Abstract
To assess the effect of lesion motion and respiration rate on Standardised Uptake Value (SUV) and the ability of 4D PET to restore any loss in SUV and distortion of lesion volume on two PET/CT systems. A Perspex phantom with four cylindrical reservoirs filled with 18F-FDG was used in this study. The cylinders measured 5, 10, 15, and 20 mm in diameter. A GE Discovery STE8 (GE Medical Systems Milwaukee, WI) and a Siemens Biograph 64/40 (Siemens Medical Solutions, Erlangen, Germany) scanner was used to acquire a stationary un-gated PET scan of the phantom. Multiple 10 min list mode 4D PET scans were acquired using the Varian RPM on the GE camera and the Anzai Gating system on the Siemens camera. The phantom was scanned at five different respiratory rates and motion amplitudes in a sinusoidal fashion, 15 RPM/1 cm, 15 RPM/2 cm, 15 RPM/4 cm, 30 RPM/2 cm and 7.5 RPM/2 cm (RPM-respirations per minute). Each scan was reconstructed into ten bins and as an un-gated static image. The SUVmax, SUVmean and volume were measured for all four reservoirs using Siemens TrueD analysis software. With increasing lesion movement the SUVmax and SUVmean decreased and the volume increased with the SUVmax in the smallest lesion underestimated by up to a factor of four. The SUVmax, SUVmean and volume were mostly recovered using 4D imaging regardless of amount of lesion displacement. The larger lesions showed better count recovery and volume correction than the smaller lesions. The respiratory rate had no effect of SUV or volume. Un-gated imaging of moving lesions decreases apparent SUV in small lesions significantly and overestimates volumes. 4D PET scanning recovers most of the apparent loss in SUV and distortion of volumes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The dual imaging modality of PET/CT using FDG is increasingly being used in radiotherapy to aid in the delineation of target volumes [1, 2]. A inherit limitation of PET scanning however is it’s long acquisition time when compared to anatomical imaging modalities such a CT. A PET scan is acquired in steps of between 2 and 5 min with a total whole body scan taking around 20–30 min. Due to the long scan time patients are instructed to breathe freely during the PET and CT acquisitions. This can lead to blurring and mis-registration artefacts between the PET and CT scans making accurate delineation of target volumes difficult [3]. The blurring of PET avid lesions due to respiratory motion has the effect of reducing the apparent intensity of a lesion and increasing its apparent size [4–7].
With the ability to deliver highly conformal stereotactic radiotherapy with small margins accurate delineation of tumour margins is of great importance [8, 9]. On modern PET/CT scanners it is now possible using commercially available respiratory gating systems to perform retrospectively respiratory gated PET [5, 10]. This scanning technique has the potential to provide information about the amount of lesion displacement and direction of movement due to respiration and correct PET images for respiratory motion artefact [4–7]. A number of phantom studies have shown the ability of PET scanning to recover signal lost through the effects of simulated respiratory motion [6, 7]. However, the association between increasing range lesion motion and loss of signal has not been well described. There has also been little comparison of 4D PET scanning between different imaging systems.
At out institution as part of the validation process for this novel technology we designed a Perspex insert to use with the commonly used radiotherapy phantom the Modus Medical Quasar Phantom. The insert contained reservoirs of various sizes that could be filled with know amounts of radioactive tracer. The insert was designed to make the following observations on the two PET/CT systems in our institution:
-
1.
Observe the effect that various amounts of displacement and speeds of motion has on un-gated PET images on various size lesions.
-
2.
Quantify the ability of each of our PET systems to recover signal loss when using 4D PET scanning.
-
3.
Compare the results of the our two cameras the GE-DiscoverySTE8 (GE Medical Systems Milwaukee, WI) and the Siemens Biograph64 (Siemens Medical Solutions, Erlangen, Germany)
Materials and methods
In this study the effect that simulated respiratory motion has on detected activity on a PET/CT scanner was tested. The modus Medical QUASAR respiratory motion phantom (Modus Medical, London, ON) is a commercially available quality assurance phantom that has been developed to simulate respiratory motion during radiotherapy. This phantom was adapted to be used on a PET camera with moving reservoirs of activity to simulate ‘lesions’. This same phantom could then be scanned on either of our PET/CT systems. The phantom could also be attached to either the Varian RPM or Anzai respiratory tracking systems that send breathing trace to the cameras.
Respiratory motion phantom
Figure 1 shows a photo of the phantom used for the study. The body shaped phantom (width 30 cm, height 20 cm, length 12 cm) has two cylindrical holes (diameter 8 cm) which can accommodate various cylinders. As can be seen in the figure, a motor on the phantom can push the cylinder forwards and back various distances, rates and motion patterns. For this study a sinusoidal motion pattern was used.
A customised cylinder was manufactured for the present study and can be seen in the insert in Fig. 1. The Perspex moving part of the phantom was prepared with four cylindrical reservoirs that were filled with the same concentration of 18F-FDG. The reservoirs measured 5, 10, 15 and 20 mm in diameter, all being 15 mm in height. No background activity has been used. Motion patterns of up to 4 cm peak to peak displacement and frequencies between 7.5 and 30 movements per minute (rpm) were programmed.
Data acquisition
The same acquisition process was used for both systems:
-
1.
A stationary helical CT scan for attenuation correction
-
2.
A stationary 3 min acquisition of the phantom as a baseline
-
3.
A 10 min list mode acquisition of the phantom moving in a sinusoidal motion in the following combinations:
-
(a)
15 RPM/1 cm of motion
-
(b)
15 RPM/2 cm of motion
-
(c)
15 RPM/4 cm of motion
-
(d)
7.5 RPM/2 cm of motion
-
(e)
30 RPM/2 cm of motion
-
(a)
The phantom was scanned on two PET/CT systems, a GE Discovery STE8 (GE Medical Systems Milwaukee, WI) scanner using the Varian RPM gating system (Palo Alto, CA) and a (Siemens Medical Solutions, Erlangen, Germany) scanner using the Anzai gating system (Anzai MEDICAL, Shinagawa, Tokyo).
The Varian RPM system employs an infrared camera that monitors the movement of reflective markers on a box placed on a subject’s abdomen. In the case of the phantom the box was placed on a platform that moves up and down in synchronisation with the movement of the phantom insert. The respiratory movement is tracked by the Varian software and a trigger is sent to the PET system at each peak inspiration. The Anzai gating system employs a belt with a pressure sensor that is placed around a subject’s abdomen. The belt was position around the phantom in a similar manner to a patient with the pressure sensor position on top of the moving platform. As the platform moves up and down the pressure changes were sent as an electronic signal to the Anzai detection system. The respiratory trace is tracked by the Anzai software and like the Varian system the trigger is sent to the PET system at peak inspiration.
On each scanner a helical CT scan of the stationary phantom was acquired to provide a transmission scan for attenuation correction. The helical CT scan used 140 kV, effective 50 mA, slice thickness of 3 mm and a gantry rotation time of 1.0 s. Then on each camera a stationary PET scan was acquired of the phantom to act as a baseline measurement. The scan was performed with the phantom position in the first phase of the respiratory cycle. This baseline scan was acquired for 3 min using a 128 × 128 matrix.
The range of 7.5–30 cycles per minute was selected to represent the breathing rate that most patients would fall into. The range of lesion displacement of 1–4 cm was also chosen to reflect a realistic maximum range of tumour motion due to respiration. These ranges were selected based on our own experience and that described in the literature [11]. Each scan was reconstructed into an un-gated 3D scan using CT attenuation correction, OSEM iterative reconstruction with four iterations and eight subsets and correction for scatter and randoms. Each of the scans was also re-binned into ten gates using the respiratory trigger and reconstructed using the same parameters with attenuation correction applied using the co-acquired CT.
Data analysis
Using the Siemens TrueD image analysis software for all data from both PET/CT scanners the SUVmax, SUVmean, and volume of each lesion was measured using a 40% SUVmax threshold on the un-gated (3D) scan. A volume of interest using a semi-automated threshold method was used to outline all the lesions. A percentage of the maximum SUV was chosen to contour the lesions in order to remove operator bias and 40% has been shown to be a reproducible method of contouring tumour volumes [12, 13]. Using a percentage of the SUV max rather than a fix threshold meant that as the signal was degraded due to motion the contours would remain consistent. The same parameters were measured in all ten bins of the gated (4D) scan again using a 40% SUVmax threshold to contour the activity. The average SUVmax, SUVmean, volume of the ten bins was calculated and compared to the values obtained from the un-gated 3D scan. All the values were compared to the baseline stationary scan. All outlines were created by a single operator experienced in PET image analysis.
The software is also able to measure the maximum displacement between two volumes of interest. This is done by taking the centre voxel of each volume on interest (VOI) in all ten bins and measure the distance between the two VOI’s (Table 1).
Results
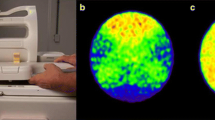
As expected the apparent SUV decreases in a stationary phantom for smaller volumes as can be observed in Fig. 2. The effect is due to the spatial resolution of the PET scanners (4 mm in plane in both systems) and only in the largest lesion studied here (2 cm diameter) the full SUV max is recorded Fig. 3.
Lesion displacement and SUV
On both cameras there was a clear association between increasing lesion motion and loss of SUV on the un-gated scan compared to the baseline. This is displayed graphically in Fig. 4. The average SUVmax from all 10 bins was graphed on the y-axis and the amount of displacement was graphed on the x-axis. The smaller lesions showed a greater drop in SUVmax at the highest displacement than the larger lesions. On the GE-STE8 at 4 cm of movement the SUVmax of the 20 mm lesions dropped by 150% (0.92–0.36) while SUVmax of the 5 mm lesion dropped by 450% times (0.33–0.06). The biograph showed the same pattern where smaller lesions showed greater drop in SUVmax due to movement than the larger lesions.
The 4D acquisition was able to recover most of the apparent loss in SUV regardless of the amount of motion. On both cameras the larger lesions showed better signal recovery than the smaller lesions. On the GE-STE8 SUVmax of the 20 mm lesion at 1,2, and 4 cm of movement were 0.86, 0.85, and 0.85 compared to the baseline value of 0.92. However the SUVmax of the 5 mm lesion was 0.18, 0.22, 0.23 compared to 0.33 on the baseline scan. The Siemens Biograph64 showed the same pattern where the signal recovery on the 4D scan was better in the larger lesions that the smaller. This is shown in Fig. 4 where the dotted lines show the decrease in SUVmax of the four lesions at 0, 1,2 and 4 cm of movement and the bold line shows the SUVmax of the gated scans.
Lesions displacement and volume
Using un-gated 3D scanning there was a clear correlation between increasing motion and volume. On Both cameras at 4 cm of movement there was up to a sevenfold increase in volume on the un-gated scan compared to the baseline.
As can be seen graphically in Fig. 5 where the average volumes of the lesions are on the y-axis and the amount of lesion displacement is on the x-axis. In the gated scans the volume of a lesion as compared to the stationary scan was almost completely restored across all displacement amounts used on both cameras. The volume was also consistent across all three amounts of lesions displacement used. On the GE-STE8 at 1, 2, and 4 cm of movement the volume of the 20 mm lesion was 3.96, 3.85 and 3.85 cm3 respectively. This pattern was similar on the Siemens-Biograph64 as can be seen in Fig. 5.
Respiration rate
The phantom was scanned with 2 cm of movement at three different respiration rates 7.5, 15 and 30 cycles per minute. On both cameras across the three rates there was little difference in the SUVmax, SUVmean and volume of the four lesions. The same results were shown on the Siemans-Biograph64. This is seen in Fig. 6 where the SUVmax and volume values for each of the four lesions are very close.
Discussion
It is intuitively understood that the SUV of moving lesions as measured with respiratory gated PET is higher than un-gated PET. In one of the largest in vivo cohorts Lupi et.al. [4] found, “the use of respiratory trigger induced rather variable but overall consistent increases in SUV”. From the results of this phantom study it is possible to infer that the variable increase in SUV is a result of the variable amount of movement seen in the lung lesions analysed. Our results compare favourably with a similar phantom study carried out by Park et al. [6] who found that signal loss depends both on the amount of displacement and pattern of respiratory motion. In their study they also found that 4D-PET was able to recover most of the loss induced by respiratory motion. Our study has found that this appears to be true for both the GE-STE8 scanner with the Varian gating system and the Siemens Biograph64 with the Anzai gating system. While the results from the two cameras are similar the GE-STE8 does appear to recover more of the lost signal due to motion than the Biograph. It can be observed that the SUVmax for the stationary phantom on the Biograph was higher that the GE-STE but with 1 cm of motion the SUVmax values were similar on both systems. These differences may be explained by the different technology employed by the two manufacturers. The GE STE8 uses a Bismuth germinate of BGO crystal detector and the Biograph uses a Lutetium Orthosilicate or LSO crystal detect. The differences could also be explained by uncertainties in the predictability of the respiratory motion or the different respiratory motion tracking systems employed. A paper comparing the RPM and ANZAI systems found that the estimation of tumour position using different monitoring systems may vary depending on the system used [10]. In general quantitation between cameras employing different technology are not equivalent. It is for this reason that therapeutic monitoring at different time points in the same patient are always performed on the same camera [14]. While there are minor differences in SUVmax between the cameras the pattern of recovery does appear similar between the two cameras.
Given the significant loss in SUV signal observed in moving objects it will be difficult to use absolute SUV as a determinant of malignancy in lung cancer. This would be seen to complicate attempts to auto contour lesions based on a % of SUVmax or a fixed SUV threshold. Respiratory Gated PET scanning has the potential to improve this problem.
The distortion in lesion volume on the PET scan due to respiration is an important consideration in scans used for radiotherapy planning. An assumption is made that as the PET scan is taken over a long period of time the blurring of the PET lesion accounts for all movement. However with the availability of highly conformal dose targeting in radiotherapy obtaining the true PET volume and information about the amount of motion and direction could improve dose delivery and decrease the chances of a geometric miss [15, 16].
In this study we have attempted to show the effect of movement on SUV and volume and validate the ability of respiratory gated PET to correct for this. We have used a simple phantom design without any background or attenuating medium to do this. Our results show that increasing movement has a strong association with SUV loss and volume distortion independent of lesion size. The results also show that respiratory gated scanning should be able to recover most of the SUV loss and volume distortion regardless of the rate of respiration or amount of motion.
This study does not take into account the effect that background or various attenuating media will have of respiratory gated PET. Also the respiration that has been modelled is uniform in frequency, shape and baseline. Any deviation from this pattern is likely to produce poorer signal recovery than presented in this work. The results of this study likely represent the upper limit of the ability of 4D PET to recover loss of signal due to respiratory motion. We plan to introduce these variables in subsequent experiment. It will be now important to investigate if the same results are observed in actual patient studies.
Conclusion
Un-gated imaging of moving lesions decreases apparent SUV and overestimates volumes. There is a strong association between the amount of lesion displacement and decrease in apparent SUV. Respiratory gated PET scanning using both the GE/Varian and Siemens/Anzai systems recovers most of the apparent loss in SUV and distortion of volumes. The respiration rate has no effect on the ability of 4D PET to correct the SUV and volumes for motion.
References
Manus MPM (2010) Use of PET/CT for staging and radiation therapy planning in patients with non-small cell lung cancer. Q J Nucl Med Mol Imaging 54(5):510–520
Manus MM, Hicks RJ, Everitt S (2006) Role of PET-CT in the optimization of thoracic radiotherapy. J Thorac Oncol 1(1):81–84
Aristophanous M et al (2011) Clinical utility of 4D FDG-PET/CT scans in radiation treatment planning. Elsevier, Amsterdam
Lupi A et al (2009) The effect of 18F-FDG-PET/CT respiratory gating on detected metabolic activity in lung lesions. Ann Nucl Med 23(2):191–196
Nehmeh SA et al (2004) Four-dimensional (4D) PET/CT imaging of the thorax. Med Phys 31(12):3179–3186
Park SJ et al (2008) Evaluation of the combined effects of target size, respiratory motion and background activity on 3D and 4D PET/CT images. Phys Med Biol 53(13):3661–3679
Pevsner A et al (2005) Effect of motion on tracer activity determination in CT attenuation corrected PET images: a lung phantom study. Med Phys 32(7):2358–2362
Siva S, Manus MM, Ball D (2010) Stereotactic radiotherapy for pulmonary oligometastases: a systematic review. J Thorac Oncol 5(7):1091–1099
Ball D (2008) Stereotactic radiotherapy for nonsmall cell lung cancer. Curr Opin Pulm Med 14(4):297–302
Otani Y et al (2010) A comparison of the respiratory signals acquired by different respiratory monitoring systems used in respiratory gated radiotherapy. Med Phys 37(12):6178–6186
Seppenwoolde Y et al (2002) Precise and real-time measurement of 3D tumor motion in lung due to breathing and heartbeat, measured during radiotherapy. Int J Radiat Oncol Biol Phys 53(4):822–834
Bradley J et al (2004) Impact of FDG-PET on radiation therapy volume delineation in non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 59(1):78–86
Erdi YE et al (2002) Radiotherapy treatment planning for patients with non-small cell lung cancer using positron emission tomography (PET). Radiother Oncol 62(1):51–60
Boellaard R et al (2010) FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging 37(1):181–200
van Herk M (2007) Different styles of image-guided radiotherapy. Semin Radiat Oncol 17(4):258–267
Webb S (2001) Concepts for shuttling multileaf collimators for intensity-modulated radiation therapy. Phys Med Biol 46(3):637–651
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Callahan, J., Binns, D., Dunn, L. et al. Motion effects on SUV and lesion volume in 3D and 4D PET scanning. Australas Phys Eng Sci Med 34, 489–495 (2011). https://doi.org/10.1007/s13246-011-0109-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-011-0109-x