Abstract
Background
We measured the sizes of metastatic lymph nodes and the relationships thereof by 18F-fluorodeoxyglucose positron emission tomography/computer tomography (PET/CT). We identified risk factors for nodal upstaging in patients with esophageal squamous cell carcinoma (ESCC).
Methods
Eighty-five patients with ESCC who underwent esophagectomy with extensive mediastinal lymphadenectomy were assessed. Two radiologists blinded to pathology data reviewed PET/CT scans, evaluating both primary tumors and lymph node involvement. A pathologist examined all metastatic lymph nodes in terms of maximal diameter (LNmax), the size of the metastatic focus (Fmax), and the metastasis occupation ratio (MOR = Fmax/LNmax).
Results
The maximal tumor length averaged 2.9 ± 0.2 cm and the mean SUVmax of the primary lesion 5.3 ± 0.5. On PET/CT scans, 26 (30.6 %) patients exhibited nodal metastasis and 59 (69.4 %) did not. Pathology grades of pN0, pN1, pN2, and pN3 were assigned to 45 (52.9 %), 24 (28.2 %), 13 (15.3 %), and 3 (3.5 %) patients, respectively. Nodal upstaging was evident in 29 (34.1 %) cases. In 123 metastatic nodes of 4212 nodes dissected, the LNmax was 6.60 ± 0.39 mm, the Fmax 4.47 ± 0.35 mm, and the MOR 0.68 ± 0.03. Of 123 nodes, 85 (69.1 %) were retrieved from PET-negative stations, and the LNmax and Fmax values of these nodes were 5.88 ± 0.42 and 3.75 ± 0.31 mm, respectively. Upon multivariate analysis, tumor length (OR 1.666, p = 0.019) and lymphovascular invasion (OR 41.038, p < 0.001) were risk factors for nodal upstaging.
Conclusion
A significant proportion of nodal metastases were too small to detect via PET/CT imaging. Therefore, meticulous lymph node dissection might be helpful in ESCC patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Esophageal squamous cell carcinoma (ESCC) is an aggressive disease associated with a high frequency of lymph node metastasis compared to other gastrointestinal malignancies [1]. Lymph node metastasis has been recognized as prognostically predictive in esophageal cancer [2], and the number of metastatic lymph nodes is used in the N staging system of the American Joint Committee on Cancer (AJCC) (7th revision) [3]. Accordingly, accurate diagnosis of lymph node metastasis in patients with esophageal cancer is essential for correct preoperative staging, prediction of survival, and treatment plan selection. In particular, preoperative determination of whether the tumor has reached any lymph nodes is important, because patients with metastatic lymph nodes may be candidates for neoadjuvant therapy prior to surgery. Various methods have been used to detect lymph node metastases in esophageal cancer patients, including computed tomography (CT), ultrasonography (US), and endoscopic ultrasonography (EUS). However, even such advanced imaging modalities do not always reliably identify lymph node metastasis prior to surgical resection and pathological examination.
Positron emission tomographic/computer tomographic (PET/CT) scans obtained after administration of 18F-fluorodeoxyglucose (18F-FDG) combine physiological information derived from altered tissue metabolism with precise anatomical localization. Recently, several reports have explored the diagnostic utility of 18F-FDG PET/CT scans in nodal staging of esophageal cancer; various criteria and methods were applied [4, 5]. Several studies found that the diagnostic sensitivity and specificity of PET/CT scans used to assess the locoregional lymph nodes of esophageal cancer patients were as high as 93.9 and 92.06 %, respectively [5, 6]. However, in another study of 565 lymph nodes of lung cancer patients, PET was found to afford poor resolution and failed to identify metastatic foci smaller than 4 mm in diameter [7]. Thus, PET may not be useful for the assessment of locoregional lymph nodes in esophageal cancer if the nodes and their metastatic foci are small. In general, PET is known to be unreliable when used to diagnose small lymph node metastases less than 5 mm in diameter [8].
We performed preoperative PET/CT on all patients operated upon to treat esophageal cancer. Extensive mediastinal lymphadenectomy is a cornerstone of our basic surgical policy [9]. Based on our experience, we conducted the present study to measure the sizes of ESCC metastases in involved lymph nodes and to correlate the pathology results with preoperative PET/CT findings. We explored whether PET/CT scans could be used to determine metastasis to locoregional lymph nodes in ESCC patients. In addition, we identified the incidence of and risk factors for nodal upstaging.
Patients and methods
Eighty-five patients who underwent esophagectomy and total lymphadenectomy from August 2010 to July 2014 were included in this retrospective study (IRB approval No: 4-2014-0354). The inclusion criterion was histologically proven squamous cell carcinoma of the thoracic esophagus; patients who had resectable cervical or abdominal lymph nodes suspected to be associated with a tumor, but patients who did not have unresectable local disease were included. Exclusion criteria were an in situ lesion, concurrent multiple cancers elsewhere, treatment with neoadjuvant chemoradiation or chemotherapy, and prior mediastinal lymph node dissection. Patient demographics, operative data, and pathology findings were recorded prospectively.
Preoperative endoscopic biopsies were performed to confirm the histological diagnoses, and staging work-up included EUS and chest CT, abdomino-pelvic CT, and PET/CT scans. Each CT scan was obtained after infusion of 150 mL of nonionic contrast; 5-mm-thick slices were obtained from the lower neck to the lower borders of both kidneys. All patients underwent ultrasonography, and images were obtained at 3.5 MHz from the chest and abdomen. 18F-FDG PET/CT scans were obtained using either a Discovery600 PET/CT (GE Healthcare, Milwaukee, WI, USA) or a Biograph TruePoint 40 PET/CT (Siemens Medical Systems, CTI, Knoxville, TN, USA). All patients fasted for at least 6 h prior to scanning and peripheral blood glucose levels of all patients were confirmed to be 140 mg/dL or less prior to 18F-FDG injection. Approximately 5.5 MBq/kg body weight 18F-FDG was administered intravenously 1 h before image acquisition. After initial low-dose CT scanning (Discovery600: 30 mA, 130 kVp; Biograph TruePoint: 36 mA, 120 kVp), standard PET imaging, from the neck to the proximal thighs, with an acquisition time of 3 min/bed in the three-dimensional mode was performed. Images were reconstructed via ordered subset expectation maximization (two iterations, 20 subsets).
Tumor length was the longest craniocaudal axial length measured via endoscopy. If multiple nodules were identified, the longest nodule length was recorded as the endoscopic tumor length. If the endoscopist could not identify a tumor, mass, lesion, or nodule, the length of the polyp (the long axis of the diameter of the polyp), the ulcerated area, the mucosal defect, the nodular mucosa, or the focal thickening of the esophageal wall/stricture was recorded [10].
Criteria for preoperative diagnosis of lymph node metastasis
Preoperative staging was based on analysis of PET/CT images. Two radiologists experienced in nuclear medicine visually interpreted reconstructed PET/CT images to identify primary lesions and lymph node metastases using a three-dimensional computer display workstation, reaching consensus on each identification. Lymph nodes exhibiting focally increased 18F-FDG uptake similar to or higher than that of the liver were considered to be malignant. Symmetric 18F-FDG uptake by the bilateral pulmonary hilar lymph nodes was considered to be benign, because esophageal cancer rarely metastasizes to the hilum [11], and symmetric hilar uptake generally reflects chronic inflammation. Calcified lymph nodes were regarded as negative even if uptake was evident [12]. For quantitative analysis, regions of interest were manually placed on primary lesions evident on transaxial images to obtain SUVmax values. Classifications followed the Japanese Guidelines for Clinical Pathologic Studies on Carcinoma of the Esophagus [13].
Lymph node dissection
Surgical procedures were the same as described in our previous reports [9]; the description here is limited to esophagus and lymph node dissection. The thoracic duct, pleura, and all periesophageal tissues of the mediastinum were dissected en bloc. The right paratracheal and right recurrent laryngeal, subcarinal and bilateral hilar, diaphragmatic, and posterior mediastinal lymph nodes adjacent to the descending aorta and the left pleura were then thoroughly dissected. The lymph nodes in the aortopulmonary window (the left tracheobronchial nodes) and the left recurrent laryngeal lymph nodes were dissected separately. In the abdominal procedure, en bloc dissection of lymph nodes was performed along the cardia, lesser curvature, left gastric artery, and celiac axis. Lymph nodes around the common hepatic artery were dissected separately. The left gastric artery was cut at its origin. In addition, the proximal stomach was cut between the right and left gastric artery and resected with the esophagus using a linear stapler, after which a gastric tube was constructed. Neck dissection was performed in patients with upper esophageal cancer or with clinically positive lymph nodes in the neck. For neck dissection, a collar incision was created and the middle deep cervical and supraclavicular lymph nodes were removed en bloc. The lymph nodes along the cervical recurrent laryngeal nerve, located between the common carotid artery and the trachea, were then removed.
Pathological diagnosis of lymph nodes
All patients were staged using the AJCC criteria (7th edition) [3]. Each final pathological diagnosis of lymph node metastasis was compared with the preoperative diagnosis based on PET/CT to determine the accuracy of PET/CT for each lymph node site. All metastatic lymph nodes were microscopically evaluated in terms of maximal diameter (LNmax) and metastatic focus size (Fmax). These data were used to calculate the extent of the metastatic area in each lymph node, yielding the metastasis occupational rate (MOR) for each node. The MOR was derived using the following formula: MOR = LNmax/Fmax [2]. If the metastatic foci within the lymph node were more than one, Fmax was measured in the largest metastatic foci.
Statistical analysis
Clinical and pathological parameters are presented as means ± standard errors for continuous variables, and as frequencies (with % values) for categorical variables. The χ 2 test was used to compare categorical data, and Student’s t test was used to compare continuous variables. Univariate logistic regression was used to explore associations between potential prognostic predictors and nodal upstaging. Odds ratios (ORs) with 95 % confidence intervals (CIs) were calculated via multivariate logistic regression. Preoperative prognostic predictors with p values <0.25 upon univariate analysis were entered into the multivariate logistic regression model. Using Wald stepwise selection, with p < 0.10 as both the entry and removal probability, a final model was obtained. All p values were two sided, and a p value <0.05 was considered to reflect significance. Statistical analysis was performed using SPSS software version 20.0 (SPSS Inc., Chicago, IL, US).
Results
Patient demographics and preoperative PET analysis
Patient demographic data are listed in Table 1. There were 77 (90.6 %) male and 8 (9.4 %) female patients, of mean age 62.5 ± 0.9 years. The tumor location was in the upper esophagus in 6 (7.1 %), middle in 47 (55.3 %), and lower in 32 (37.6 %); 7 patients (8.2 %) had multiple lesions. The mean SUVmax of the primary lesion was 5.3 ± 0.5, and the maximal tumor length 2.9 ± 0.2 cm. The mean number of dissected lymph nodes was 49.6 ± 2.4. The operative mortality was developed in 2 (2.4 %) cases. The frequent operative complications are as follows: vocal cord palsy (25 cases, 29.4 %), pulmonary complications (10 cases, 11.8 %), anastomotic leakage (10 cases, 11.8 %) and chylothorax (2 cases, 2.4 %).
PET/CT scan analysis was used to divide patients into two groups; 59 patients (69.4 %) exhibited no suspicious metastatic lymph node stations (the cN− group) but 26 (30.6 %) did (the cN+ group). The cN+ group had a higher histological grade, longer tumor length, higher SUVmax, more advanced disease stage, and higher incidence of lymphovascular invasion (Table 1).
Pathological status was pN0 in 45 patients (52.9 %), pN1 in 24 (28.2 %), pN2 in 13 (15.3 %), and pN3 in 3 (3.5 %). Twenty-nine (34.1 %) cases of nodal upstaging were noted, 18 (30.5 %) and 11 (42.3 %) in the cN− and cN+ groups, respectively. The frequency of nodal upstaging did not significantly differ between the two groups (p = 0.290).
Lymph node pathology
In total, 4212 lymph nodes were dissected, 349 in the neck, 2325 in the mediastinum, and 1528 in the abdomen. Of all lymph nodes, 123 were diagnosed as metastatic by the pathologist. The most frequent metastatic sites were in the bilateral recurrent laryngeal chains (bilateral recurrent laryngeal and infra-aortic lymph nodes; 36, 29.3 %); the left gastric lymph nodes (28, 22.8 %); and the para-esophageal lymph nodes (23, 18.7 %).
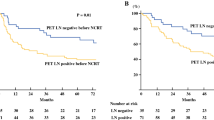
The 123 metastatic nodes were further analyzed (Table 2). The LNmax was 6.60 ± 0.39 mm, the Fmax 4.47 ± 0.35 mm (range 0.1–22 mm), and the MOR 0.68 ± 0.03. Fifty-six (45.5 %) nodes were less than 5 mm in diameter (Fig. 1a), and 82 (66.6 %) contained metastatic lesions that were less than 5 mm in diameter (Fig. 1b). MOR in 41 (33.3 %) of 123 metastatic lymph nodes were less than 0.5. Of the 123 metastatic nodes, 85 were negative on PET/CT (PET−) and 38 positive (PET+). Both the LNmax and the Fmax of nodes from PET− sites were significantly smaller than those of nodes from PET+ sites (5.88 ± 0.42 vs. 8.22 ± 0.78 mm, p = 0.005; 3.75 ± 0.31 vs. 6.10 ± 0.84 mm, p = 0.012, respectively; Table 2).
18F-FDG PET/CT tended to underestimate the N staging in comparison with pathology analysis. The N staging by PET/CT agreed with the histopathological findings in 53 of the 85 (62.4 %) patients, underestimated the N stage in 29 (34.1 %), and overestimated the N stage in 3 (3.5 %, Table 1).
Risk factors for nodal upstaging
We identified risk factors for nodal upstaging (Table 3). Upon univariate analysis, tumor length, SUVmax of the primary lesion, lymphovascular invasion, the presence of multiple lesions, total LN count, and pathological T stage were risk factors for nodal upstaging. Upon multivariate analysis, tumor length (odds ratio 1.666, 95 % CI 1.089–2.551, p = 0.019), and lymphovascular invasion (odds ratio 41.038, 95 % CI 8.736–192.781, p < 0.001) were risk factors for nodal upstaging.
Discussion
Accurate diagnosis of lymph node metastasis in ESCC patients is essential for correct preoperative staging and selection of appropriate treatment (for example, neoadjuvant therapy) prior to surgery. However, accurate diagnosis of lymph node metastasis prior to pathological examination is sometimes difficult, even using advanced imaging methods. Kajiyama et al. performed preoperative lymph node analysis using CT and EUS; the true-positive/true-negative diagnostic rate for all lymph node sites in three fields (the neck, thorax, and abdomen) was only 23.2 % and the false-negative rate 53.7 % [14]. Choi et al. reported that FDG-PET was more accurate than conventional imaging (such as CT imaging or EUS) when used to evaluate metastasis in individual lymph node groups and for N staging of esophageal cancer [6]. Notably, the utility of PET–CT has also been shown for thoracic ESCC by Yuan et al., who found that PET/CT improved the sensitivity (81.71–92.06 %), accuracy (86.15–92.44 %), and negative predictive value (94.83–98.31 %) of 18F-FDG imaging upon assessment of locoregional lymph nodes [5]. Herein, we measured the frequencies of nodal upstaging and downstaging based on routine preoperative PET/CT scanning of all patients with operable ESCC who also underwent extensive lymph node dissection. In contrast to the recent positive results of PET/CT scans on ESCC, precise nodal staging was possible in about 60 % of these patients. Our results indicate that even the most advanced functional imaging modality available, PET/CT, has limitations when used for preoperative nodal staging of ESCC patients.
One reason for inaccurate diagnosis of nodal metastasis in ESCC patients is that the lymph node metastases are small. The average largest diameter of the node metastases in our sample was only 6.60 ± 0.39 mm, and in many cases, the metastasis was significantly smaller than the involved lymph node; the average diameter of metastatic foci was 4.47 ± 0.35 mm. Almost half of all metastatic nodes (45.5 %) were of diameter less than 5 mm, and nearly two-thirds (66.6 %) contained metastatic foci less than 5 mm in diameter. Kajiyama et al. reported similar results upon analysis of 92 ESCC cases [14]. In the cited work, the mean metastasis diameter was 4.8 mm, significantly less than that of the involved lymph nodes. Of all metastatic lymph nodes, 37.2 % were less than 5 mm in diameter, as were 63.1 % of the metastases. In such cases, accurate diagnosis of metastasis prior to surgery would be difficult using conventional radiographic or ultrasonographic examinations. Also, diagnosing small lymph node metastases (less than 5 mm in diameter) remains difficult using functional imaging modalities such as PET [8]. Another reason for frequent nodal upstaging even after PET/CT scanning is that 18F-FDG PET tends to underestimate the extent of regional lymph node involvement in ESCC because of high 18F-FDG uptake by the adjacent primary tumor or tracer uptake by physiological structures at the thoracoabdominal interface [6, 11, 15]. Furthermore, 18F-FDG uptake by lesions in the lower thoracic and upper abdominal areas may be underestimated because of the effect of respiratory motion [16]. In our data, 13 positive lymph nodes from the paracardial station (just below the diaphragm, which imparts the respiratory motion effect) were all negative on PET/CT (Table 2).
Our work has several clinical implications. First, it suggests appropriate surgical policies for treatment of esophageal cancer. If surgery features extensive lymph node dissection, several fatal complications such as pulmonary complications or recurrent laryngeal nerve palsy may arise. Especially, the incidence of vocal cord palsy after radical mediastinal lymphadenectomy ranges from 30 to 80 % [9]. To reduce the morbidity and mortality associated with esophageal cancer surgery, avoidance of unnecessary lymph node dissection is helpful. However, about 40 % of patients exhibited nodal upstaging despite the lack of any evidence of lymph node metastasis on PET/CT; therefore, we suggest that extensive lymphadenectomy should be mandatory for all ESCC patients. Also, the radical lymph node dissection is thus required during operation even if the nodes are not enlarged because almost half (45.5 %) of metastatic lymph nodes were of diameter of less than 5 mm. Even though the extensive lymph node dissection could result in fatal complications and mortality, our data showed acceptable operative outcomes. Second, the indications for neoadjuvant therapy must be carefully selected. Current indication of neoadjuvant therapy in ESCC is the presence of clinically evident lymph node metastasis. Because the underestimation of nodal status by PET/CT is frequent in ESCC, even if a patient exhibits no nodal metastasis upon preoperative PET/CT and other imaging, that patient may be a candidate for neoadjuvant therapy if a risk factor for nodal upstaging is evident. Finally, our work emphasizes that advances in preoperative diagnostic imaging are required. Although visual inspection is regarded as a suitable method of analysis of PET/CT scans obtained from ESCC patients, the diagnostic accuracy thereof is inadequate to allow of nodal staging. I et al. reported that the metabolic tumor volume measured by 18F-FDG PET/CT usefully predicted pathological regional lymph node status in esophageal cancer patients [17]. In addition, Lee et al. found that PET/MR imaging afforded acceptable accuracy in terms of T-staging, compared with EUS, and, although the differences were not statistically significant, was even more accurate than EUS and PET/CT when used to predict the N stage [18]. PET/CT analysis using volume-dependent parameters and a novel imaging modality such as PET/MR imaging may, in future, improve the accuracy of preoperative esophageal cancer staging.
This study has one limitation. Measuring more than 4000 lymph nodes was difficult, so we calculated the LNmax, Fmax, and MOR values of metastatic lymph nodes only. The focus of this study is actually the analysis of pathologic characteristics of metastatic lymph nodes. This prevented calculation of exact cut-off values for lymph nodes detectable on PET/CT. Although we focused on metastatic lymph nodes, we studied a homogenous group of patients who underwent extensive mediastinal lymph node dissection. All specimens were dissected by the 12surgeon before referral to the pathologist. Our clear and consistent surgical policy combined with lymph node dissection is an advantage, increasing the reliability of our data.
In conclusion, nodal upstaging was common despite routine PET–CT scanning, which may be attributable to fact that metastatic ESCC foci are small. Extensive mediastinal lymphadenectomy might be helpful in ESCC to permit accurate pathological staging and possible locoregional disease clearance.
References
Kuwano H, Nakajima M, Miyazaki T et al (2003) Distinctive clinicopathological characteristics in esophageal squamous cell carcinoma. Ann Thorac Cardiovasc Surg 9:6–13
Hosch SB, Stoecklein NH, Pichlmeier U et al (2001) Esophageal cancer: the mode of lymphatic tumor cell spread and its prognostic significance. J Clin Oncol 19:1970–1975
Rice TW, Blackstone EH, Rusch VW (2010) 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol 17:1721–1724
Kato H, Kimura H, Nakajima M et al (2008) The additional value of integrated PET/CT over PET in initial lymph node staging of esophageal cancer. Oncol Rep 20:857–862
Yuan S, Yu Y, Chao KC et al (2006) Additional value of PET/CT over PET in assessment of locoregional lymph nodes in thoracic esophageal squamous cell cancer. J Nucl Med 47:1255–1259
Choi JY, Lee KH, Shim YM et al (2000) Improved detection of individual nodal involvement in squamous cell carcinoma of the esophagus by FDG PET. J Nucl Med 41:808–815
Nomori H, Watanabe K, Ohtsuka T et al (2004) The size of metastatic foci and lymph nodes yielding false-negative and false-positive lymph node staging with positron emission tomography in patients with lung cancer. J Thorac Cardiovasc Surg 127:1087–1092
Räsänen JV, Sihvo EI, Knuuti MJ et al (2003) Prospective analysis of accuracy of positron emission tomography, computed tomography, and endoscopic ultrasonography in staging of adenocarcinoma of the esophagus and the esophagogastric junction. Ann Surg Oncol 10:954–960
Kim DJ, Park SY, Lee S et al (2014) Feasibility of a robot-assisted thoracoscopic lymphadenectomy along the recurrent laryngeal nerves in radical esophagectomy for esophageal squamous carcinoma. Surg Endosc 28:1866–1873
Gaur P, Sepesi B, Hofstetter WL et al (2010) A clinical nomogram predicting pathologic lymph node involvement in esophageal cancer patients. Ann Surg 252:611–617
Yoon YC, Lee KS, Shim YM et al (2003) Metastasis to regional lymph nodes in patients with esophageal squamous cell carcinoma: CT versus FDG PET for presurgical detection—prospective study 1. Radiology 227:764–770
Shim SS, Lee KS, Kim B-T et al (2005) Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging 1. Radiology 236:1011–1019
Isono K (2004) Guidelines for clinical and pathologic studies on carcinoma of the esophagus: preface, general principles, part I. Esophagus 1:61–88
Kajiyama Y, Iwanuma Y, Tomita N et al (2006) Size analysis of lymph node metastasis in esophageal cancer: diameter distribution and assessment of accuracy of preoperative diagnosis. Esophagus 3:189–195
Lerut T, Flamen P, Ectors N et al (2000) Histopathologic validation of lymph node staging with FDG-PET scan in cancer of the esophagus and gastroesophageal junction: a prospective study based on primary surgery with extensive lymphadenectomy. Ann Surg 232:743
Callahan J, Binns D, Dunn L et al (2011) Motion effects on SUV and lesion volume in 3D and 4D PET scanning. Australas Phys Eng Sci Med 34:489–495
Seok H, Kim S-J, Kim IJ et al (2012) Predictive value of metabolic tumor volume measured by 18F-FDG PET for regional lymph node status in patients with esophageal cancer. Clin Nucl Med 37:442–446
Lee G, Hoseok I, Kim S-J et al (2014) Clinical implication of PET/MR imaging in preoperative esophageal cancer staging: comparison with PET/CT, endoscopic ultrasonography, and CT. J Nucl Med 114:138974
Compliance with ethical standards
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, S.Y., Kim, D.J., Jung, H.S. et al. Relationship Between the Size of Metastatic Lymph Nodes and Positron Emission Tomographic/Computer Tomographic Findings in Patients with Esophageal Squamous Cell Carcinoma. World J Surg 39, 2948–2954 (2015). https://doi.org/10.1007/s00268-015-3221-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3221-3