Abstract
Background
The Lancet Commission on Global Surgery (LCoGS) described the lack of access to safe, affordable, timely surgical, and anesthesia care. It proposed a series of 6 indicators to measure surgery, accompanied by time-bound targets and a template for national surgical planning. To date, no sub-Saharan African country has completed and published a nationwide evaluation of its surgical system within this framework.
Method
Mercy Ships, in partnership with Harvard Medical School and the Madagascar Ministry of Health, collected data on the 6 indicators from 22 referral hospitals in 16 out of 22 regions of Madagascar. Data collection was by semi-structured interviews with ministerial, medical, laboratory, pharmacy, and administrative representatives in each region. Microsimulation modeling was used to calculate values for financial indicators.
Results
In Madagascar, 29% of the population can access a surgical facility within 2 h. Surgical workforce density is 0.78 providers per 100,000 and annual surgical volume is 135–191 procedures per 100,000 with a perioperative mortality rate of 2.5–3.3%. Patients requiring surgery have a 77.4–86.3 and 78.8–95.1% risk of incurring impoverishing and catastrophic expenditure, respectively. Of the six LCoGS indicator targets, Madagascar meets one, the reporting of perioperative mortality rate.
Conclusion
Compared to the LCoGS targets, Madagascar has deficits in surgical access, workforce, volume, and the ability to offer financial risk protection to surgical patients. Its perioperative mortality rate, however, appears better than in comparable countries. The government is committed to improvement, and key stakeholder meetings to create a national surgical plan have begun.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thirty-two percent of the global disease burden requires surgical decision-making [1]. Yet, surgery remains the “neglected stepchild of global health” [2].
In April 2015, the Lancet Commission on Global Surgery (LCoGS) defined the scale of the problem: Five billion people lack access to safe, affordable surgical and anesthesia care [3]; 143 million additional procedures are needed every year [4]; 33 million individuals face catastrophic health expenditure every year due to payments for surgical and anesthesia services [5]; and lack of access to surgery causes losses in economic productivity estimated cumulatively at USD $12.3 trillion [6]. A set of six indicators, recommended targets, and a template for a national surgical plan were proposed to ensure surgery and anesthesia care become an integral part of each country’s health system [7].
The six indicators focus on preparedness (access to surgery and surgical workforce density); delivery (surgical volume and perioperative mortality rate); and financial risk (protection against impoverishing and catastrophic expenditures). Measuring the indicators allows a country to benchmark itself against the LCoGS targets and to develop a national surgical plan for improvement and ongoing monitoring of the indicators [7] (Table 1).
As part of a project to implement the World Health Organization (WHO) Surgical Safety Checklist in all the regional referral hospitals in Madagascar, Mercy Ships, an international non-governmental organization (NGO), in partnership with Harvard Medical School’s Program in Surgery and Social Change (PGSSC), collected data on the LCoGS’ six core indicators. Mercy Ships operates an 84-bed hospital ship which visits countries at the invitation of the President and works closely with the Ministry of Health to offer free surgeries, medical training, and quality improvement initiatives. From October 2014 until June 2016, Mercy Ships was docked in Madagascar. During this time, the LCoGS core indicators were used to assess the preparedness, delivery, and impact of surgical and anesthesia services in Madagascar, thereby providing data for the Ministry of Health to develop a national surgical plan. This paper describes the methodology, the evaluation of surgical services in Madagascar, and the start of a national surgical plan.
Materials and methods
Initial assessment and design
Initial assessment of the structure of Madagascar’s hospital system and educational needs occurred from October to December 2014, followed by data collection between September 2015 and April 2016, and by data analysis between April 2016 and June 2016. Assessment consisted of hospital surveys and interviews with key personnel, such as the Minister of Health; medical school deans; the World Health Organisation representative to Madagascar; various hospital directors and their chiefs of surgery, anesthesia, and nursing; and, where available, providers of surgically relevant services, such as radiology and biomedical engineering.
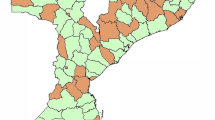
There are 22 regions in Madagascar, each with a regional referral hospital, which, in seven regions, is also a university hospital. The majority of surgery takes place in the regional referral hospitals, although some district hospitals provide cesarean section and minor operations, such as herniorrhaphy and appendectomy. Each Regional Minister of Health and hospital director received a letter from Mercy Ships and the Ministry of Health detailing dates when Mercy Ships would visit.
Data collection
Initial discussions with the Ministry of Health envisaged visits to 25 hospitals in 20 regions. However, due to pilot illness and flight schedule changes, 22 hospitals in 16 regions were ultimately visited, representing 17 hospitals outside the capital and 5 hospitals in the capital city. On arrival, courtesy visits were made to the offices of the Regional Minister of Health and the hospital director. These visits served to confirm receipt of Mercy Ships’ and Ministry of Health introductory communication and authorization, to describe the LCoGS data collection process, and to request permission of the hospital director to interview hospital staff. Data collection interviews took place with a combination of the following representatives, depending on availability: Regional Ministry of Health representatives; hospital directors; surgical, anesthesia, radiology, laboratory, and pharmacy staff; and other staff such as technical assistants, cashiers, and hospital statisticians.
All interviewees were adults over 18 years old who gave uncompensated, voluntary, verbal consent to participate. Confidential semi-structured interviews took place at the interviewee’s own hospital and were conducted in French by one of the authors (EB) with assistance from VR, HR where necessary. Interviews on LCoGS indicators lasted between 30 min and 3 h each. Each interviewee was interviewed once; however, on several occasions, follow-up emails and/or telephone calls were employed to clarify data where necessary. Responses were recorded contemporaneously in electronic records. All responses were de-identified and stored in a password-protected database accessible only to PGSSC and Mercy Ships representatives.
Initially, a semi-structured interview tool was created by Mercy Ships and designed to cover all aspects of the LCoGS six core surgical indicators. However, during the study, four of the authors (EB, SS, NR, and MS) became part of a PGSSC working group to create a standardized semi-structured interview tool. The PGSSC semi-structured interview tool (Appendix of ESM) was used for several stages of data collection and is now freely available in the public domain.
Definitions and analysis of the LCoGS six core indicators (Table 1)
The definition of each of the six indicators is given in Table 1.
In Madagascar, a “specialist” is defined as someone who had undergone 3 years of practice as a “generalist,” followed by an additional 4-year specialization.
With regard to Indicator 1, hospitals do not record the number of patients who travel more than 2 h to reach their facility; interviewees were asked to estimate this. We attempted to control for recall bias by conducting multiple interviews with a variety of hospital representatives.
No population census has been conducted since 1993; subnational population data were taken from the World Bank [8].We also lacked specific patient population and costing data from three of five hospitals visited in Antananarivo. To adjust for this, we calculated averages based on data available from the other hospitals visited in that city and used those figures in our subsequent analysis.
The costs of supplies and medications associated with a procedure were calculated based on those necessary for a caesarian section. Prior to June 2015, these supplies and medications (known as a “kit” in Madagascar) had been donated free of charge by the United Nations Population Fund. After June 2015, donations ceased, and hospitals began compiling their own kits and charging for them. Often these hospital-assembled kits are insufficient, necessitating that patients purchase a follow-on (“suivi”) kit. A Malagasy NGO created two standardized versions of a more complete kit for use, one for caesarian sections under general anesthesia and one under regional anesthesia. Cost calculations in this paper used these complete kits as a baseline.
To calculate values for Indicators 5 and 6, microsimulation modeling was used. Calculations were based on observed costs from three different regions of Madagascar of a pregnant woman in obstructed labor for 2 days living at least 40 km from the nearest surgical center. Costs were adjusted to international dollars (I$) using purchasing power parity converters available from the World Bank.
Impoverishing expenditure was defined as an expense that pushed a patient into or further into poverty (income below I$1.25/day) by out-of-pocket payments, adjusted for purchasing power parity [3]. Catastrophic expenditure was defined as an expense of at least 10% of an individual’s household income [9].
Timeline for national surgical plan
At the beginning of the study, the template for a national surgical plan was published, but the process was undefined. We planned preliminary discussions with the Ministry of Health for the mid-way point in December 2015, with the aim of defining future directions.
The study was approved by the Mercy Ships Institutional Review Board, Boston Children’s Hospital Institutional Review Board, and the Madagascar Ministry of Health.
Results
From September 2015 to April 2016, data were obtained from 22 out of 25 hospitals that were planned for assessment. Three hospitals were omitted due to aircraft schedule changes at short notice on account of weather and pilot illness. The 22 hospitals represent 16 regions (Table 2).
The average patient population among the surgical sites visited was 394,181 (range 1944–2,000,000). Surgical centers had on average 131 beds (range 42–600) and three operating rooms (range 1–12). The types of surgery performed at these facilities are given in Table 3.
In Madagascar, 29% of the population can access a surgical facility within 2 h. Specialist surgical workforce density is 0.78 per 100,000 population (Table 4), and the surgical volume is 163 (regional range 135–191) procedures per 100,000 population per year (Table 5). Madagascar’s POMR ranges between 2.5 and 3.3% at the regional hospitals.
Depending on the cost of surgery in each region, patients in Madagascar requiring surgery have between a 77.4% (95% CI 75.0–79.9%) and a 86.3% (95% CI 84.2–88.2%) chance of incurring impoverishing expenditure and between a 78.8% (95% CI 75.3–83.0%) and a 95.1% (95% CI 93.1–97.1%) chance of incurring catastrophic expenditure from the costs of surgery (Table 6).
Discussion
In this comprehensive assessment of surgical capacity in Madagascar, using the LCoGS six core indicators for monitoring universal access to safe, affordable surgical care, we find that Madagascar meets one out of six LCoGS targets, collecting POMR data. Scale-up of workforce and surgical volume, improving timely access to surgical care, and increasing financial risk protection for surgical patients are necessary to make progress toward achieving the other five targets. Madagascar’s post-operative mortality rate (POMR) appears better than those of some other LMICs [10, 11].
The overall workforce deficit and low surgical volume in Madagascar are similar to other LMICs [12–14]. In Madagascar, outside the capital city, only 5 of 17 regional centers surveyed could fix an open fracture, whereas all centers, both in the rural regions and in the capital, could undertake laparotomy and cesarean section.
Since 1975, China has helped supplement workforce numbers in Madagascar [15]. In two hospitals surveyed (Sambava and Ambovombe), all the surgeons, anesthesiologists, and obstetricians were Chinese, a situation that reportedly caused difficulties in communication and teamwork. Although many African countries have reported successful health partnerships with other nations [16–22], these can be time-consuming and expensive. The most efficient way to supplement surgical workforce remains unknown [23].
Prior assessments of surgical capacity in Madagascar have been limited to three areas: emergency care in one of 22 regions [24], financial implications of maternal and child health in one region [25], and pediatric surgical workforce density [26]. Our assessment covers a wider range of surgery in 16 of 22 regions, encompassing 73% of the national population. In our study, only 29% of the patients lived within 2 h of a surgical center, compared with 75% in the maternal and child health study, but similar to our study, the costs of medications and supplies constituted the majority of out-of-pocket expenses [25].
In most LMICs, patients face catastrophic expenditure to pay for surgery [5]. Madagascar is one of the world’s poorest countries, with annual income estimated at $440 USD [27]. To pay for surgery, patients sell portions of their livelihoods, such as cattle ($340–469 USD per head), parcels of land ($44–49 USD per square meter), or rice paddies ($521–625 USD). Madagascar currently lacks universal health coverage, but a type of insurance does exist for the very poor, known as the Fonds d’Equité. However, this is rarely used, primarily because of a culturally driven reluctance to self-identify, or to be publically identified, as “poor.” Our data, similar to Lin et al. [28], suggest that finance is one of the most important barriers to accessing surgical care.
POMR was the only indicator for which Madagascar met the LCoGS target. Madagascar is at the lower end of reported POMR in other countries [10, 11]. However, conclusive comparisons are hindered by lack of standardized definitions [29] and by the fact that surgeries are limited to healthier patients.
Our study has some limitations. Hospital data and costs were collected by face-to-face interview and not anonymously. This could have introduced positive and negative bias. Alternatively, a deliberately poor impression could have been given in the hope of receiving help. Population sizes were based on estimates, as no current census data exist, but we attempted to control for this by taking data from multiple interviewees and population data from the World Bank. Although we covered only 73% of regional hospitals, most surgery occurs in these regional centers; this is likely to be sufficiently representative. Despite its limitations, our study has a number of strengths. It is the first comprehensive assessment of surgical capacity in Madagascar. It serves as a “proof-of-concept” study on feasibility using the LCoGS indicators to benchmark a national surgical system. It also identifies key areas for improvement. Furthermore, the study illustrates how an NGO, an academic institution and a Ministry of Health, can collaborate for capacity assessments and strategic planning.
Assessments of surgical systems are useful only if data are made available to the government to be used in developing a plan for improvement and ongoing monitoring. The LCoGS template for a national surgical plan provides just that. At the time of writing, all data have been shared with the Malagasy Ministry of Health; a working party of surgical specialists has been created; support has been obtained from other NGOs, major stakeholders, and funders; and a preliminary planning forum is due to occur in September 2016.
In conclusion, we have evaluated the preparedness, delivery, and impact of surgical care in Madagascar; bench-marked the country against the LCoGS targets recommended to be achieved by the year 2030; and reported a “proof of concept” for this type of assessment in future countries. This process has revealed a deficit in Madagascar’s surgical system when compared to LCoGS targets, namely in the areas of timely access to surgical care, specialist surgical workforce, and surgical volume. Madagascar’s system is currently unable to offer financial risk protection to the majority of surgical patients. While much work remains to be done, initial signs are promising that the current government is committed to creating a national surgical plan to address the key areas of deficit—namely infrastructure, workforce, and service delivery.
References
Bickler SN, Weiser TG, Kassebaum N et al (2015) Global burden of surgical conditions. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (eds) Essential surgery: disease control priorities, vol 1, 3rd edn. The International Bank for Reconstruction and Development/The World Bank, Washington DC
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32(4):533–536. doi:10.1007/s00268-008-9525-9
Alkire BC, Raykar NP, Shrime MG et al (2015) Global access to surgical care: a modelling study. Lancet Glob health 3(6):e316–e323
Rose J, Weiser TG, Hider P et al (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health 3:S13–S20
Shrime MG, Dare AJ, Alkire BC et al (2015) Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob health 3(Suppl. 2):S38–S44
Alkire BC, Shrime MG, Dare AJ et al (2015) Global economic consequences of selected surgical diseases: a modelling study. Lancet Glob Health 3(Suppl. 2):S21–S27
Meara JG, Leather AJ, Hagander L et al (2015) Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624
World Bank. Subnational Population database World Bank 2014. http://databank.worldbank.org/data/reports.aspx?source=subnational-population
Xu K, Evans DB, Carrin G et al (2007) Protecting households from catastrophic health spending. Health Aff (Millwood) 26(4):972–983
Uribe-Leitz T, Jaramillo J, Maurer L et al (2016) Variability in mortality following caesarean delivery, appendectomy, and groin hernia repair in low-income and middle-income countries: a systematic review and analysis of published data. Lancet Glob health 4(3):e165–e174
The Global Surgery Collaborative (2016) Mortality of emergency abdominal surgery in high-, middle- and low-income countries. Br J Surg 103(8):971–988
Dubowitz G, Detlefs S, McQueen KA (2010) Global anesthesia workforce crisis: a preliminary survey revealing shortages contributing to undesirable outcomes and unsafe practices. World J Surg 34(3):438–444. doi:10.1007/s00268-009-0229-6
Hoyler M, Finlayson SR, McClain CD et al (2014) Shortage of doctors, shortage of data: a review of the global surgery, obstetrics, and anesthesia workforce literature. World J Surg 38(2):269–280. doi:10.1007/s00268-013-2324-y
McQueen K, Coonan T, Ottaway A et al (2015) The bare minimum: the reality of global anaesthesia and patient safety. World J Surg 39(9):2153–2160. doi:10.1007/s00268-015-3101-x
Madagascar awards medals to Chinese doctors. Peoples Daily Online 2010
Baird R, Poenaru D, Ganey M et al (2016) Partnership in fellowship: comparative analysis of pediatric surgical training and evaluation of a fellow exchange between Canada and Kenya. J Pediatr Surg. doi:10.1016/j.jpedsurg.2016.06.002
Chao TE, Riesel JN, Anderson GA et al (2015) Building a global surgery initiative through evaluation, collaboration, and training: the Massachusetts General Hospital experience. J Surg Educ 72(4):e21–e28
Monroe-Wise A, Kibore M, Kiarie J et al (2014) The clinical education partnership initiative: an innovative approach to global health education. BMC Med Educ 14:1043
Ndenga E, Uwizeye G, Thomson DR et al (2016) Assessing the twinning model in the Rwandan human resources for health program: goal setting, satisfaction and perceived skill transfer. Glob Health 12:4
Ulisubisya M, Jornvall H, Irestedt L et al (2016) Establishing an anaesthesia and intensive care partnership and aiming for national impact in Tanzania. Glob Health 12:7
Jones A (2016) Envisioning a global health partnership movement. Glob Health 12(1):1
Edwards S, Ritman D, Burn E et al (2015) Towards a simple typology of international health partnerships. Glob Health 11:49
Kelly E, Doyle V, Weakliam D et al (2015) A rapid evidence review on the effectiveness of institutional health partnerships. Glob Health 11:48
Kannan VC, Andriamalala CN, Reynolds TA (2015) The burden of acute disease in Mahajanga, Madagascar—a 21 month study. PLoS ONE 10(3):e0119029
Honda A, Randaoharison PG, Matsui M (2011) Affordability of emergency obstetric and neonatal care at public hospitals in Madagascar. Reprod Health Matters 19(37):10–20
Chirdan LB, Ameh EA, Abantanga FA et al (2010) Challenges of training and delivery of pediatric surgical services in Africa. J Pediatr Surg 45(3):610–618
World-Bank. Madagascar Country Profile. 2016. http://www.worldbank.org/en/country/madagascar
Lin BM, White M, Glover A, et al (2016) Barriers to surgical care and health outcomes: a prospective study on the relation between wealth, sex, and postoperative complications in the Republic of Congo. World J Surg. doi:10.1007/s00268-016-3676-x
Ng-Kamstra JS, Greenberg SL, Kotagal M et al (2015) Use and definitions of perioperative mortality rates in low-income and middle-income countries: a systematic review. Lancet 385(Suppl. 2):S29
Acknowledgements
E. Bruno received funding for International travel by Boston Children’s Hospital, Boston, MA, USA, and from the Mark Allen McConkey, M.D., Medical Student Public Service Fund. L. S. Baxter received a travel and education Grant from the National Institute for Academic Anaesthesia, UK. M. G. Shrime receives funding from the GE foundation for its Safe Surgery 2020 initiative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. C. White, V. A. Ravelojaona, H. N. Rakotoarison, H. H. Andriamanjato, K. L. Close, A. Herbert, N. Raykar and S. Saluja have no conflicts of interest to declare.
Additional information
Emily Bruno and Michelle C. White serve as the lead authors of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bruno, E., White, M.C., Baxter, L.S. et al. An Evaluation of Preparedness, Delivery and Impact of Surgical and Anesthesia Care in Madagascar: A Framework for a National Surgical Plan. World J Surg 41, 1218–1224 (2017). https://doi.org/10.1007/s00268-016-3847-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3847-9