Abstract
Background and Aim
Cholangiocarcinoma (CCA) often develops after the hepatic resection for hepatolithiasis as well as indwelling it. We studied the incidence and prognosis of subsequent CCA in patients with hepatolithiasis in South Korea.
Methods
We identified individuals with diagnosed CCA at the time of or after surgery, during 2002–2016, from the Korean National Health Insurance. The incidences and survival rates of subsequent CCA were analyzed and compared with concomitant CCA. The standardized incidence ratios (SIRs) of CCA in this cohort were evaluated in the standard Korean population. All data were stratified by the presence of intrahepatic or extrahepatic CCA, age and sex.
Results
Of the 7852 patients with hepatectomy for BDS, 433 (5.84%) had concomitant CCA. Over the 12-year follow-up, 107 of 7419 (1.98%) patients were diagnosed with subsequent CCA. Patients with hepatic resection for BDS revealed higher SIRs for subsequent CCA (12.89, 95% CI 10.96–15.15) in cases of both intrahepatic CCA (13.40, 10.55–17.02) and extrahepatic CCA (12.42, 9.98–15.46). The median survival time for subsequent CCA was 0.87 years, while that for concomitant CCA was 2.79 years. Having subsequent CCA (HR 2.71, 95% CI 2.17–3.40) and being male (HR 1.28, 1.05–1.57) were related to a shorter survival time. The CCA site and age at CCA diagnosis were not related to prognoses.
Conclusions
Subsequent CCA developed in 2% of the patients with hepatic resection for benign BDS until 10 years and was associated with poorer prognoses than concomitant CCA. Future studies focused on the long-term surveillance for CCA in such patients are needed.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Hepatolithiasis (HL), the presence of stones within the intrahepatic bile ducts, and its associated diseases are highly prevalent in Eastern countries; however, their prevalence is on the decline in these countries [1].
Surgical resection is recommended in cases of single-lobe HL with atrophy, uncontrolled strictures, symptom durations longer than 10 years, and a long history of biliary enteric anastomosis [2,3,4,5,6]. Cholangiocarcinoma (CCA) was found in 3.3–23.3% of patients with hepatic resection for HL, constituting approximately 15% of all CCA cases [1, 7,8,9]. Korea is among the countries in which HL-associated CCA is most prevalent [1]. Although the risk of malignancy is lower in patients with complete stone removal than in those with residual stones, CCA develops in 1.6–9.9% of patients during follow-up after surgery [1, 4, 7]. The development of concomitant or subsequent CCA is an independent prognostic factor in such patients [10, 11]. Performing second surgery for subsequent CCA after hepatic resection is very difficult due to advanced cancer stage or insufficient remnant liver volume [12]. Therefore, surveillance for the development of subsequent CCA should be considered in these patients [1].
Studies from different Asian countries have reported on subsequent CCA development after hepatic resection for HL [1, 4, 7, 12, 13]. However, the incidence, duration between surgery and diagnosis, and survival rates associated with subsequent CCA have not yet been defined. As most of the aforementioned studies had a retrospective case–control design and were conducted in a single institution, their results are inconsistent. Therefore, a nationwide study using big data for long-term follow-up can prove helpful in improving the power of study. In this study, we used data from the Korean National Health Insurance (NHI), which covers the entire Korean population—comprising more than 50,000,000 people [14].
This study aimed to analyze the incidence, risks, and prognoses associated with subsequent CCA in patients with hepatic resection for bile duct stones (BDS). We defined BDS treated with hepatic resection as HL, and analyzed the incidence and prognosis of subsequent CCA in comparison with those of concomitant CCA.
Materials and Methods
Data Source
This study used the Korean NHI claims database, to which each healthcare provider electronically submits all in-patients’ and out-patients’ diagnosis and treatment data for the reimbursement of insurance. The database includes almost all the information on the medical services provided to patients, i.e., diagnosis, patient demographics, prescriptions, surgeries, tests, and imaging data. Diagnostic information is documented in accordance with the International Classification of Disease (ICD)-10.
In 2005, the Korean government launched a Support for Serious Illness (SSI) program, in which the coinsurance rate is reduced for registered cancer patients. Registration in the program requires a physician’s diagnosis which necessitates confirmation by more than one among pathology results, typical radiologic findings, or laboratory data. The cancer diagnosis is further reviewed by another healthcare professional to ensure it meets the diagnostic criteria, and the data are then submitted to the NHI. The SSI data are integrated into the NHI; we used this data in our study.
To analyze patient mortality, we used Statistics Korea, which provides national sources of vital status information via the Korean Governmental Vital Statistics. The dates of death were collected in all the deceased cases, which enabled the calculation of the number of person-years of the study population. By linking the NHI and SSI databases, we were able to track CCA patients and identify their vital status. This study was approved by the Ethics Committee of Korea University.
Study Population
We extracted all hepatectomy cases with a diagnosis of BDS, registered between January 1, 2002, and December 31, 2016, from the NHI-SSI database. We identified patients who underwent hepatectomy (Q7221–Q7225) with a BDS diagnosis (K80.0–K80.9), who were older than 40 years, were followed up for more than 1 year, and had no previous history of digestive system cancers and hepatocellular carcinoma (HCC). We identified patients registered in the SSI database by searching for the following ICD-10 codes: intrahepatic CCA (ICC, C22.1), HCC (C22.0), extrahepatic CCA (ECC, C24.0–C24.9) and other digestive cancers (C15.0–C21.9, C22.2–C22.9, C23.0–C23.9, and C25.0–C25.9). A 3-year washout period was used to prevent prevalent cancer cases from interfering with the data. The study’s cancer patients were followed up until December 31, 2015, and October 31, 2016, for the detection of subsequent cancers and identification of their vital status, respectively. For a given cancer type, the person-years at risk were calculated from the date of diagnosis of the study cancer to the date of cancer diagnosis or the exit date.
The database used in our study included the following variables: identity, sex, birth date, date of last follow-up, and cause of death. All patients were followed up until the end of December 2015 for the determination of their vital status.
Statistical Analysis
The incidence of subsequent CCA following surgery in the study population was compared to that of the general population, and the SIRs with their 95% confidence intervals (CIs) were calculated. The SIR is an estimate of cancer occurrence in a population relative to what could be expected if these patients had the same cancer experience as the general population. The incidence rates of the general population, derived from the KCR registry, were used to compute the expected numbers. The time at risk was measured starting from the date of surgery to the date of CCA diagnosis, the date of death, or the predetermined censoring date. The SIRs were computed for sex and age at the time of the cancer diagnosis (40–59, 60–79, and ≥ 80, years). The 95% CIs for the SIRs were determined assuming a Poisson distribution for the observed number of cancer cases. Cumulative incidence curves displayed the predicted cancer risk in our study’s cancer patients based on sex.
A Chi-square test was used to compare the characteristics of those with and without CCA. Using the vital statistics, Kaplan–Meier survival analysis was performed, generating a Kaplan–Meier survival plot. Here, the cumulative survival associated with subsequent CCA was compared to that of concomitant CCA. Cox proportional hazard analysis was used to examine the relationship between survival and explanatory factors such as sex, age group, cancer location and subsequent CCA in terms of the hazard ratio (HR) of death with 95% CI. Stata/MP2 (version 13.1; Statacorp, College Station, TX, USA) was used in the analyses. Statistical significance was defined as a P value less than 0.05. Subgroup analysis by sex was performed.
Ethical Considerations
The study was reviewed and approved by Ethics Committee of Korea University.
Results
Patients Characteristics
We identified 14,582 patients who received hepatic resection for BDS during 2002–2016. Of these patients, those with digestive cancers diagnosed more than 3 months prior to the surgery (n = 1564) and HCC (n = 1684), with washout periods (2002–2004, n = 2547), with follow-up durations less than 1 year (n = 692), aged less than 40 years old (n = 231), or with missing data (n = 10) were excluded. A total of 7852 patients were enrolled in this study. The male/female ratio was 2860/4992, and the mean age was 61.36 years. A total of 433 (5.84%) patients were diagnosed with concomitant CCA within a period of 3 months at the time of surgery, and all 7852 patients were followed up (Fig. 1). During the 12-year follow-up, 147 (1.98%) patients were diagnosed with subsequent CCA. A total of 580 out of 7852 (7.39%) patients were diagnosed with HL-CCA. Patients with HL-CCA were predominantly female (P < 0.0001) and older (P < 0.0001) and had a higher mortality than those without it. In addition, patients with subsequent CCA were predominantly female (P = 0.021) and younger (P = 0.026) and had higher proportions of ECC (P < 0.0001) and mortality (P < 0.0001) than those with concomitant CCA (Table 1).
Incidence of Subsequent CCA in Patients with Hepatic Resection for BDS
The incidences of ICC and ECC increased until 10 years after hepatic resection, and plateaued thereafter (Fig. 2). The incidence rates of ICC and ECC were not different between the sexes (Fig. 2). The SIRs were higher than 10 in all CCA (SIR 12.89, 95% CI 10.96–15.15), ICC (13.40, 10.55–17.02) and ECC (12.42, 9.98–15.46) cases. Women had higher SIRs than men. The SIRs gradually decreased with increasing age: 25.21 (40–59 years), 10.53 (60–79 years), and 6.08 (more than 80 years). Women had higher SIRs in cases of ICC (18.68, 13.95–25.02) than ECC (14.63, 10.96–19.53), while men had higher SIRs in the case of ECC (10.31, 7.37–14.43) than ICC (8.49, 5.59–12.90) (Table 2).
Incidence of subsequent cholangiocarcinoma (CCA) in patients with hepatic resection for bile duct stones. The incidences of all CCAs (a), as well as intrahepatic (b), and extrahepatic CCAs (c) gradually increased until 10 years. The incidences of all CCAs (d), and intrahepatic (e) and extrahepatic CCAs (f) were not different between the sexes
Mortality Associated with Concomitant and Subsequent CCA
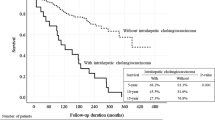
The survival rates of the patients with subsequent CCA were poorer than those with concomitant CCA in all the CCA, ICC, and ECC cases (Fig. 3a–c). Poorer prognoses were observed in the case of both men (Fig. 3d–f) and women (Fig. 3g–i) with subsequent CCA. The median survival time associated with subsequent CCA was 0.87 years, while that of concomitant CCA was 2.79 years. The 5- and 10-year survival rates of subsequent CCA were 13.7% (95% CI, 6.03–24.6) and 6.9% (0.9–22.2), respectively, while those of concomitant CCA were 42.4% (35.3–49.3) and 34.5% (26.8–42.2), respectively. Cox proportional hazard analysis revealed that having subsequent CCA (HR 2.71, 95% CI 2.17–3.40) and being male (HR 1.28, 95% CI 1.05–1.57) were associated with shorter survival times, while the CCA site (ICC versus ECC) and age at CCA diagnosis were not associated with the mortality. These results were consistent in both sexes (Table 3).
The survival rates associated with concomitant and subsequent cholangiocarcinoma (CCA) in patients with hepatic resection for bile duct stones. Subsequent CCA showed lower survival rates than all CCAs (a), and intrahepatic (b) and extrahepatic CCAs (c). These results were consistent in men (d, e, f) and women (g, h, i). CCA, cholangiocarcinoma
Discussion
This is the first nationwide population-based study to analyze the incidence, relative risk, and mortality associated with CCA in patients with hepatic resection for BDS. Subsequent CCA developed in 2% of patients with hepatic resection for benign BDS until 10 years and revealed poorer prognoses than concomitant CCA.
This study showed that CCAs were diagnosed in 433 (5.84%) patients during surgery (concomitant CCA) and in 147 (1.98%) patients after surgery during the 12-year follow-up (subsequent CCA). A total of 7.82% of the preoperative benign HL patients developed CCA. The incidences of concomitant or subsequent CCA in this population-based study were consistent with those observed in previous case–control studies, at 3.3–23.3% [1, 7,8,9] and 1.6–9.9% [1, 4, 7], respectively. Therefore, HL should be treated to prevent CCA, and long-term surveillance is required.
The clinical features and risk factors associated with HL-CCA have been reported. Age higher than 40 years [3], presence of bilateral disease [15], bile duct strictures and liver atrophy [16], duration of symptoms > 10 years [17], and presence of residual stones [18] were reported as risk factors of HL-CCA [19]. The incidences of HL-CCA were highest in 60–79-year-olds, followed by in 40–59-year-olds. Patients aged 80 years revealed the lowest incidences, and none of the patients aged less than 40 years developed HL-CCA. Therefore, 40–80-year-old patients may be candidates for HL-CCA surveillance. Although the incidences of both concomitant and subsequent CCA were higher in the men, the women showed a higher subsequent to concomitant CCA ratio: 1.91% versus 4.39% in women, and 2.12% versus 7.48% in men, respectively.
The present study revealed that the relative risks of CCA differed by age, sex, and cancer location. No previous study has focused on the SIRs of HL-CCA. The SIRs gradually decreased with increasing age. The higher SIRs in the 40–59-year-old group may be attributed to the fact that only a few of these individuals developed CCA. Although the incidence of CCA was higher in men, the SIRs were higher in women. Men have a higher number of risk factors such as the presence of clonorchiasis [20], hepatitis B or C virus infection [21, 22], and Helicobacter pylori infection [23] than women. The effects of HL in women may be greater than in men. In this study, HL after surgery revealed high SIRs for ECC as well as ICC, while the magnitude of the SIRs was higher in cases of ICC than ECC. A recent systemic review [24] and population-based case–control study [25] revealed that the presence of BDS, irrespective of the location, is a risk factor for both ICC and ECC. However, the presence of intrahepatic BDS is a higher relative risk factor for ICC [26] and extrahepatic BDS for ECC [25]. The relative risks for ICC and ECC between the sexes has not been reported before. An interesting finding of our study is that different SIRs in the case of ICC and ECC were observed between the sexes. Women had a higher SIR for ICC than ECC, while men had a higher SIR for ECC than ICC. Further studies need to focus on the causes of the different risks between the sexes, in terms of hormonal, genetic and environmental factors.
The long-term outcomes of patients whose HL and strictures were completely removed were satisfactory. The presence of HL-CCA was an independent prognostic factor in HL patients [27]. The prognosis and clinicopathological features of CCA do not differ, with or without HL [2, 10, 28, 29]. However, the prognoses of concomitant and subsequent CCA are very different. Consistent with the findings of previous studies [12], subsequent CCA was associated with poorer prognoses than concomitant CCA, in the case of both ICC and ECC, and in both sexes in this study. The median survival time and overall survival rates of subsequent and concomitant CCA were 0.87 year versus 2.79 years, and 12.93% versus 39.95%, respectively. Men had marginally poorer prognoses than women, with an HR of 1.28 (95% CI 1.05–1.57). Age and CCA location did not influence the survival time.
The causes of subsequent CCA after the complete treatment of HL are not clearly defined. The presence of recurrent cholangitis, biliary stricture, bile stasis, and chronic bacterial infection are common problems in HL patients [30, 31]. About half of all patients with preoperative benign HL had biliary strictures in the first- or second-order bile duct branches [9]. These recurrent or chronic inflammatory events induce prolonged inflammation of the bile duct epithelium–named “chronic proliferative cholangitis”—which is the main process behind HL-CCA carcinogenesis [32, 33]. Inflammation-mediated signal pathways [34] and epithelial–mesenchymal transition [35] play a major role in biliary fibrosis and biliary carcinogenesis [36]. Surgical specimens of HL-CCA revealed coincidentally detected precancerous lesions such as intraductal papillary neoplasm of the bile duct (IPNB) and biliary intraepithelial neoplasia (BilIN) [9, 37]. One study reported that BilIN or IPNB were present in 12 patients (16.4%) and 1 patient (1.4%) of 73 preoperative benign HL patients, respectively [9]. Precancerous lesions may be present in the residual liver in the absence of residual stones. During follow-up after surgery, precancerous lesions may progress to malignancy.
We considered that most of the BDS cases enrolled in this study involved HL and not common bile duct (CBD) stones. As HL does not have a specific ICD10 code, we defined BDS (ICD 10, K80.0–K80.9) treated with hepatic resection (Q7221–Q7225) as HL. In this study, we defined CCA as ICC or ECC. ICC (C22.1) is defined as a CCA located proximally to the second-degree bile ducts within the liver. ECC (C24.0–C24.9) includes hilar and distal CCA. Hilar CCA is localized to the area between the second-degree bile ducts and the insertion of the cystic duct into the CBD, and distal CCA is confined to the area between the origin of the cystic duct and ampulla of Vater. Subsequent CCA was usually defined as CCA diagnosis after 3–12 months from hepatic resection. In this study, we used a 3-month interval for the diagnosis of subsequent CCA, as CCA is a very aggressive carcinoma and can develop very rapidly.
This study has several strengths. First, we enrolled a large number of patients, based on long-term follow-up data derived from population-based registries. We identified 147 patients with subsequent CCA and analyzed their prognoses; this is the largest sample size in a single study in the existing literature. In addition, we were able to perform an in-depth assessment of the sex-related differences. We evaluated the differences between the sexes in terms of diagnostic age, the SIR, and mortality, and were able to adjust the surveillance strategies between the sexes. Finally, this study analyzed biliary tract cancers according to their location (ICC and ECC). We obtained detailed results on the incidences of and relative risks for ICC and ECC in both sexes.
The limitations of this study include the lack of risk evaluation, as well as its retrospective design. The known risks factors of CCA such as the presence of hepatitis B, hepatitis C, liver cirrhosis, diabetes mellitus, obesity, H. pylori infection, biliary parasitic infection, bile duct cysts and primary sclerosing cholangitis, exposure to certain toxins, alcohol consumption, tobacco smoking, and host genetic polymorphisms were not analyzed in this study [26, 38,39,40]. In South Korea, the regions with higher rate of clonorchiasis revealed increased incidence of CCA [41]. However, in this study, we could not analyze the relations between clonorchiasis and CCA. Another point of view, the effect of ethnic variations in the incidence of CCA was also reported [42]. Although we did not analyze the effects on the incidence of CCA according to different ethnic groups in South Korea, we supposed that the effects were limited. The proportion of other ethnic groups in South Korean was less than 4% [43].
To exclude the coding discrepancies, we selected CCA by ICD-10 code among patients registered in the SSI database. Registration in the SSI program needs a physician’s diagnosis and ensuring by another healthcare professional. In addition, we compared number of patients diagnosed as CCA to Korean Government Cancer Statistics. By these methods, we acquired specificity of CCA coding data. Additionally, some cases of extrahepatic BDS may have been included in this study. We could not distinguish between CBD stones and HL, as the ICD10 code did not allow for the categorization of BDS by site. Nonetheless, a majority of the BDS cases enrolled in this study may be considered as HL cases.
In conclusion, our data revealed an increased risk of CCA following hepatic resection for BDS until a period of 10 years. The SIR was higher in cases of ECC as well as ICC, and was higher in women. As subsequent CCA is associated with very poor prognoses compared to concomitant CCA, surveillance for the occurrence of CCA after curative treatment for HL should be considered. Further studies should focus on the indications and methods of surveillance in such patients.
References
Kim HJ, Kim JS, Joo MK, et al. Hepatolithiasis and intrahepatic cholangiocarcinoma: a review. World J Gastroenterol. 2015;21:13418–13431.
Catena M, Aldrighetti L, Finazzi R, et al. Treatment of non-endemic hepatolithiasis in a Western country. The role of hepatic resection. Ann R Coll Surg Engl. 2006;88:383–389.
Kim YT, Byun JS, Kim J, et al. Factors predicting concurrent cholangiocarcinomas associated with hepatolithiasis. Hepatogastroenterology. 2003;50:8–12.
Tsuyuguchi T, Miyakawa K, Sugiyama H, et al. Ten-year long-term results after non-surgical management of hepatolithiasis, including cases with choledochoenterostomy. J Hepatobiliary Pancreat Sci. 2014;21:795–800.
Suzuki Y, Mori T, Yokoyama M, et al. Hepatolithiasis: analysis of Japanese nationwide surveys over a period of 40 years. J Hepatobiliary Pancreat Sci. 2014;21:617–622.
Li SQ, Liang LJ, Peng BG, et al. Hepaticojejunostomy for hepatolithiasis: a critical appraisal. World J Gastroenterol. 2006;12:4170–4174.
Lee TY, Chen YL, Chang HC, Chan CP, Kuo SJ. Outcomes of hepatectomy for hepatolithiasis. World J Surg. 2007;31:479–482.
Tabrizian P, Jibara G, Shrager B, Schwartz ME, Roayaie S. Hepatic resection for primary hepatolithiasis: a single-center Western experience. J Am Coll Surg. 2012;215:622–626.
Park HM, Hur YH, Cho CK, Koh YS, Kim HJ, Park EK. Incidence of underlying biliary neoplasm in patients after major hepatectomy for preoperative benign hepatolithiasis. Ann Hepatobiliary Pancreat Surg. 2016;20:173–179.
Lee CC, Wu CY, Chen GH. What is the impact of coexistence of hepatolithiasis on cholangiocarcinoma? J Gastroenterol Hepatol. 2002;17:1015–1020.
Chen DW, Tung-Ping Poon R, Liu CL, Fan ST, Wong J. Immediate and long-term outcomes of hepatectomy for hepatolithiasis. Surgery. 2004;135:386–393.
Lin CC, Lin PY, Chen YL. Comparison of concomitant and subsequent cholangiocarcinomas associated with hepatolithiasis: clinical implications. World J Gastroenterol. 2013;19:375–380.
Kim HJ, Kim JS, Suh SJ, et al. Cholangiocarcinoma risk as long-term outcome after hepatic resection in the hepatolithiasis patients. World J Surg. 2015;39:1537–1542.
Hong SN, Kim HJ, Kim KH, Han SJ, Ahn IM, Ahn HS. Risk of incident Mycobacterium tuberculosis infection in patients with inflammatory bowel disease: a nationwide population-based study in South Korea. Aliment Pharmacol Ther. 2017;45:253–263.
Li SQ, Liang LJ, Peng BG, et al. Outcomes of liver resection for intrahepatic stones: a comparative study of unilateral versus bilateral disease. Ann Surg. 2012;255:946–953.
Suzuki Y, Mori T, Abe N, et al. Predictive factors for cholangiocarcinoma associated with hepatolithiasis determined on the basis of Japanese Multicenter study. Hepatol Res. 2012;42:166–170.
Liu ZY, Zhou YM, Shi LH, Yin ZF. Risk factors of intrahepatic cholangiocarcinoma in patients with hepatolithiasis: a case-control study. Hepatobiliary Pancreat Dis Int. 2011;10:626–631.
Meng ZW, Han SH, Zhu JH, Zhou LY, Chen YL. Risk Factors for Cholangiocarcinoma after initial hepatectomy for intrahepatic stones. World J Surg. 2017;41:835–843.
Park JS, Jeong S, Lee DH, et al. Risk factors for longterm outcomes after initial treatment in hepatolithiasis. J Korean Med Sci. 2013;28:1627–1631.
Jeong YI, Shin HE, Lee SE, et al. Prevalence of clonorchis sinensis infection among residents along 5 major rivers in the Republic of Korea. Korean J Parasitol. 2016;54:215–219.
Park B, Jung KW, Oh CM, Choi KS, Suh M, Jun JK. Ten-year changes in the hepatitis B prevalence in the birth cohorts in Korea: results from nationally representative cross-sectional surveys. Medicine (Baltimore). 2015;94:e1469.
Shon HS, Choi HY, Kim JR, et al. Comparison and analysis of the prevalence of hepatitis C virus infection by region in the Republic of Korea during 2005–2012. Clin Mol Hepatol. 2015;21:249–256.
Lim SH, Kwon JW, Kim N, et al. Prevalence and risk factors of Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol. 2013;13:104.
Bergquist A, von Seth E. Epidemiology of cholangiocarcinoma. Best Pract Res Clin Gastroenterol. 2015;29:221–232.
Welzel TM, Graubard BI, El-Serag HB, et al. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based case-control study. Clin Gastroenterol Hepatol. 2007;5:1221–1228.
Cai H, Kong WT, Chen CB, et al. Cholelithiasis and the risk of intrahepatic cholangiocarcinoma: a meta-analysis of observational studies. BMC Cancer. 2015;15:831.
Uenishi T, Hamba H, Takemura S, et al. Outcomes of hepatic resection for hepatolithiasis. Am J Surg. 2009;198:199–202.
Chen MF, Jan YY, Hwang TL, et al. Impact of concomitant hepatolithiasis on patients with peripheral cholangiocarcinoma. Dig Dis Sci. 2000;45:312–316.
Guglielmi A, Ruzzenente A, Valdegamberi A, et al. Hepatolithiasis-associated cholangiocarcinoma: results from a multi-institutional national database on a case series of 23 patients. Eur J Surg Oncol. 2014;40:567–575.
Fan ST, Wong J. Complications of hepatolithiasis. J Gastroenterol Hepatol. 1992;7:324–327.
Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009;146:843–853.
Nakanuma Y, Terada T, Tanaka Y, Ohta G. Are hepatolithiasis and cholangiocarcinoma aetiologically related? A morphological study of 12 cases of hepatolithiasis associated with cholangiocarcinoma. Virchows Arch A Pathol Anat Histopathol. 1985;406:45–58.
Li FY, Cheng NS, Mao H, et al. Significance of controlling chronic proliferative cholangitis in the treatment of hepatolithiasis. World J Surg. 2009;33:2155–2160.
Zhou Q, Gong Y, Huang F, et al. Expression levels and significance of nuclear factor-κB and epidermal growth factor receptor in hepatolithiasis associated with intrahepatic cholangiocarcinoma. Dig Surg. 2013;30:309–316.
Sung R, Lee SH, Ji M, et al. Epithelial-mesenchymal transition-related protein expression in biliary epithelial cells associated with hepatolithiasis. J Gastroenterol Hepatol. 2014;29:395–402.
Tajima Y, Kanematsu T. Hepatolithiasis and intrahepatic cholangiocarcinoma: carcinogenesis based on molecular mechanisms. J Hepato Biliary Pancreat Surg. 2005;12:463–466.
Ohta T, Nagakawa T, Ueda N, et al. Mucosal dysplasia of the liver and the intraductal variant of peripheral cholangiocarcinoma in hepatolithiasis. Cancer. 1991;68:2217–2223.
Chang JS, Tsai CR, Chen LT. Medical risk factors associated with cholangiocarcinoma in Taiwan: a population-based case–control study. PLoS ONE. 2013;8:e69981.
Palmer WC, Patel T. Are common factors involved in the pathogenesis of primary liver cancers? A meta-analysis of risk factors for intrahepatic cholangiocarcinoma. J Hepatol. 2012;57:69–76.
Tyson GL, El-Serag HB. Risk factors for cholangiocarcinoma. Hepatology. 2011;54:173–184.
Lim MK, Ju YH, Franceschi S, et al. Clonorchis sinensis infection and increasing risk of cholangiocarcinoma in the Republic of Korea. Am J Trop Med Hyg. 2006;75:93–96.
Antwi SO, Mousa OY, Patel T. Racial, ethnic, and age disparities in incidence and survival of intrahepatic cholangiocarcinoma in the United States; 1995–2014. Ann Hepatol. 2018;17:604–614.
Korean Statistical Information Service. Population by Census, 2016. http://kosis.kr/eng/. Accessed August 8, 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no potential conflicting interests related to this paper.
Rights and permissions
About this article
Cite this article
Kim, H.J., Kang, T.U., Swan, H. et al. Incidence and Prognosis of Subsequent Cholangiocarcinoma in Patients with Hepatic Resection for Bile Duct Stones. Dig Dis Sci 63, 3465–3473 (2018). https://doi.org/10.1007/s10620-018-5262-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5262-6