Abstract
Background
Postoperative inflammatory complications are associated with poorer prognosis in gastrointestinal malignancies. The aims of this study were to clarify the impact of postoperative inflammation itself on overall survival (OS) and relapse-free survival (RFS) in advanced gastric cancer patients.
Methods
We retrospectively analyzed 490 patients who underwent curative resection for pStage II and III gastric cancer from 2005 to 2008. We evaluated postoperative inflammation based on duration of hyperthermia (body temperature ≥38 °C) and leukocytosis (≥12,000/µL−1). OS and RFS were compared between a prolonged inflammation group and non-prolonged inflammation group. Multivariate analysis using the Cox proportional hazard model was performed to identify independent prognostic factors.
Results
The prolonged inflammation group comprised 57 (11.7%) patients who had hyperthermia for 4 days or longer and 42 (8.6%) patients who had leukocytosis for 7 days or longer. OS and RFS were significantly worse in the prolonged hyperthermia group (OS: hazard ratio (HR) 1.84, 95% confidence interval (CI) 1.19–2.73, P = 0.004; RFS: HR 1.66, 95% CI 1.08–2.45, P = 0.015). The prolonged leukocytosis group also showed significantly worse OS (HR 1.92, 95% CI 1.19–2.96, P = 0.004) and RFS (HR 1.90, 95% CI 1.19–2.88, P = 0.004). Multivariate analysis identified prolonged hyperthermia as an independent factor for predicting poor prognosis (OS: HR 1.77, 95% CI 1.13–2.68, P = 0.013; RFS: HR 1.60; 95% CI 1.03–2.39, P = 0.038).
Conclusions
Prolonged hyperthermia and leukocytosis after curative gastrectomy were associated with poorer OS and RFS in advanced gastric cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the third leading cause of cancer death in the world [1]. Surgical resection is the mainstay of treatment for gastric cancer, but recurrence and metastasis occur in 20–60% of patients [2,3,4]. We previously reported that postoperative complications impacted adversely on overall survival (OS) and disease-specific mortality (DSM) among 1395 patients who underwent curative resection for gastric cancer [5]. The cumulative incidence of DSM was also significantly worse in patients with complications. Multivariate analysis identified that an increased risk of complications significantly affected both OS and DSM [5]. In patients with colorectal cancer, some studies showed that postoperative complications involving intra-abdominal infection lead to higher levels of serum VEGF and IL-6 and a higher recurrence rate [6, 7].
The association between inflammatory status before surgery and prognosis can be defined using the Glasgow prognostic score (GPS) and neutrophil–lymphocyte ratio (NLR) [8,9,10]. Tokunaga et al. [11] reported postoperative intra-abdominal infectious complication is a prognostic factor for patients with gastric cancer. Inflammatory response seems to play an important role, but there are only few reports investigating association between postoperative inflammation itself and prognosis.
In this study, we hypothesized that an inflammatory response caused by postoperative complications could mediate a poor prognosis after curative resection for gastric cancer.
Materials and methods
Data source
From January 2005 to December 2008, 1418 patients with gastric cancer underwent curative gastrectomy at the Cancer Institute Hospital of Japanese Foundation for Cancer Research, Tokyo, Japan. Among them, 506 patients (35.7%) were diagnosed as pathological stage (pStage) II or III. We retrospectively reviewed their medical records. We excluded eight patients with synchronous cancer in other organs and three patients with rare histology (carcinosarcoma and neuroendocrine carcinoma). Five patients died during hospital stay after surgery, and they were excluded from this study. The remaining 490 patients constituted the entire cohort of this study. Gastrectomy and lymph node dissection were carried out according to the Japanese gastric cancer treatment guidelines [12]. Tumor was staged according to the 7th edition of the International Union Against Cancer tumor, node, metastasis (TNM) classification system [13]. In our institution, patients with clinical stage (cStage) I disease were treated with laparoscopic gastrectomy, while patients with cStage II and III were treated with open gastrectomy with D2 lymph node dissection. Patients were routinely given the epidural anesthesia during 3 days after surgery. Acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) were not used routinely. Patients with pathological stage (pStage) II or III disease, but not those with pT3N0 disease, received adjuvant chemotherapy based on a Japanese phase III trial for gastric cancer after 2007 [14]. Before the phase III trial, adjuvant chemotherapy using an oral fluorouracil agent was administered based on the surgeon’s choice. Information including patient characteristics, surgical records, and pathological data were obtained from the prospective database of our hospital. We defined the presence of postoperative complication as grade 2 or higher according to Clavien–Dindo classification [15].
Evaluation of inflammation
During the postoperative period, we usually perform blood examination on days 1, 3, and 7, with other days added if considered necessary by the attending surgeon. Body temperature (BT) was measured at least three times every day.
We evaluated inflammation with body temperature and white blood cell (WBC) count. Among variables of systemic inflammatory response syndrome (SIRS) criteria [16], we rated inflammation as present if the patient had a body temperature of 38 °C or higher or leukocytosis 12,000 µL−1 or higher. We counted the number of days with inflammation in each patient and set this as the inflammatory indicator of the patient. As for leukocytosis, we did not measure the white blood cell count every day; therefore, we rated it unless the WBC count went below 12,000 µL−1. If BT or the WBC count went below 38 °C or 12,000 µL−1 and these went up later, we rated the number of days with second inflammation and added to the number of the days with the first inflammation.
Statistical analysis
The primary interest of this study was to evaluate whether postoperative inflammation affects the following time-to-event end points: (1) OS, defined as the duration between the date of surgery and death from any cause or the date of last follow-up in living patients and (2) RFS, defined as the duration between the date of surgery and recurrence or the death due to any cause. Survival curves were evaluated by Kaplan–Meier method and the log-rank test was employed for comparisons.
Differences in patient characteristics as categorical variables were compared between the prolonged and non-prolonged hyperthermia groups by the Chi-square test. The Wilcoxon test was conducted for continuous variables. A Cox proportional hazards analysis was performed to identify independent prognostic factors among the variables for OS and RFS. In the analysis, each patient’s age, tumor location, perioperative blood transfusion, pathological stage, presence/absence of preoperative chemotherapy and adjuvant chemotherapy, duration of hyperthermia and leukocytosis were included as covariates.
Statistical analyses were carried out using JMP 11 (SAS institute, Cary, NC, USA). P values less than 0.05 were considered significant.
Results
Duration of inflammation and tumor recurrence
To determine cutoff values, we randomly divided 490 patients into two groups, a training set and validation set. We then identified those values of inflammatory indicators showing the highest hazard ratio for tumor recurrence in the training set and confirmed them using the validation set. Using this method, we defined prolonged hyperthermia group as duration of hyperthermia for 4 days or longer and prolonged leukocytosis as that lasting for 7 days or longer.
Patient characteristics
Table 1 summarizes the characteristics of 490 patients who underwent curative resection for pStage II and III gastric cancer. Of these, 57 (11.7%) patients had a maximum body temperature over 38 °C for 4 days or longer and thus were classified into the prolonged hyperthermia group, while 42 (8.6%) patients had leukocytosis for 7 days or longer and thus comprised the prolonged leukocytosis group. Twenty-four patients (4.9%) had both prolonged hyperthermia and leukocytosis. Usage of acetaminophen or NSAIDs did not differ significantly between prolonged and non-prolonged hyperthermia group (P = 0.689), and prolonged and non-prolonged leukocytosis group (P = 0.119). The prolonged hyperthermia group included significantly more male gender, longer operation time, large blood loss, total gastrectomy, tumor in the upper third of the stomach, splenectomy, presence of postoperative complications, and pStage III patients. A similar tendency was seen in the prolonged leukocytosis group, although more patients with deeper primary lesions. Duration of leukocytosis was significantly longer in open surgery group than laparoscopic surgery group (P < 0.001), but duration of hyperthermia did not significantly differ (P = 0.724). Of the 490 patients, 209 (42.7%) received adjuvant chemotherapy. Prolonged and non-prolonged hyperthermia group included 29 and 180 patients, and prolonged and non-prolonged leukocytosis group included 22 and 187 patients, respectively. Forty-two patients (8.6%) received preoperative chemotherapy, including 9 (15.8%) in the prolonged hyperthermia group and 33 (7.6%) in the non-prolonged hyperthermia group. Prolonged and non-prolonged leukocytosis group included 11 and 31 patients with preoperative chemotherapy.
Survival outcomes
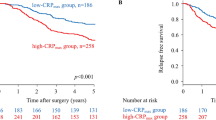
OS and RFS results are represented graphically in Figs. 1 and 2, respectively. The median follow-up time for the 490 patients was 61.8 months. One hundred and fifty-eight patients died during this period, and 132 had recurrence of gastric cancer. OS and RFS were both significantly worse in the prolonged hyperthermia group compared to the non-prolonged hyperthermia group (OS: hazard ratio (HR) 1.84, 95% confidence interval (CI) 1.19–2.73; Fig. 1a, RFS: HR 1.66, 95% CI 1.08–2.45; Fig. 1b). For pStage II disease, OS and RFS were not significantly different between the groups, However, for pStage III disease, both OS (HR 1.95, 95% CI 1.21–3.01) and RFS (HR 1.82, 95% CI 1.14–2.79) were significantly worse in the prolonged hyperthermia group than in the non-prolonged hyperthermia group. Similarly, the prolonged leukocytosis group showed significantly worse OS (HR 1.92, 95% CI 1.19–2.96; Fig. 2a) and RFS (HR 1.90, 95% CI 1.19–2.88; Fig. 2b) compared to the non-prolonged leukocytosis group. In pStage II disease, neither was significantly different between the prolonged and non-prolonged leukocytosis groups. On the other hand, for pStage III disease, the prolonged leukocytosis group showed significantly worse OS (HR 1.81, 95% CI 1.08–2.87) and RFS (HR 1.74, 95% CI 1.05–2.75) compared to the non-prolonged leukocytosis group.
Table 2 summarizes the multivariate analyses of prognostic factors for OS and RFS. Postoperative complication was excluded to investigate the effect of inflammatory response itself for prognosis and avoid multicollinearity, because postoperative complication was strongly associated with prolonged hyperthermia or leukocytosis from odds ratio of 6.08 between postoperative complication and prolonged hyperthermia, and that of 14.96 between postoperative complication and prolonged leukocytosis. By multivariate analysis, prolonged hyperthermia was independently associated with poor OS (HR 1.77; 95% CI 1.13–2.68) and RFS (HR 1.60; 95% CI 1.03–2.39). In contrast, multivariate analysis showed no statistically significant correlation between prolonged leukocytosis and OS or RFS.
Discussion
The present study showed that postoperative inflammation was associated with poor OS and RFS after curative resection for pStage III gastric cancer. We focused on pStage II and III gastric cancer patients in this study because those with pStage I disease show very low recurrence and mortality rates irrespective of postoperative inflammation and would not be suitable for comparing survival. Prolonged hyperthermia by our definition was an independent risk factor for poorer OS and RFS, while prolonged leukocytosis was also associated with poorer OS and RFS.
Postoperative inflammation has been suspected to affect oncological outcomes for malignancies. Intra-abdominal infectious complication after gastrectomy is associated with poor prognosis [11] and Nagasako et al. [17] reported an association between anastomotic complications and a higher recurrence rate for early gastric cancer. Our current study supports these previous data in suggesting that postoperative inflammation is associated with worse OS and RFS in patients with advanced gastric cancer.
Preoperative inflammation-based GPS and NLR before surgery has also been associated with tumor stage and aggressiveness, leading to poor prognosis in gastric cancer patients [8,9,10]. Further, we found here that even postoperative inflammation in terms of prolonged hyperthermia and leukocytosis after curative resection was associated with poorer OS and RFS. In this study, we could not investigate the relationship between preoperative GPS or NLR and prognosis because preoperative CRP or lymphocyte count was not measured in many cases during study period. Since hyperthermia and leukocytosis are included in the SIRS criteria and also related to the systemic inflammatory response, we evaluated postoperative inflammation based on these measures. Neutrophil or CRP is also indicator of inflammation, but it is difficult to set cutoff value. Additionally, CRP does not show present inflammation because CRP increases behind inflammation and decrease behind relief of inflammation. Inflammatory cytokines such as IL-6 and IL-10 are known to be associated with tumor growth [18, 19], and SIRS is followed by nine compensatory anti-inflammatory response syndrome (CARS) [20,21,22], with a Th1/Th2 balance shift toward Th2 and suppression of cellular immunity in the CARS phase [20, 23]. As SIRS is severe, the subsequently occurring CARS is inevitably also severe. Therefore, residual cancer cells might grow up in response to postoperative inflammatory cytokine activity and suppressed cellular immunity. More residual cancer cells would exist in pStage III gastric cancer patients than in those with pStage II disease; therefore, we speculate that they may proliferate even further in response to postoperative inflammation.
Overall, our multivariate analysis demonstrated that prolonged hyperthermia, age, blood transfusion pathological stage, tumor location, and preoperative chemotherapy were associated with poorer OS and RFS. Our study revealed prolonged postoperative inflammation could impact adversely on OS and RFS. Perioperative blood transfusion was also shown to cause immune dysfunction and malignant transformation of neoplastic cell [24], and such phenomena could contribute to the poor prognosis observed in this study. Preoperative chemotherapy might also be associated with more advanced disease at initial diagnosis, leading to poor OS and RFS.
The limitations of the present study include its retrospective nature, being conducted at a single institution, and the assessment of inflammation. We used body temperature and leukocytosis to decide presence of inflammation; however, these parameters are also affected by some drugs and the interval between measurements. Since we did not measure white blood cell count every day, duration of leukocytosis might not accurately reflect the severity of inflammation. Additionally, multicollinearity might exist between prolonged hyperthermia and leukocytosis, and measuring inflammatory cytokines could be more useful for assessing inflammation precisely. Our multivariate analysis also ruled out the impact of adjuvant chemotherapy as an independent prognostic factor; however, the indications and regimens of adjuvant chemotherapy were not established before the ACTS-GC trial started [14]. Therefore, it was not feasible to investigate the influence of adjuvant chemotherapy on recurrence or survival in association with postoperative inflammation in the present study.
In conclusion, postoperative prolonged hyperthermia and leukocytosis in terms of persistent inflammation were associated with poorer OS and RFS, specifically for pStage III gastric cancer patients.
References
Albert T (2012) GLOBOCAN database (World Health Organization web site). http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed 13 Dec 2015
Adachi Y, Oshiro T, Mori M et al (1996) Prediction of early and late recurrence after curative resection for gastric carcinoma. Cancer 77:2445–2448
Maehara Y, Hasuda S, Koga T et al (2000) Postoperative outcome and sites of recurrence in patients following curative resection of gastric cancer. Br J Surg 87:353–357
Rivera F, Vega-Villegas ME, Lopez-Brea MF (2007) Chemotherapy of advanced gastric cancer. Cancer Treat Rev 33:315–324
Kubota T, Hiki N, Sano T et al (2014) Prognostic significance of complications after curative surgery for gastric cancer. Ann Surg Oncol 21:891–898
Alonso S, Pascual M, Salvans S et al (2015) Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol 41:208–214
Salvans S, Mayol X, Alonso S et al (2014) Postoperative peritoneal infection enhances migration and invasion capacities of tumor cells in vitro: an insight into the association between anastomotic leak and recurrence after surgery for colorectal cancer. Ann Surg 260:939–943 (discussion 943–944)
Jiang X, Hiki N, Nunobe S et al (2012) Prognostic importance of the inflammation-based Glasgow prognostic score in patients with gastric cancer. Br J Cancer 107:275–279
Wang SC, Chou JF, Strong VE et al (2016) Pretreatment neutrophil to lymphocyte ratio independently predicts disease-specific survival in resectable gastroesophageal junction and gastric adenocarcinoma. Ann Surg 263:292–297
Mimatsu K, Oida T, Fukino N et al (2014) Glasgow prognostic score is a useful predictive factor of outcome after palliative gastrectomy for stage IV gastric cancer. Anticancer Res 34:3131–3136
Tokunaga M, Tanizawa Y, Bando E et al (2013) Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol 20:1575–1583
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Sobin LH, Gospodarowicz MK, Wittekind C (2010) International Union against cancer. In: Sobin LH, Gospodarowicz MK, Wittekind C (eds) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, Chichester
Sakuramoto S, Sasako M, Yamaguchi T et al (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357:1810–1820
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Nagasako Y, Satoh S, Isogaki J et al (2012) Impact of anastomotic complications on outcome after laparoscopic gastrectomy for early gastric cancer. Br J Surg 99:849–854
Kumagai K, Saikawa Y, Takeuchi H et al (2013) The neutrophil elastase inhibitor sivelestat suppresses accelerated gastrointestinal tumor growth via peritonitis after cecal ligation and puncture. Anticancer Res 33:3653–3659
Hiki N, Berger D, Prigl C et al (1998) Endotoxin binding and elimination by monocytes: secretion of soluble CD14 represents an inducible mechanism counteracting reduced expression of membrane CD14 in patients with sepsis and in a patient with paroxysmal nocturnal hemoglobinuria. Infect Immun 66:1135–1141
Kimura F, Shimizu H, Yoshidome H et al (2010) Immunosuppression following surgical and traumatic injury. Surg Today 40:793–808
Ni Choileain N, Redmond HP (2006) Cell response to surgery. Arch Surg 141:1132–1140
Moore FA, Moore EE (1995) Evolving concepts in the pathogenesis of postinjury multiple organ failure. Surg Clin N Am 75:257–277
Heidecke CD, Hensler T, Weighardt H et al (1999) Selective defects of T lymphocyte function in patients with lethal intraabdominal infection. Am J Surg 178:288–292
Sun C, Wang Y, Yao HS et al (2015) Allogeneic blood transfusion and the prognosis of gastric cancer patients: systematic review and meta-analysis. Int J Surg 13:102–110
Acknowledgements
We thank Dr. Naoki Ishizuka for his advice on statistics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okumura, Y., Hiki, N., Kumagai, K. et al. Postoperative Prolonged Inflammatory Response as a Poor Prognostic Factor After Curative Resection for Gastric Cancer. World J Surg 41, 2611–2618 (2017). https://doi.org/10.1007/s00268-017-4032-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4032-5