Abstract
Background
Postoperative liver failure (PHLF) is one of the most common complications following major hepatectomy. The preoperative assessment of future liver remnant (FLR) function is critical to predict the incidence of PHLF.
Objective
To determine the efficacy of the plasma clearance rate of indocyanine green clearance of FLR (ICGK-F) in predicting PHLF in cases of highly invasive hepatectomy with extrahepatic bile duct resection.
Methods
Five hundred and eighty-five patients who underwent major hepatectomy with extrahepatic bile duct resection, from 2002 to 2014 in a single institution, were evaluated. Among them, 192 patients (33 %) had PHLF. The predictive value of ICGK-F for PHLF was determined and compared with other risk factors for PHLF.
Results
The incidence of PHLF was inversely proportional to the level of ICGK-F. With multivariate logistic regression analysis, ICGK-F, combined pancreatoduodenectomy, the operation time, and blood loss were identified as independent risk factors of PHLF. The risk of PHLF increased according to the decrement of ICGK-F (the odds ratio of ICGK-F for each decrement of 0.01 was 1.22; 95 % confidence interval 1.12–1.33; P < 0.001). Low ICGK-F was also identified as an independent risk factor predicting the postoperative mortality.
Conclusions
ICGK-F is useful in predicting the PHLF and mortality in patients undergoing major hepatectomy with extrahepatic bile duct resection. This criterion may be useful for highly invasive hepatectomy, such as that with extrahepatic bile duct resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with perihilar cholangiocarcinoma, extended hepatectomies with resection of the caudate lobe and extrahepatic bile duct are often necessary to obtain negative surgical margins and offer better survival outcomes [1, 2]. This procedure is associated with the highest mortality in liver surgery even in high-volume centers [3]. When future liver remnant (FLR) function is insufficient, preoperative portal vein embolization (PVE) is recommended to increase the FLR volume [4]. In addition, biliary drainage is a mandatory procedure to normalize the liver function affected by partial or total biliary tree obstruction. Moreover, due to the anatomical proximity of portal triads, combined resection of the portal vein and/or hepatic artery, in combination with the extrahepatic bile duct, is sometimes necessary due to cancer invasion into these structures. For these reasons, the surgeries for perihilar cholangiocarcinoma are different from those for hepatocellular carcinoma or metastatic liver tumors, in which extrahepatic bile duct resection is not usually necessary. Therefore, an accurate preoperative evaluation of the FLR function is critical for improving the surgical outcome following major hepatectomy with extrahepatic bile duct resection.
The liver function of the FLR should be assessed according to the volume and function. We used the plasma disappearance rate of indocyanine green clearance of the FLR (ICGK-F), which is calculated by combining the data from CT volumetry (for the FLR volume) and indocyanine green (ICG) clearance tests (for the function). For instance, in patients with ICGK value 0.180 (normal range 0.150–0.200) and who are going to undergo 70 % hepatectomy, ICGK-F is equal to 0.054 (=0.180 × 0.30). Nagino et al. previously reported that the patients with ICGK-F less than 0.05 have a significantly higher mortality rate than patients who undergo major hepatectomy with extrahepatic bile duct resection following portal vein embolization (PVE) [4]. Moreover, Yokoyama et al. retrospectively analyzed 274 patients who underwent right hepatectomy, right trisectionectomy, or left trisectionectomy for biliary cancer between 1991 and 2008 [5]. In multiple logistic regression analyses, an ICGK-F less than 0.05 had a significant impact on the incidence of postoperative mortality. Therefore, we have been using a cut-off value of 0.05 for ICGK-F to determine the operative indication for major hepatectomy with extrahepatic bile duct resection.
With the advancement of recent perioperative patient management, the morbidity and mortality rates in major hepatectomy for perihilar cholangiocarcinoma have dramatically improved, especially after 2001 [6]. Therefore, it is necessary to reassess the value of ICGK-F in predicting morbidity and mortality among recent cases. The aim of this study was to determine the efficacy of ICGK-F in predicting posthepatectomy liver failure (PHLF) and mortality in recent surgical cases (from 2002 to present) of perihilar cholangiocarcinoma.
Patients and methods
Study population
From January 2002 to February 2014, a total of 592 patients underwent a major hepatectomy with extrahepatic bile duct resection for perihilar cholangiocarcinoma at the First Department of Surgery, Nagoya University Hospital in Nagoya, Japan. Excluding 4 patients who did not undergo an ICG test or CT volumetry and 3 patients with ICG excretory defect, a total of 585 patients were evaluated. Major hepatectomy in this study included the resection of three or more Couinaud segments as well as caudate lobectomy with extrahepatic bile duct resection. One hundred and seventy-six patients who underwent surgery between January 2002 and December 2008 overlapped with a previous study [5]. Written informed consent for participation was obtained from each patient before study enrollment, which was approved by the Nagoya University Hospital Human Research Review Committee.
Preoperative patient management
When the observed patients had jaundice, an appropriate biliary drainage, either by endoscopic nasobiliary drainage, an endoscopic biliary stent, or percutaneous transhepatic biliary drainage, was performed. If the total serum bilirubin level was more than 2.0 mg/dl, an additional drainage for the obstructed biliary branch was performed and the operation was postponed until the total serum bilirubin level went down under 2.0 mg/dl. ICG test was also not performed when the total serum bilirubin level was more than 2.0 mg/dl. For ICG clearance tests, ICG (0.5 mg per kg bodyweight) was administered through a peripheral vein, and venous blood was sampled before and 5, 10, and 15 min after injection. Specimens were analyzed for ICG concentrations on a spectrophotometer at 805 nm. The plasma disappearance rate of ICG (ICGK) was calculated by linear regression analysis of plasma ICG concentration as previously described [5, 7].
As an institutional strategy, when the liver parenchyma resection rate exceeded 60 % or when the ICGK-F was below 0.05, a PVE was performed to increase the FLR volume [4, 8]. PVEs were performed using an ipsilateral approach, as previously described [9, 10]. Microcoils and 100 % ethanol were used as the embolic materials. CT scans and ICG clearance tests were performed 2–3 weeks after the PVE to calculate the ICGK-F. In general, excluding several exceptional cases, when the ICGK-F value did not fulfill the institutional criteria (≥0.05), the scheduled surgery was postponed. Thereafter, the CT volumetry and ICG tests were repeatedly evaluated every 4 weeks until the ICGK-F reached the institutional criteria level. When the ICGK-F was below 0.05, even after a long waiting period, surgery was performed only if the patient had a strong desire to undergo resection and the appropriate informed consent had been obtained.
Recording of the clinical data and postoperative complications
Detailed daily clinical records were kept for all patients. PHLF and posthepatectomy bile leakage were defined according to the criteria of the International Study Group of Liver Surgery (ISGLS) [11, 12]. Postoperative infectious complications, including pneumonia, surgical site infections (SSI), and bacteremia, as detected by the culture method, were also recorded for up to 30 days after surgery. The diagnosis of pneumonia required radiological evidence of consolidation with leukocytosis. SSI included superficial/deep incisional infections and organ space infections [13]. Bacteremia was diagnosed when a blood culture grew an isolate of organisms, with no contamination of the skin flora. Clinically significant ascites or pleural effusion requiring drainage was also recorded.
Statistical analyses
The data were analyzed using the Windows versions of JMP, version 8 (SAS Institute Inc., Cary, NC), or Dr. SPSS II, version 11.01 J (SPSS Inc., Chicago, IL). The results were expressed as the median (range). Continuous data were compared between the two groups using Student’s t test. When data were not normally distributed, univariate analysis was performed using a non-parametric test. Categorical data were compared using the χ2 test or Fisher’s exact test, as appropriate. Multiple logistic regression analysis was used to examine the relationship between PHLF or mortality and perioperative variables. The prognostic value of the plasma clearance rate of ICG (ICGK), the proportion of the FLR, and ICGK-F for predicting PHLF was assessed using receiver operating characteristic (ROC) curve analysis, and the areas under the curve (AUCs) among these factors were compared. A result was considered statistically significant when the P value was less than 0.05.
Results
Type of surgery and ICGK-F value
Sixty-one per cent of patients (n = 353) underwent preoperative PVE to increase the FLR volume. In 308 patients, ICG test was performed before and after PVE. There was no significant difference in the value of ICGK before (median 0.160; range 0.096–0.266) and after (median 0.161; range 0.098–0.261) PVE. The volume of the FLR was increased after PVE and, as a result, ICGK-F values after PVE (median 0.069; range 0.031–0.149) increased significantly compared to the values before PVE (medina 0.054; range 0.023–0.128) (P < 0.001).
The type of hepatectomies and the number of patients with different levels of ICGK-F are shown in Fig. 1a. Right hepatectomy was performed in 196 patients (34 %), left hepatectomy in 185 patients (32 %), left trisectionectomy in 148 patients (25 %), right trisectionectomy in 45 patients (8 %), and central bisegmentectomy in 11 patients (2 %). All of the patients, excluding 5 unnecessary cases, underwent caudate lobectomy. Among 585 patients, combined pancreatoduodenectomy was performed in 87 patients (15 %). Combined portal vein resection was performed in 210 patients (36 %) and hepatic artery resection in 121 patients (21 %).
a Type of hepatectomies and the number of patients with different ICGK-F levels. RH right hepatectomy, LH left hepatectomy, LT left trisectionectomy, RT right trisectionectomy, CB central bisegmentectomy. b Incidence rate of PHLF (grade B or C determined by the ISGLS) in the different levels of ICGK-F. c Surgery-related mortality rate for different levels of ICGK-F
A total of 192 patients (33 %) developed grade B (n = 164) or C (n = 28) PHLF according the ISGLS. The incidence rate of PHLF was roughly proportional to the decrement of the ICGK-F value (Fig. 1b). More than 50 % of patients developed PHLF when the ICGK-F value was less than or equal to 0.05. There were 12 patients (2.1 %) with surgery-related death. The mortality rate was significantly higher for 39 patients with ICGK-F less than or equal to 0.05 compared to patients with ICGK-F more than 0.05 (7.7 % vs. 1.7 %, P = 0.010) (Fig. 1c). Notably, no mortality was observed among patients with ICGK-F more than 0.08.
Preoperative factors associated with PHLF
The preoperative factors were compared between the patients with grade B or C PHLF (PHLF group, n = 192) and others (non-PHLF group, n = 393) (Table 1). The proportion of male patients was significantly higher in the PHLF group compared to the non-PHLF group (73 % vs. 59 %, P < 0.001). The serum total bilirubin (T-Bil) on admission and the proportion of the patients with cholangitis were significantly higher in the PHLF group. Preoperative biliary drainage was performed in 498 patients (85 %), and the proportion of patients with biliary drainage was higher in the PHLF group. ICGK, the proportion of FLR, and ICGK-F were all significantly lower in the PHLF group compared to the non-PHLF group.
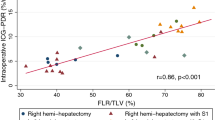
The area under the ROC curve in predicting PHLF in the factors of ICGK (index of function), the proportion of FLR (index of volume), and ICGK-F (index of function × volume) were 0.573, 0.641, and 0.670, respectively (Fig. 2). The AUC was significantly greater in the ICGK-F compared to that in the ICGK (P < 0.001).
Intraoperative factors associated with PHLF
More patients underwent right hepatectomy and fewer patients underwent left hepatectomy in the PHLF group compared to the non-PHLF group. The overall incidence rate of PHLF was 43 % in right hepatectomy, 16 % in left hepatectomy, 40 % in left trisectionectomy, 33 % in right trisectionectomy, and 46 % in central bisegmentectomy. Combined portal vein resection or pancreatoduodenectomy was more frequently performed in the PHLF group compared to the non-PHLF group (Table 2). The operation time and intraoperative blood loss were significantly higher in the PHLF group than in the non-PHLF group.
Postoperative courses and PHLF
There were 12 patients who died after surgery (Table 3). All patients with surgery-related death were with PHLF and infectious complications. Six out of 12 patients underwent re-operation due to postoperative portal vein thrombosis (n = 4), intestinal perforation (n = 2), and intra-abdominal bleeding (n = 1). The mean postoperative hospital length of stay and complication rates were significantly greater in the PHLF group compared to the non-PHLF group.
Factors associated with PHLF
The various preoperative and intraoperative factors associated with the incidence of PHLF were included in the multivariate logistic regression analyses. The analyzed risk factors included gender, preoperative cholangitis, preoperative biliary drainage, ICGK-F, combined pancreatoduodenectomy, combined portal vein resection, operation time, and blood loss (Table 4). A low ICGK-F value, combined pancreatoduodenectomy, long operation time, and great blood loss were identified as independent risk factors for PHLF. The odds ratio for each 0.01 decrement in ICGK-F was 1.22 (95 % confidential interval 1.12–1.33, P < 0.001). This odds ratio was similar to the levels of each increment of 1 h operation time (odds ratio 1.18) and each increment of 250 ml blood loss (odds ratio 1.20).
Factors associated with the postoperative mortality
Regarding the surgical procedure, there was no patient who died after surgery in left hepatectomy. Excluding central bisegmentectomy with small number of patients (n = 11), the mortality rate was not significantly different among other procedures such as right hepatectomy (3.1 %), left trisectionectomy (2.7 %), and right trisectionectomy (2.2 %). Among the various preoperative and intraoperative factors, ICGK-F, the operation time, and blood loss were significantly different between the patients who died after surgery and those who did not according to univariate analysis (data not shown). The multivariate logistic regression analyses revealed that the low ICGK-F and long operation time were independent risk factors for postoperative mortality (Table 5).
Discussion
Insufficient remnant liver function is a major problem following extended hepatectomy. PHLF frequently occurs after major hepatectomy, and this complication sometimes has a fatal postoperative outcome. Therefore, before performing major hepatectomies, it is crucial to accurately evaluate the FLR function and predict the risk of PHLF. The functional reserve of the FLR should be evaluated by both the remnant liver volume and remnant liver function. The volume can be evaluated by the CT volumetry, whereas the function can be evaluated by the ICG clearance test, asialoglycoprotein receptor scintigraphy with 99mTc-galactosyl human serum albumin [14], and other tests [15, 16]. We have been using ICGK-F, which combines the value of CT volumetry and the ICG clearance test, for more than 20 years as a useful criterion for evaluating FLR function [4, 5]. Patients with perihilar cholangiocarcinoma always accompany biliary stenosis. For these patients, ICG test may be more suitable than other liver function assessment methods because the results of ICG test sensitively reflect the condition of biliary obstruction and biliary excretory function. ICGK-F of more than 0.05 has been considered a safety margin because in a previous study the patients with ICGK-F less than 0.05 had a significantly higher rate of postoperative mortality than those who did not [5]. In this study, by only including recent cases (after 2001), we sought to re-evaluate and validate the value of ICGK-F as a predictor of PHLF and postoperative mortality in selected cases of major hepatectomy with extrahepatic bile duct resection for perihilar cholangiocarcinoma.
When the patients were categorized into groups with and without PHLF, gender and the presence of preoperative cholangitis had significant differences between the two groups (Table 1). These variables were already reported as detrimental factors in hepatectomy. A clinical study by Imamura et al. [17] and Yokoyama et al. [18] showed that male sex was a negative factor for the hepatic regeneration rate following PVE. Regarding cholangitis, a previous study showed that the presence of preoperative cholangitis has a negative impact on the postoperative maximum total serum bilirubin levels, morbidity rate, and postoperative hospital stay [19]. In addition to the aforementioned risk factors, the value of ICGK-F was significantly lower in the PHLF group than in the non-PHLF group (Table 1). This study also demonstrated that the risk of PHLF was inversely correlated with the level of ICGK-F (Fig. 1b). In patients with ICGK-F less than 0.05, more than half developed PHLF. In contrast, in patients with ICGK-F of more than 0.120, the incidence rate of PHLF was less than 20 %. These results indicated that the ICGK-F could be a useful indicator in predicting the risk of PHLF.
Assessment of an accurate FLR volume before surgery is mandatory because the volume in each segment is highly variable among patients [20]. Shirabe et al. reported that the remnant liver volume of patients who died of liver failure after right hepatectomy was significantly smaller than that of patients who survived [21]. In addition to the data for the FLR volume, qualitative tests for liver function are important for assessing the FLR functional reserve because the metabolic function of the liver is not always linearly proportional to the liver volume. Among the various qualitative tests for liver function, ICG clearance is considered the most powerful predictor of posthepatectomy mortality [22–24]. Nonami et al. reported that the low ICGK value is one of the independent risk factors for postoperative mortality [23]. Therefore, it is reasonable to combine the data of CT volumetry and ICG testing to assess the risk of major hepatectomy. However, only a few reports have analyzed the combined data of CT volumetry and ICG testing [25, 26]. According to the ROC curve analysis for predicting PHLF, the area under the curve was higher than either ICGK or the proportion of the FLR, and it was significantly different between the ICGK and ICGK-F, indicating that the ICGK-F is a superior predictor to ICGK (Fig. 2). We have been using ICGK-F as a criterion to assess the operability, especially for cases of severe major hepatectomy with extrahepatic bile duct resection. The mortality rate was 1.7 % in patients with ICGK-F more than 0.05. This level of mortality is acceptable in a major hepatectomy with extrahepatic bile duct resection, which is the most technically difficult liver resection. One may suggest to increase the cut-off value of ICGK-F to 0.08 to further decrease the incidence of mortality (no surgery-related death with ICGK-F > 0.08). However, it is ethically unacceptable because approximately one-third of patients in this cohort were with ICGK-F 0.05–0.08.
The ICG test is simple, cost effective, and repeatable with minimum invasiveness. However, there are some patients with constitutional ICG excretory defect [27] and thus the ICGK-F criterion is not applicable for such patients. Liver function was assessed by an alternative method such as 99mTc-galactosylated serum albumin scintigraphy for these patients. Nevertheless, the number of the patients with ICG excretory defect in this study was very low (n = 3/592, 0.5 %). Additionally, few patients had an allergic response to ICG. Therefore, the ICG test can be safely applied to the general patient population without major complications.
It should be noted that the analysis in this study was retrospective, although the data used for the analysis were prospectively collected. The mean operation time and intraoperative blood loss were different between the PHLF and non-PHLF groups. These factors may affect the postoperative incidence of PHLF; therefore, it may be difficult to independently assess the predictive value of ICGK-F for PHLF. However, we found that the ICGK-F was an independent risk factor for PHLF with multivariate logistic regression analyses. The odds ratio for the risk of PHLF in each 0.01 decrement in ICGK-F was 1.22, which was similar to that for the 1-h increment in operation time (odds ratio; 1.18) and 250-ml increment in intraoperative blood loss (odds ratio; 1.20) (Table 4).
In conclusion, this study demonstrated that the ICGK-F was a useful indicator for predicting PHLF. The level of ICGK-F was inversely correlated to the incidence of PHLF. ICGK-F should be used to determine the operative indication and in selecting high-risk patients for PHLF or postoperative mortality among patients who plan to undergo major hepatectomy with extrahepatic bile duct resection.
References
Natsume S, Ebata T, Yokoyama Y et al (2012) Clinical significance of left trisectionectomy for perihilar cholangiocarcinoma: an appraisal and comparison with left hepatectomy. Ann Surg 255:754–762
Nagino M, Kamiya J, Arai T et al (2006) “Anatomic” right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg 243:28–32
Ebata T, Kosuge T, Hirano S et al (2014) Proposal to modify the international union against cancer staging system for perihilar cholangiocarcinomas. Br J Surg 101:79–88
Nagino M, Kamiya J, Nishio H et al (2006) Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg 243:364–372
Yokoyama Y, Nishio H, Ebata T et al (2010) Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg 97:1260–1268
Igami T, Nishio H, Ebata T et al (2010) Surgical treatment of hilar cholangiocarcinoma in the “new era”: the Nagoya University experience. J Hepatobiliary Pancreat Sci 17:449–454
Uesaka K, Nimura Y, Nagino M (1996) Changes in hepatic lobar function after right portal vein embolization. An appraisal by biliary indocyanine green excretion. Ann Surg 223:77–83
Ebata T, Yokoyama Y, Igami T et al (2012) Portal vein embolization before extended hepatectomy for biliary cancer: current technique and review of 494 consecutive embolizations. Dig Surg 29:23–29
Nagino M, Nimura Y, Kamiya J et al (1995) Right or left trisegment portal vein embolization before hepatic trisegmentectomy for hilar bile duct carcinoma. Surgery 117:677–681
Nagino M, Nimura Y, Kamiya J et al (1996) Selective percutaneous transhepatic embolization of the portal vein in preparation for extensive liver resection: the ipsilateral approach. Radiology 200:559–563
Rahbari NN, Garden OJ, Padbury R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
Rahbari NN, Reissfelder C, Koch M et al (2011) The predictive value of postoperative clinical risk scores for outcome after hepatic resection: a validation analysis in 807 patients. Ann Surg Oncol 18:3640–3649
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27:97–132; quiz 133–134; discussion 196
Kokudo N, Vera DR, Tada K et al (2002) Predictors of successful hepatic resection: prognostic usefulness of hepatic asialoglycoprotein receptor analysis. World J Surg 26:1342–1347
Nanashima A, Yamaguchi H, Shibasaki S et al (2001) Measurement of serum hyaluronic acid level during the perioperative period of liver resection for evaluation of functional liver reserve. J Gastroenterol Hepatol 16:1158–1163
Lee SG, Hwang S (2005) How I do it: assessment of hepatic functional reserve for indication of hepatic resection. J Hepatobiliary Pancreat Surg 12:38–43
Imamura H, Shimada R, Kubota M et al (1999) Preoperative portal vein embolization: an audit of 84 patients. Hepatology 29:1099–1105
Yokoyama Y, Nagino M, Oda K et al (2008) Sex dimorphism in the outcome of preoperative right portal vein embolization. Arch Surg 143:254–259; discussion 259
Yokoyama Y, Ebata T, Igami T et al (2014) The adverse effects of preoperative cholangitis on the outcome of portal vein embolization and subsequent major hepatectomies. Surgery
Abdalla EK, Denys A, Chevalier P et al (2004) Total and segmental liver volume variations: implications for liver surgery. Surgery 135:404–410
Shirabe K, Shimada M, Gion T et al (1999) Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg 188:304–309
Guglielmi A, Ruzzenente A, Conci S et al (2012) How much remnant is enough in liver resection? Dig Surg 29:6–17
Nonami T, Nakao A, Kurokawa T et al (1999) Blood loss and ICG clearance as best prognostic markers of post-hepatectomy liver failure. Hepatogastroenterology 46:1669–1672
Hemming AW, Scudamore CH, Shackleton CR et al (1992) Indocyanine green clearance as a predictor of successful hepatic resection in cirrhotic patients. Am J Surg 163:515–518
Kasai Y, Hatano E, Iguchi K et al (2013) Prediction of the remnant liver hypertrophy ratio after preoperative portal vein embolization. Eur Surg Res 51:129–137
Ohkura Y, Mizuno S, Kishiwada M et al (2014) Benefit of technetium-99 m galactosyl human serum albumin scintigraphy instead of indocyanine green test in patients scheduled for hepatectomy. Hepatol Res 44:E118–128
Hwang S, Ha TY, Song GW et al (2015) Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg 19:1305–1314
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yokoyama, Y., Ebata, T., Igami, T. et al. The Predictive Value of Indocyanine Green Clearance in Future Liver Remnant for Posthepatectomy Liver Failure Following Hepatectomy with Extrahepatic Bile Duct Resection. World J Surg 40, 1440–1447 (2016). https://doi.org/10.1007/s00268-016-3441-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3441-1