.1007/s00268-016-3471-8
Vrielink OM, Wevers KP, Kist JW et al (2017) Laparoscopic anterior versus endoscopic posterior approach for adrenalectomy: a shift to a new golden standard? Langenbecks Arch Surg 402:767–773
Acknowledgements
This study was supported by funding from National Natural Science Foundation of China (No. 81572621).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Xie, J., Dai, J., Zhou, Wl. et al. Adrenal Ganglioneuroma: Features and Outcomes of 42 Cases in a Chinese Population. World J Surg 42, 2469–2475 (2018). https://doi.org/10.1007/s00268-018-4499-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4499-8