Abstract
Background
Hepatolithiasis is a well-known risk factor of cholangiocarcinoma. Despite advances in diagnostic modalities, diagnosing cholangiocarcinoma in patients with hepatolithiasis still challenging and there are not enough reports on the incidence of cholangiocarcinoma in patient with hepatolithiasis after treatment. We aimed to evaluate the incidence and clinical characteristics of cholangiocarcinoma in patients with hepatolithiasis who underwent liver resection or non-resection.
Methods
Among a total of 257 patients who received treatment for hepatolithiasis, 236 patients were eligible for analysis. Exclusion criteria were follow-up period less than 9 months, preoperative diagnosis of cholangiocarcinoma, occurrence of cholangiocarcinoma within 1 year after treatment. Completeness of stone clearance was defined when there was no intrahepatic duct stone during whole follow-up period. A retrospective study was done to analyze the patients’ characteristics, the results and complications of the procedure, and the long-term outcomes for these patients. Kaplan–Meier method and cox proportional regression were used for statistical analysis.
Results
95 patients underwent hepatic resection (resection group) and 144 patients did not (non-resection group). Complete stone clearance was 71 % (67/95) in resection group and 41 % (58/141) in non-resection group (p < 0.001). The incidence of cholangiocarcinoma was 6.8 % (16/236) during follow-up period (mean 41 ± 41 months). Cholangiocarcinoma occurred 6.3 % (6/95) and 7.1 % (10/141) in resection and non-resection group, respectively. There was no significant difference in survival between two groups (p = 0.254). In analysis of according to completeness of stone clearance regardless of treatment modality, cholangiocarcinoma incidence was higher in patients with residual stone (10.4 %) than complete stone removal (3.3 %) (p = 0.263). On multivariate analysis, none of the factors (age, gender, CA19-9, stone location, bile duct stenosis, liver atrophy, stone recurrence, residual stone, and hepatic resection) showed relationship with the incidence of cholangiocarcinoma.
Conclusion
Hepatic resection for hepatolithiasis is considered to have a limited value in preventing cholangiocarcinoma and the patients should be carefully followed even after hepatic resection. A combination of different treatment modalities is necessary to decrease the residual stone and improve the outcome of the patients with hepatolithiasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatolithiasis, intrahepatic duct stones, is frequent in Asian countries and also it is one of the major risk factors for cholangiocarcinoma [1, 2]. The overall incidence of cholangiocarcinoma in association with hepatolithiasis has been reported to be 4–12 % [3–5]. Intrahepatic stone makes chronic recurrent cholangitis and biliary carcinogenesis is caused by prolonged inflammation of the biliary epithelium secondary to bile duct stones, bile stasis, and bacterial infections [6–8].
Stone removal using percutaneous transhepatic choledochoscopic lithotomy (PTCSL) can resolve the cholangitis due to stone [9] and also surgical treatment such as hepatic resection can eliminate the inflammatous hepatic segment including stones [10]. Despite the various efforts to remove the stones and advances in diagnostic modality, early diagnosis of cholangiocarcinoma is still challenging in these patients [11].There have been insufficient data regarding the long-term outcome of hepatectomy as the treatment modality of hepatolithiasis. Furthermore, the literature contains few data for occurrence of cholangiocarcinoma after treatment of hepatolithiasis.
This study was aimed to evaluate the incidence of cholangiocarcinoma and clinical characteristics after treatment in hepatolithiasis patients.
Material and methods
Patients
We retrospectively reviewed that the patients were treated for hepatolithiasis from January 2004 to December 2013, at Korea University Anam and Guro Hospital, Korea University College of Medicine, Seoul, Korea.
Among 257 patients included in this study, 236 patients were eligible for analysis and total 21 patients were excluded. Exclusion criteria were follow-up period less than 9 months, preoperative diagnosis of cholangiocarcinoma, occurrence of cholangiocarcinoma within 1 year after treatment.
All patients were received adequate procedures including hepatic resection for stone removal. Hepatic resection was preferred in the patients with atrophy of involved liver segments or lobe on initial CT. PTCSL and endoscopic retrograde cholangioscopy were offered in all indicated patients during follow-up period. As medical treatment, broad spectrum antibiotics were used when cholangitis is suspected.
Completeness of stone clearance was defined when there was no intrahepatic duct stone during whole follow-up period. Either remnant or new stone was regarded as residual stone. Recurrence of stone was defined to be detected on previously treated bile duct. The definition of development of cholangiocarcinoma was occurrence of tumor in hepatic lobe with stone.
Patients were followed up 1 year after treatment and then whenever cholangitis was recurred. Abdominal CT or MRI was taken before treatment and 1 year after. In case of hepatic resection, additional exam was taken within 1 year after operation.
We compared the two groups during the same study period in regard to the patients’ characteristics, complete stone clearance, and occurrence of cholangiocarcinoma as the long-term outcomes.
Statistical analysis
The t test and Mann–Whitney U test were used for continuous variables. Categorical variables were tested by the Person χ 2 test. The cumulative rates of cholangiocarcinoma were analyzed by the Kaplan–Meier method and compared using the log-rank test. Cox proportional hazards regression model (variables: age, gender, CA19-9, location of stone, bile duct stenosis, liver atrophy, residual stone, stone recurrence, and liver resection) was used for risk development of cholangiocarcinoma. p values less than 0.05 were considered statistically significant.
Results
Patient characteristics
Ninety-five patients underwent hepatic resection (resection group) and 141 patients were treated without hepatic resection (non-resection group). Mean follow-up duration was 41 ± 41 months.
We compared the two groups with regard to the clinical characteristics. The patient’s characteristics are described in Table 1. Mean age was significantly younger in hepatic resection group than the non-resection group. There was no significant difference in level of CA 19-9 and symptoms between the two groups.
Intrahepatic duct stone location
The most common site of the intrahepatic duct stone was left hepatic lobe. Stone distribution in liver was 54.7 % (129/236) in the left lobe, 23.7 % (56/236) in the right lobe, and 21.6 % (51/236) in both lobes. Stone location in non-resection group and resection group was 44.7 % (63/141) and 69.5 % (66/95) % in the left lobe, 31.9 % (45/141) and 11.6 % (11/95) in the right lobe, 23.4 % (33/141) and 18.9 % (18/95) in both lobes, respectively. Left intrahepatic duct stone was more frequent in resection group (p < 0.001).
Treatment for intrahepatic duct stone
In 141 patients of non-resection group, PTCSL was done in 62 patients, CBD exploration with choledochoscopic examination in 9 patients, and intraoperative choledochoscopic examination in 4 patients. Bilio-enteric anastomosis was done in 4 cases (choledochojejunostomy). Thirty-three patients had stones in both hepatic lobes at initially, and new intrahepatic duct stones were found in 50 patients during follow-up. These 83 patients (59 %) were considered to have residual stones.
In hepatic resection group, left hemihepatectomy or lobectomy was frequently used in 87.4 % (83/95) and right lobectomy or segmentectomy was done 12.6 % (12/95). Choledochojejunostomy was done in 3 patients. Peri-operative PTCS was performed in 10 patients of 18 patients with stones in both hepatic lobes. Of 18 patients with both hepatic lobe stones, only 8 patients had residual stones constantly after resection. One patient who failed to remove due to stricture underwent PTCSL after operation. In 10 patients, new stone was detected in other hepatic segment after surgery. Nine patients with both hepatic lobes stones had recurrence after PTCSL. Total 28 patients (29 %) were considered to have residual stone in resection group. There was no peri-operative death.
Complete stone clearance was possible in 41 % (58/141) of non-resection group and 71 % (67/95) of resection group. Residual stone rate was significantly low in resection group. (p < 0.001) There was no significant difference in bilio-enteric anastomosis of treatment (p = 0.887).
Incidence of cholangiocarcinoma during follow-up
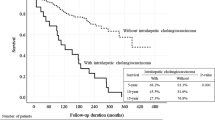
Among the 236 patients with hepatolithisis, intrahepatic cholangiocarcinoma occurred in total 16 patients (6.8 %) (Fig. 1).The clinical features are summarized in Table 2. The median tumor occurrence time was 28 months (13–111 months). Among 16 patients with cholangiocarcinoma, 6 patients (6.3 %) developed in hepatic resection group and 10 patients (7.1 %) developed in non-resection group. There was no significant difference in the cholangiocarcinoma incidence between the two groups (p = 0.254) (Fig. 2).
Cholangiocarcinoma according to completeness of stone clearance
When analyzed according to completeness of stone clearance regardless of treatment modality, cholangiocarcinoma occurred in four patients among the 125 patients with complete stone clearance (3.2 %). On the other hand, 12 patients developed cholangiocarcinoma among the 111 patients with incomplete stone clearance (10.8 %). Cholangiocarcinoma incidence was high in patients with residual stone, but there is no difference in survival between two groups by Kaplan–Meier log-rank test (p = 0.263) (Fig. 3).
In hepatic resection group, cholangiocarcinoma occurrence was significantly low in patients with complete stone clearance (3 %, 2/67) compared with incomplete stone clearance (14.2 %, 4/28) (p = 0.042). However, cholangiocarcinoma developed even after complete stone clearance in two patients, one in caudate lobe 14 months after left hemihepatectomy and the other in medial segment after left hemihepatectomy, 28 months later.
Also in non-resection group, cholangiocarcinoma occurred in 3.4 % (2/58) of patients with complete stone clearance and 9.6 % (8/83) of patients with incomplete stone clearance, there is no difference in survival between two groups (p = 0.510).
Risk factors associated with cholangiocarcinoma
In cox regression analysis, residual stone and hepatic resection did not show the relation with incidence of cholangiocarcinoma. Only CA 19-9 was found to be significant risk factor for survival (Table 3). However, none of the factors was found to be significant in multivariate analysis.
Discussion
Although there have been an effort to manage stones effectively including hepatic resection, hepatolithiasis is associated with a recurrent cholangitis, biliary stricture, and stone formation. Furthermore, the biliary carcinogenesis is caused by prolonged inflammation through recurrent hepatolithiasis and cholangitis. Epidemiological, pathological, and genetic studies have showed the relationship between hepatolithiasis and cholangiocarcinoma [6–8]. The presence of cholangiocarcinoma-associated hepatolithiasis is the main factor compromising long-term survival in patients with hepatolithiasis [10] but unfortunately early diagnosis of concomitant cholangiocarcinoma is difficult [11]. Hepatic resection is frequently considered for the definitive treatment of hepatolithiasis, because it can remove stones and stenotic bile duct simultaneously, reduce the risk of recurrent stones and development of cholangiocarcinoma [12–15]. Nevertheless, subsequent late development of cholangiocarcinoma may appear months to years after the initial hepatectomy [10, 16, 17].
To the best of our knowledge, few studies on the comparing of treatment modality for hepatolithiasis reported that surgical treatment showed better long-term outcome [9, 18]. But it is not clear whether hepatic resection could reduce the occurrence of cholangiocarcinoma.
We analyzed the data of patients who were treated for hepatolithiasis. Long-term outcomes especially occurrence of intrahepatic cholangiocarcinoma were compared according to treatment modality. During the 41 months of mean follow-up period, total 16 patients (6.8 %) developed cholangiocarcinoma. No significant difference was proven in hepatic resection group and non-hepatic resection group (6.3 vs. 7.1 %, p = 0.526). Furthermore, there was no difference in clinical manifestation and laboratory data to predict the development of malignancy between the two groups. Hepatic resection did not show any advantage for cholangiocarcinoma in this study, especially if incomplete clearance of stones was performed. Although it was generally agreed that hepatic resection could remove not only stones and ductal stricture but also premalignant pathologic change and concomitant cholangiocarcinoma; however, it did not showed any difference in survival according to subsequent cholangiocarcinoma in this study. Furthermore, cholangiocarcinoma developed in two patients with complete stone clearance. In these cases, cancer was developed in near hepatic lobe from resected hepatic segment. This may be caused that any premalignant change such as biliary intraepithelial neoplasia exists in nearby bile duct. Long-term inflammation derived from neighboring segment stones may promote liver carcinogenesis and aggressive hepatic resection including neighboring segments may prevent cholangiocarcinoma.
Incidence of cholangiocarcinoma was higher in patients with residual stone than patients without residual stone (10.8 vs. 3.2 %, p = 0.054). This finding was similar in hepatic resection group and non-resection group (14.2 vs. 3 %, 9.6 vs. 3.4 %, respectively) but significant difference was shown only in hepatic resection group (p = 0.042). This suggests that complete stone removal is important in the prevention of cholangiocarcinoma. Previous studies on long-term outcomes after treatment reported that residual stone and bile duct stricture are the risk factors for complication [9].
But the treatment strategy for complete stone removal is not simple especially in patients with both hepatic lobes stones. Although it looks like high proportion of the patients with residual stone in resection group, purely new stone detection was in 10 patients (10.5 %) because 8 patients had stones in both hepatic lobes. In our cases, 4 patients with residual stones after hepatic resection had all both hepatic lobe stones and cholangiocarcinoma developed in right hepatic lobe. This fact would decrease the positive effect of hepatic resection in survival. This may cause the different results compared with other reports. We think that the incidence of cholangiocarcinoma would be low in patients with complete stone clearance and it yields the importance of complete stone removal in hepatolithiasis, which reduce the incidence of cholangiocarcinoma and will increase the survival.
Limitation of this study is the different follow-up period between two groups. And 41 months would be short interval to clarify the survival difference and the risk factor of cholangiocarcinoma. Second, this study was limited by retrospective nature.
In summary, hepatic resection for hepatolithiasis is considered to have a limited value in preventing the risk of cholangiocarcinoma. Neither did for survival after treatment. Hepatic resection should be offered to selected patients and careful follow-up for cholangiocarcinoma is needed even after hepatic resection. A combination of different treatment modalities is necessary to decrease the residual stone and improve the outcome of the patients with hepatolithiasis.
References
Tyson GL, El-Serag HB (2011) Risk factors for cholangiocarcinoma. Hepatology 54(1):173–184
Ben-Menachem T (2007) Risk factors for cholangiocarcinoma. Eur J Gastroenterol Hepatol 19(8):615–617
Lin CC, Lin PY, Chen YL (2013) Comparison of concomitant and subsequent cholangiocarcinomas associated with hepatolithiasis: clinical implications. World J Gastroenterol 19(3):375–380
Liu CL, Fan ST, Wong J (1998) Primary biliary stones: diagnosis and management. World J Surg 22(11):1162–1166. doi:10.1007/s002689900536
Su CH, Shyr YM, Lui WY, P’eng FK (1997) Hepatolithiasis associated with cholangiocarcinoma. Br J Surg 84(7):969–973
Zhou Q, Gong Y, Huang F, Lin Q, Zeng B, Li Z et al (2013) Expression Levels and Significance of Nuclear Factor-κB and Epidermal Growth Factor Receptor in Hepatolithiasis Associated with Intrahepatic Cholangiocarcinoma. Dig Surg 30(4–6):309–316
Lee KT, Chang WT, Wang SN, Chuang SC, Chai CY, Hu SW (2006) Expression of DPC4/Smad4 gene in stone-containing intrahepatic bile duct. J Surg Oncol 94(4):338–343
Kuroki T, Tajima Y, Kanematsu T (2005) Hepatolithiasis and intrahepatic cholangiocarcinoma: carcinogenesis based on molecular mechanisms. J Hepatobiliary Pancreat Surg 12(6):463–466
Park JS, Jeong S, Lee DH, Bang BW, Lee JI, Lee JW et al (2013) Risk factors for long-term outcomes after initial treatment in hepatolithiasis. J Korean Med Sci 28(11):1627–1631
Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T et al (2009) Outcomes of hepatic resection for hepatolithiasis. Am J Surg 198(2):199–202
Hur H, Park IY, Sung GY, Lee DS, Kim W, Won JM (2009) Intrahepatic cholangiocarcinoma associated with intrahepatic duct stones. Asian J Surg 32(1):7–12
Uchiyama K, Kawai M, Ueno M, Ozawa S, Tani M, Yamaue H (2007) Reducing residual and recurrent stones by hepatectomy for hepatolithiasis. J Gastrointest Surg 11(5):626–630
Cheung MT, Kwok PC (2005) Liver resection for intrahepatic stones. Arch Surg 140(10):993–997
Chen DW, Tung-Ping R, Liu CL, Fan ST, Wong J (2004) Immediate and longterm outcomes of hepatectomy for hepatolithiasis. Surgery 135(4):386–393
Cai X, Wang Y, Yu H, Liang X, Peng S (2007) Laparoscopic hepatectomy for hepatolithiasis: a feasibility and safety study in 29 patients. Surg Endosc 21(7):1074–1078
Chijiiwa K, Ichimiya H, Kuroki S, Koga A, Nakayama F (1993) Late development of cholangiocarcinoma after the treatment of hepatolithiasis. Surg Gynecol Obstet 177(3):279–282
Sheen-Chen SM, Chou FF, Eng HL (1991) Intrahepatic cholangiocarcinoma in hepatolithiasis: a frequently overlooked disease. J Surg Oncol 47(2):131–135
Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS (2009) Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery 146(5):843–853
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H.J., Kim, J.S., Suh, S.J. et al. Cholangiocarcinoma Risk as Long-term Outcome After Hepatic Resection in the Hepatolithiasis Patients. World J Surg 39, 1537–1542 (2015). https://doi.org/10.1007/s00268-015-2965-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-2965-0