Abstract
Background
The C-reactive protein to albumin (CRP/Alb) ratio, a novel inflammation-based prognostic score, is associated with outcomes in septic patients. The prognostic value of CRP/Alb ratio has not been established in cancer patients. The aim of this study is to evaluate the significance of CRP/Alb ratio in therapeutic outcome after pancreatic resection for pancreatic cancer.
Methods
The study comprised 113 patients who had undergone pancreatic resection for pancreatic cancer between April 2001 and December 2011. We retrospectively investigated the relation between CRP/Alb ratio and disease-free as well as overall survival.
Results
The optimal cut-off level of the CRP/Alb ratio was 0.03. For disease-free survival, preoperative biliary drainage (p = 0.011), advanced tumor-node-metastasis (TNM) classification (p = 0.002), and higher CRP/Alb ratio (p = 0.049) by univariate analysis, and advanced TNM classification (p = 0.003) by multivariate analysis, were independent and significant predictors of cancer recurrence. For overall survival, preoperative biliary drainage (p = 0.012), advanced TNM classification (p = 0.001), and higher CRP/Alb ratio (p = 0.023) by univariate analysis, and advanced TNM classification (p = 0.003) and higher CRP/Alb ratio (p = 0.035) by multivariate analysis, were independent and significant predictors of poor patient outcome.
Conclusions
The CRP/Alb ratio may be an independent and significant indicator of poor long-term outcomes in patients with pancreatic cancer after pancreatic resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is one of the most lethal and aggressive of all malignancies [1]. Despite the advances of preoperative diagnosis, operative techniques, and perioperative management, the 5-year survival rate after surgical resection still remains poor, which has been reported to range between 18 and 31.6 % [2, 3]. Several tumor-related factors have been reported to correlate with outcome after operation in patients with pancreatic cancer, including tumor stage, lymph node status, vascular invasion, perineural invasion, and resection margin status [3–5].
However, the evidences are increasing that the systemic inflammatory response, as patient-related factor, plays an important role in the progression of various type of malignancies [6, 7]. The preoperative systemic inflammation, represented by modified Glasgow prognostic score (mGPS), neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR), has been reported to predict cancer-specific survival of various cancer, including pancreatic cancer [5, 8–13]. It is widely known that the mGPS is based on circulating levels of two acute phase proteins, C-reactive protein (CRP) and albumin. The CRP to albumin (CRP/Alb) ratio, a novel inflammation based prognostic score also based on these two factors, was recently established to identify patients with serious illness on acute medical admission and reported to be associated with poor outcome in patients with sepsis [14, 15]. The prognostic value of the CRP/Alb ratio in cancer patients has been limited only in patients with hepatocellular carcinoma [16]. Therefore, in this study, we retrospectively investigated the relation between preoperative CRP/Alb ratio and disease-free as well as overall survival in patients with pancreatic cancer after pancreatic resection.
Patients and methods
Between April 2001 and December 2011, 123 patients with pancreatic cancer underwent pancreatic resection at the Department of Surgery, Jikei University Hospital, Tokyo, Japan. Of these, 10 patients were excluded, three patients for non-curative resection for liver metastasis, one patient for non-curative resection for positive ascites cytology, and 6 patients who were lost to follow-up, leaving the remaining 113 patients for this study.
We performed a retrospective review of a prospectively maintained database of patients who were histologically diagnosed as pancreatic cancer. Hemogram and chemistry profile were routinely measured for each patient preoperatively. Preoperative biliary drainage was performed when the patients developed obstructive jaundice and/or cholangitis.
The systemic inflammatory response was assessed using the modified GPS (mGPS) and CRP/Alb ratio. The mGPS was estimated as described previously [5, 8, 9]: patients with normal albumin (≥35 g/l) and normal CRP level (≤10 mg/l) as GPS 0, those with elevated CRP level (>10 mg/l) as GPS 1, and those with both low albumin (<35 g/l) and elevated CRP level (>10 mg/l) as GPS 2. CRP/Alb ratio was calculated by dividing the serum CRP level (mg/l) by serum albumin level (g/l). The type of pancreatic resection, pancreaticoduodenectomy (PD); distal pancreatectomy (DP); central pancreatectomy (CP); total pancreatectomy (TP), was selected based on tumor location and was classified into two groups: PD and non-PD. Tumor-node-metastasis (TNM) classification based on pathology was according to the General Rules for the Study of Pancreatic Cancer by the Japan Pancreas Society using the 6th editions of the TNM Classification System [17]. Postoperative complications were classified according to Clavien–Dindo classification [18].
At first, we investigated the relation between clinicopathologic variables and disease-free or overall survival after pancreatic resection by univariate and multivariate analyses. The following 10 variables were evaluated: age, gender, presence of preoperative biliary drainage, TNM classification based on pathology, type of resection, duration of operation, intraoperative blood loss, presence of postoperative complications classified as grade 3 or greater, mGPS, and CRP/Alb ratio. Clinicopathologic continuous variables were classified into 2 groups for the Log-rank test and the Cox proportional hazard regression model as follows: age <65 or ≥65 years, duration of operation <480 or ≥480 min, intraoperative blood loss <1000 or ≥1000 g, and CRP/Alb ratio <0.03 or ≥0.03.
Next, we investigated the relationship between clinicopathologic variables and CRP/Alb ratio by univariate analysis. The factor consisted of the following 9 factors: age, gender, presence of preoperative biliary drainage, TNM classification based on pathology, type of resection, duration of operation, intraoperative blood loss, presence of postoperative complications classified as grade 3 or greater, and mGPS.
Recurrence of pancreatic cancer was defined as newly detected local or distant metastatic tumors by ultrasonography, computed tomography or magnetic resonance image with or without increase in serum carcinoembryonic antigen or carbohydrate antigen 19–9.
This retrospective study was approved by the Ethics Committee of The Jikei University School of Medicine.
Statistical analysis
Data are expressed as a mean ± standard deviation (SD). Univariate analysis was performed using the Mann–Whitney U-test and Chi-square test. The optimal cut-off level of the CRP/Alb ratio was determined by a receiver operating characteristics (ROC) analysis. Univariate analysis of disease-free and overall survival was performed using the Log-rank test, and the Cox proportional regression model with backward elimination stepwise approach for multivariate analysis. All p values were considered statistically significant when the associated probability was less than 0.05. These analyses were conducted using IBM® SPSS statistics version 20.0 (IBM Japan, Tokyo, Japan).
Results
Patient characteristics
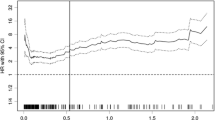
Patient characteristics are outlined in Table 1 as a mean ± SD, range, or ratio. Among the study population, the mean age was 66.8 years with a range 27 to 85 years, and 70 of them were male. Preoperative biliary drainage was performed in 43 of 113 patients (38.1 %). Patients with preoperative elevated CRP/Alb ratio were shown in 58 of 113 (51.3 %). Ninety-three patients are scored as mGPS 0, nine patients as mGPS 1, and one patient as mGPS 2. Postoperative complications developed in 58 of 113 patients (51.3 %), consisting of surgical site infection in 12 (10.6 %), pulmonary complications in 16 (14.2 %), and grade B or C postoperative pancreatic fistula in 20 patients (17.7 %). Of these, postoperative complication classified as Clavien–Dindo grade 3 or greater developed in 28 patients (24.8 %). In this study, the 5-year disease-free survival and overall survival rates after pancreatic resection for pancreatic cancer were 18.0 and 24.1 %, respectively. Applying ROC analysis to the survival status at the 3-year follow-up, the optimal cut-off level for the CRP/Alb ratio was 0.03, with the area under the curve was 0.638 (95 % CI 0.514–0.762, p = 0.028).
Univariate and multivariate analyses of clinicopathological variables in relation to disease-free survival after pancreatic resection for pancreatic cancer
Table 2 provides the relationship between the clinical variables and disease-free survival after pancreatic resection for pancreatic cancer. In univariate analysis, the disease-free survival was significantly worse in patients with the presence of preoperative biliary drainage (p = 0.011), pStage III or IV (p = 0.002), and CRP/Alb ratio ≥0.03 (p = 0.049, Fig. 1a). In multivariate analysis, pStage III or IV (p = 0.003) was the only independent and significant predictor of the disease-free survival.
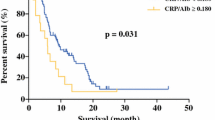
Univariate and multivariate analyses of clinicopathological variables in relation to overall survival after pancreatic resection for pancreatic cancer
Table 3 provides the relationship between the clinical variables and overall survival after pancreatic resection for pancreatic cancer. In univariate analysis, the overall survival was significantly worse in patients with the presence of preoperative biliary drainage (p = 0.012), pStage III or IV (p = 0.001), and CRP/Alb ratio ≥0.03 (p = 0.023, Fig. 1b). In multivariate analysis, pStage III or IV (p = 0.003) and CRP/Alb ratio ≥0.03 (p = 0.035) were independent and significant predictor of the overall survival. The patients with mGPS 1 or 2 tended to have worse disease-free survival, but not significantly (p = 0.091).
Association between clinicopathologic variables and CRP/Alb ratio
Table 4 provides the relationship between clinicopathologic variables and preoperative CRP/Alb ratio. In univariate analysis, advanced pTNM stage (p = 0.007) and higher mGPS (p < 0.001) were greater in high CRP/Alb ratio group.
Discussion
In this study, we found that the CRP/Alb ratio is an independent and significant risk factor for poor overall survival after pancreatic resection of pancreatic cancer. To the best of our knowledge, this is the first study to report the prognostic value of CRP/Alb ratio in patients with pancreatic cancer after pancreatic resection.
Recent reports advocate that the outcomes of patients with cancer were determined not only by tumor-related factors but also by patient-related factors. The presence of preoperative systemic response in the patient has been reported to predict poor survival after resection of various gastrointestinal cancers, including pancreatic cancer [5, 8–13]. Previous studies have suggested that mGPS represent potential prognostic markers in resected pancreatic cancer cases [5, 10]. In our study, advanced TNM classification as tumor-specific factor was associated with disease-free as well as overall survival, and the CRP/Alb ratio was an independent prognostic factor of poor survival in multivariate analysis. In contrast, mGPS was not an independent poor prognostic factor in multivariate analysis. These results suggested that predictive value of the CRP/Alb ratio was superior to mGPS because it could stratify the patient outcomes more strictly as it comprises continuous variables. Thus, the CRP/Alb ratio may reflect the potential inflammatory state. The CRP/Alb ratio was firstly reported to identify seriously ill patients on acute medical ward [14], and there were increasing evidence of this novel inflammation-based score in the field of patients with sepsis [15], hemodialysis [19], and cancer [16]. In these studies, the CRP/Alb ratio had also greater prognostic value than the existing inflammation-based scores, such as CRP alone, mGPS, and NLR.
The mechanism of the relation between the CRP/Alb ratio and cancer-specific survival in patients with cancer remains unclear. Elevated serum CRP level reflects a non-specific inflammatory response to tumor necrosis or local tissue damage and indicates a favorable environment for the establishment and growth of distant metastasis [20]. In this study, the patients with advanced TNM stage were more frequent in elevated CRP/Alb ratio group, which may reflect these factors. Moreover, serum CRP was reported to inhibit apoptosis of cancer cells in experimental study [21]. Serum level of vascular endothelial growth factor, an angiogenic factor, is increased in the presence of elevated serum CRP concentration [22]. Angiogenesis plays an important role in tumor growth and has been reported to be associated with poor outcome in patients with gastrointestinal tumors [23]. Furthermore, host immune response was associated with tumor growth. High-grade tumor inflammatory cell infiltrate was associated with low rate of recurrence and improved survival in pancreatic cancer [5], and elevated CRP concentration was related to a less infiltration of lymphocytes at the periphery of the tumor [24]. On the other hand, hypoalbuminemia is often observed in patients with advanced cancer and is usually regarded as a good index for malnutrition and cachexia. These conditions were induced by metabolic dysfunction resulting from complex crosstalk of inflammatory cytokines. Poor nutritional state had been reported to be associated with worse survival [25, 26]. Thus, the CRP/Alb ratio may associate with nutritional and/or septic status of patient. Perioperative nutritional support was recommended to improve the nutritional status in pancreatic surgery because there was a high prevalence of malnutrition in patients with pancreatic cancer [27]. Preoperative immunonutrition was reported to suppress the perioperative inflammatory response [28], and n-3 polyunsaturated fatty acids were also reported to have anti-inflammatory action in some clinical trials [29]. Further investigation to evaluate the relationship between immunonutrition and this inflammatory-based prognostic score is important to improve the management of patients with pancreatic cancer.
There are a few limitations to the present study. CRP is a non-specific marker of inflammation, and it is possible that the presence of other systemic disease could influence CRP concentrations. For the pancreatic head tumors, the associated clinical condition of jaundice or cholangitis may be a confounding factor in assessing CRP levels. However, in this study, hemogram and chemistry profile were measured just before operation for the assessment of CRP/Alb ratio after improvement of inflammation related to obstructive jaundice. Moreover, we evaluate this feature by including preoperative biliary drainage to the analyses, and the presence of preoperative biliary drainage was comparable in both CRP/Alb ratio groups. In summary, preoperative CRP/Alb ratio predicted prognostic outcome of patients with pancreatic cancer in overall survival after pancreatic resection. Risk stratification using CRP/Alb can be performed easily before surgery by preoperative hemogram and chemistry profile, which are a standard blood work for perioperative management. Routine preoperative CRP/Alb ratio measurement in patients undergoing curative treatment for pancreatic cancer would be useful for identifying patients with poorer prognosis and making clinical decisions.
Conclusion
The CRP/Alb ratio may be an independent and significant indicator of poor long-term outcomes in patients with pancreatic cancer after pancreatic resection.
References
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65:5–29
Okabayashi T, Shima Y, Iwata J et al (2014) S-1 vs. gemcitabine as an adjuvant therapy after surgical resection for ductal adenocarcinoma of the pancreas. World J Surg 38:2986–2993
Winter JM, Cameron JL, Campbell KA et al (2006) 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg 10:1199–1210
van Roest MH, Gouw AS, Peeters PM et al (2008) Results of pancreaticoduodenectomy in patients with periampullary adenocarcinoma: perineural growth more important prognostic factor than tumor localization. Ann Surg 248:97–103
Jamieson NB, Denley SM, Logue J et al (2011) A prospective comparison of the prognostic value of tumor- and patient-related factors in patients undergoing potentially curative surgery for pancreatic ductal adenocarcinoma. Ann Surg Oncol 18:2318–2328
Mantovani A, Allavena P, Sica A et al (2008) Cancer-related inflammation. Nature 454:436–444
Pagès F, Galon J, Dieu-Nosjean MC et al (2010) Immune infiltration in human tumors: a prognostic factor that should not be ignored. Oncogene 29:1093–1102
Proctor MJ, Morrison DS, Talwar D et al (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow inflammation outcome study. Eur J Cancer 47:2633–2641
McMillan DC (2008) An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc 67:257–262
La Torre M, Nigri G, Cavallini M et al (2012) The glasgow prognostic score as a predictor of survival in patients with potentially resectable pancreatic adenocarcinoma. Ann Surg Oncol 19:2917–2923
Paramanathan A, Saxena A, Morris DL (2014) A systematic review and meta-analysis on the impact of pre-operative neutrophil lymphocyte ratio on long term outcomes after curative intent resection of solid tumours. Surg Oncol 23:31–39
Stotz M, Gerger A, Eisner F et al (2013) Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br J Cancer 109:416–421
Shirai Y, Shiba H, Sakamoto T et al (2015) Preoperative platelet to lymphocyte ratio predicts outcome of patients with pancreatic ductal adenocarcinoma after pancreatic resection. Surgery 158:360–365
Fairclough E, Cairns E, Hamilton J et al (2009) Evaluation of a modified early warning system for acute medical admissions and comparison with C-reactive protein/albumin ratio as a predictor of patient outcome. Clin Med 9:30–33
Ranzani OT, Zampieri FG, Forte DN et al (2013) C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS ONE 8:e59321
Kinoshita A, Onoda H, Imai N et al (2015) The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol 22:803–810
Japan Pancreas Society (2009) General rules for the study of pancreatic cancer, 6th edn. Kanehara, Tokyo
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Hwang JC, Jiang MY, Lu YH et al (2015) Precedent fluctuation of serum hs-CRP to albumin ratios and mortality risk of clinically stable hemodialysis patients. PLoS One 10:e0120266
Wong VK, Malik HZ, Hamady ZZ et al (2007) C-reactive protein as a predictor of prognosis following curative resection for colorectal liver metastases. Br J Cancer 96:222–225
Yang J, Wezeman M, Zhang X et al (2007) Human C-reactive protein binds activating Fcgamma receptors and protects myeloma tumor cells from apoptosis. Cancer Cell 12:252–265
Xavier P, Belo L, Beires J et al (2006) Serum levels of VEGF and TNF-alpha and their association with C-reactive protein in patients with endometriosis. Arch Gynecol Obstet 273:227–231
Fondevila C, Metges JP, Fuster J et al (2004) p53 and VEGF expression are independent predictors of tumour recurrence and survival following curative resection of gastric cancer. Br J Cancer 90:206–215
Canna K, McArdle PA, McMillan DC et al (2005) The relationship between tumour T-lymphocyte infiltration, the systemic inflammatory response and survival in patients undergoing curative resection for colorectal cancer. Br J Cancer 92:651–654
Kanda M, Fujii T, Kodera Y et al (2011) Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg 98:268–274
Okumura S, Kaido T, Hamaguchi Y et al (2015) Impact of preoperative quality as well as quantity of skeletal muscle on survival after resection of pancreatic cancer. Surgery 157:1088–1098
Bozzetti F, Mariani L (2014) Perioperative nutritional support of patients undergoing pancreatic surgery in the age of ERAS. Nutrition 30:1267–1271
Giger U, Büchler M, Farhadi J et al (2007) Preoperative immunonutrition suppresses perioperative inflammatory response in patients with major abdominal surgery-a randomized controlled pilot study. Ann Surg Oncol 14:2798–2806
Mocellin MC, Camargo CQ, Nunes EA et al (2015) A systematic review and meta-analysis of the n-3 polyunsaturated fatty acids effects on inflammatory markers in colorectal cancer. Clin Nutr. doi:10.1016/j.clnu.2015.04.013
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Haruki, K., Shiba, H., Shirai, Y. et al. The C-reactive Protein to Albumin Ratio Predicts Long-Term Outcomes in Patients with Pancreatic Cancer After Pancreatic Resection. World J Surg 40, 2254–2260 (2016). https://doi.org/10.1007/s00268-016-3491-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3491-4