Abstract
Background
Main concern during the practice of selective non-operative management (SNOM) for abdominal stab wounds (SW) and gunshot wounds (GSW) is the potential for harm in patients who fail SNOM and receive a delayed laparotomy (DL). The aim of this study is to determine whether such patients suffer adverse sequelae because of delays in diagnosis and treatment when managed under a structured SNOM protocol.
Methods
190 patients underwent laparotomy after an abdominal GSW or SW (5/04–10/12). Patients taken to operation within 120 min of admission were included in the early laparotomy (EL) group (n =153, 80.5 %) and the remaining in the DL group (n =37, 19.5 %). Outcomes included mortality, hospital stay, and postoperative complications.
Results
The median time from hospital arrival to operation was 43 min (range: 17–119) for EL patients and 249 min (range: 122–1,545) for DL patients. The average number and type of injuries were similar among the groups. Mortality and negative laparotomy were observed only in the EL group. There was no significant difference in the hospital stay between the groups. The overall complications were higher in the EL group (44.4 vs. 24.3 %, p =0.026). DL was independently associated with a lower likelihood for complications (OR 0.39, 95 % CI 0.16–0.98, p =0.045). Individual review of all DL patients did not reveal an incident in which complications could be directly attributed to the delay.
Conclusions
In a structured protocol, patients who fail SNOM and require an operation are recognized and treated promptly. The delay in operation does not cause unnecessary morbidity or mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The emergence of “selective conservatism” as an alternative to routine laparotomy for penetrating abdominal injuries [1, 2] laid the cornerstones of a new therapeutic approach in trauma surgery. A large body of literature from South Africa and the U.S. reported encouraging results with selective non-operative management (SNOM) for abdominal stab wounds (SW) and gunshot wounds (GSW) [3–7]. SNOM has been shown to decrease the rate of unnecessary laparotomies, shorten hospital stay, and produce significant cost savings [7].
SNOM is an active process and may switch to a laparotomy if the hemodynamic condition or the abdominal clinical exam changes [8]. For those patients who “fail” SNOM and eventually require surgical intervention, there is concern that the delay in treatment may cause significant complications. This study evaluated the outcome of SW and GSW patients who were initially managed non-operatively but later needed a laparotomy. We hypothesized that if SNOM is offered properly under a structured protocol, such delays do not lead to adverse events.
Materials and methods
Patients
After Institutional Review Board approval, the medical records of all SW and GSW patients, who received a laparotomy at the Massachusetts General Hospital, an academic Level 1 Trauma Center, from May 1 2004 through October 31 2012 were reviewed. Patients who underwent an emergency room thoracotomy or died shortly after arrival were excluded. Throughout this period, the Trauma Center was covered around the clock by a trauma team, including in-house trauma attending surgeons.
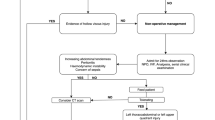
Clinical protocol
A structured SNOM protocol was used to determine the appropriate patients for non-operative treatment. In the presence of hemodynamic instability, diffuse abdominal tenderness, and evisceration, an immediate operation was offered. All other patients were considered eligible for SNOM. Abdominal computed tomography (CT) was used liberally in SNOM patients. Whereas initially some non-evaluable patients were managed by an immediate laparotomy, we gradually switched to SNOM with the assistance of CT for all such patients. CT images were interpreted by an attending radiologist (covering the Trauma Center 24/7) in the presence of the attending trauma surgeon.
SNOM patients were admitted to a dedicated observation unit and monitored closely for 12–24 h. Serial clinical exams were performed in frequent intervals according to the patient’s acuity and at minimum every 4 h. Although the preferred course required the same physician (attending and/or senior resident) to perform the serial exams, this was not always feasible when the day and night float teams changed. However, a detailed “pass-off” was part of the routine and the two teams (outgoing and incoming) performed one clinical exam together to ensure they agree on the findings. After the period of observation in the dedicated unit, the patients were either moved to a regular ward bed or discharged. If during the observation period the patient either developed diffuse abdominal tenderness or hemodynamic deterioration, the team would promptly proceed to an operation without further imaging. More subtle signs such as persistent but only local abdominal tenderness, vomiting after food challenge, or mild persistent tachycardia without any episodes of hypotension were considered on a case-by-case basis.
Definitions
Patients taken to operation within 120 min of admission were included in the early laparotomy (EL) group and the remaining in the delayed laparotomy (DL) group, indicating patients who were initially offered SNOM. This 2-h limit was set arbitrarily on the basis of our center’s infrastructure, which allows immediate access to resources such as CT and OR. Our established practice has been to take patients with penetrating injuries immediately to operation if the decision is made based on clinical symptoms and signs. Even if a CT was considered as part of the initial decision-making, this was immediately available and typically completed within less than 20 min. Therefore, it was assumed that if a patient was not taken to the OR within 2 h, a deliberate decision was made against immediate laparotomy. In parallel to this time points, we evaluated the medical records to ensure that the notes were consistent with our classification to EL or DL, and there was no reason for DL other than an initial decision to manage the patient non-operatively.
Data and outcomes
Data were collected on the following variables: Age, Gender, Injury Severity Score, Abbreviated Injury Scale for the abdomen, type of injury (GSW or SW), interval from hospital arrival to the operating room (OR), vital signs and clinical exam on admission and before surgery, blood products transfused, imaging procedures, operations, morbidity, mortality, and intensive care unit and hospital stay.
EL and DL were compared. Outcomes included postoperative complications, mortality, and hospital length of stay. Complications were grouped according to the Clavien–Dindo classification [9]. If patients had multiple complications, they were assigned the grade of the most severe complication. The medical records of all DL patients were screened in detail to evaluate if any complication was related to the delay.
Statistical analysis
Data were summarized as means ±SD, if normally distributed, as medians with interquartiles, if abnormally distributed, or as frequencies (%) when appropriate. Two-sample t-tests, Wilcoxon rank sum tests, or Fisher’s exact tests were used to compare continuous or categorical variables. Multivariable analyses using linear and logistic regression models were performed in order to determine the effect of the timing of laparotomy on outcomes controlling for other risk factors as well as to identify independent predictors for the outcomes. Analyzes were repeated stratified by type of injury. All analyzes were conducted using SAS version 9.3 (The SAS Institute, Cary, NC). A p value < 0.05 was considered statistically significant.
Results
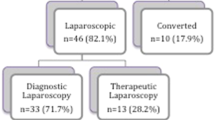
Of 190 SW and GSW patients, who underwent laparotomy, 153 (80.5 %) were included in the EL group with a median time of 43 min (range: 17–119 min) from arrival to the Emergency Department until arrival to the OR. The remaining 37 (19.5 %) patients were included in the DL group with a median time to operation of 249 min (range: 122–1545 min).
Table 1 compares the two groups. There were no differences in demographics, injury severity, and admission hemodynamics. As expected, EL patients had a higher frequency of positive abdominal ultrasonographic exams and a greater intraoperative blood loss and blood transfusion.
Table 2 describes the reasons for laparotomy and the different type of injuries. There was a higher incidence of GSW compared to SW among EL patients than DL patients. Hypotension and diffuse abdominal tenderness on admission were common reasons for operation among EL patients. In the majority of the cases, the decision for laparotomy in DL patients was based on imaging studies or development of peritonitis during observation. Only 3 DL patients developed hypotension during observation. Two of those patients became transiently hypotensive. On exploration, one had a liver laceration and the other an omental bleeding vessel; both had small amounts of hemoperitoneum and the injuries were easily controlled. The third patient was brought to the operating room due to hypotension from an increasing chest tube output. There were no differences in the type or number of organ injuries between the two groups. Non-therapeutic laparotomies were performed only in the EL group (n =5, 3.3 %).
The different outcomes are presented in Table 3. More EL patients developed complications overall (44.4 vs. 24.3 %, p =0.026). Major complications (grade 3, 4, and 5) occurred in 28.8 % of EL patients compared to 18.9 % of DL patients, but the difference did not achieve statistical significance. ICU and hospital stays were not different between the two groups; mortality was not different either, although all 5 patients who died belonged to the EL group.
Complications developed in 9 DL patients and are described in Table 4. These complications were reviewed in detail and none was felt to be a result of the delay in treatment. No DL patient had an anastomotic leak, sepsis, septic shock, or multi-organ failure. Additionally, there was no significant difference in the median hospital length of stay between the patients, who developed complications in the DL and EL groups (7.0 vs. 5.5 days, p =0.09).
The results of the multivariable analysis are summarized in Table 5. No predictors of mortality were identified due to the small number of patients who did not survive their injuries. DL was independently associated with a lower likelihood for any complication and for severe complications. However, the patients in the DL group were more likely to stay in the hospital for more than 5 days.
Figure 1 captures the development of complications according to the intervals from hospital arrival to OR arrival. As this interval increased, the percentage of patients who developed postoperative complications decreased.
Discussion
In a Level 1 Trauma Center with a structured policy of SNOM for patients with penetrating abdominal trauma, patients who failed SNOM and eventually required a laparotomy did not suffer unnecessary morbidity or mortality. This data support the use of SNOM and eases the unjustified fear of worse prognosis and potential for harm, often given as a reason to avoid a trial of SNOM.
SNOM has a long history but a slow penetration in the practices of surgeons. Although certain groups dealing with high penetrating trauma volumes repeatedly showed excellent results [4, 8, 10], many other groups remained skeptical [11–14]. The skepticism was greater for abdominal GSW even if older [7] and more recent [15] studies have argued that SNOM is safe. Two of the most frequent arguments against SNOM claimed that: (1) a non-therapeutic laparotomy carries minimal risk and (2) a delay of a therapeutic laparotomy carries significant risk. The first argument has been proven wrong. Non-therapeutic laparotomies are associated with complications, which are as high as 14.5 and 41.3 % in retrospective and prospective studies, respectively [16, 17]. The second argument became the objective of our study.
In two prospective studies [4, 18] of abdominal GSW, the rate of DL was 13.2 and 3 %, respectively. In these studies, DL patients did not suffer adverse sequelae related to the delay. In the largest review of abdominal GSW to date with 1,856 GSW to the abdomen [7], 80 patients received DL and 5 of them developed complications which could be attributed to the delay. They were all managed successfully and none resulted in mortality. Other authors have shown different results. A recent retrospective study based on the National Trauma Data Bank showed that failure of SNOM with consecutive need for DL was independently associated with increased mortality in both GSW (OR 4.48) and SW (OR 9.83) patients [11].
In our study, nearly 1 out of every 5 patients with a laparotomy for a penetrating abdominal injury was initially managed by SNOM. Worrisome imaging findings in combination with the development of clinical symptoms prompted a laparotomy at a median of 4 h and as late as 26 h after arrival. Nine DL patients developed a complication and 7 of them were classified as grade 3, 4, or 5. Although judgments about causation are hard to make retrospectively, we examined each case in detail and with the intent to assign causation to the delay liberally if any suspicion arose. There were two patients who developed intra-abdominal abscesses and one could claim that the even the short delays in operating them (128 and 146 min, respectively) may have encouraged the development of the complication. However, the operative report described minimal contamination, and therefore this claim could not be made with confidence.
DL showed an independent association with fewer complications despite a slight increase in the median hospital LOS. As the interval from hospital arrival to operation increased, the rate of complications decreased, attesting to the fact that sicker patients were correctly chosen for an operation from the beginning, whereas stable and asymptomatic patients were correctly selected for a period of observation.
A number of limitations mitigate the power of our conclusions. The retrospective nature of the study prevented valid assessments on causation, as mentioned above. The sample size is limited but typical of most trauma centers around the country, which have experienced a decline in penetrating trauma volumes. Most importantly, the delays are short. In fact, the definition of a delay in this study can be debated since the word “delay” carries negative connotations and possibly considered to indicate inadequate diligence and care. This has not been our intent. We wanted to emphasize that, in the absence of compelling signs and symptoms consistent with significant intra-abdominal injuries, offering a trial of SNOM is safe. Typically, if such injuries exist, the combination of imaging studies and an evolving clinical exam will reveal the need for laparotomy soon after the admission.
The safety of SNOM is based on close clinical observation and frequent clinical exams. As simple as this sound, it requires that the entire trauma team, including doctors, nurses, and physician extenders, are informed about the anticipated signs and symptoms that could indicate the failure of NOM. In a well-organized setting, the team should be able to identify promptly any early changes in the hemodynamic status or abdominal exam. It is because of this infrastructure and shared mindset among the trauma team members that patients who failed NOM in our study were brought to the operating room within a very short period of time avoiding unnecessary delays.
The point of our study is not to claim that missing injuries and failing to recognize the need for surgical intervention is justifiable. It is rather to argue that under a structured protocol of SNOM, patients in need for an operation are identified and treated promptly. We argue that an injury that does not produce symptoms which does not produce immediate harm. When symptoms develop, action should be taken, and it is up to the acute care surgeon and an organized support system to recognize this moment quickly.
SNOM in abdominal penetrating injuries should not be the exclusive privilege of high-volume trauma centers. We have previously shown that it is the system and commitment rather than the volume of penetrating trauma patients that sets the foundation for safe SNOM [15]. With dwindling penetrating trauma volumes around the nation, most trauma centers cannot count on the experience of daily trauma laparotomies. Nevertheless, they can develop successful policies that allow the right patients to receive the right operation and those who do not need one to receive none. Our study adds to the existing body of literature about the safety of SNOM in abdominal SW and GSW. It specifically targets the issue of potential harm of DL when SNOM fails. It shows that a structured protocol of SNOM in a Level 1 Trauma Center does not risk unnecessary complications and can be safely offered in patients with penetrating abdominal trauma.
References
Shaftan GW (1969) Selective conservatism in penetrating abdominal trauma. J Trauma 9:1026–1028
McAlvanah MJ, Shaftan GW (1978) Selective conservatism in penetrating abdominal wounds: a continuing reappraisal. J Trauma 18:206–212
Demetriades D, Charalambides D, Lakhoo M et al (1991) Gunshot wound of the abdomen: role of selective conservative management. Br J Surg 78:220–222
Demetriades D, Velmahos G, Cornwell E 3rd et al (1997) Selective nonoperative management of gunshot wounds of the anterior abdomen. Arch Surg 132:178–183
Velmahos GC, Demetriades D, Cornwell EE 3rd (1998) Transpelvic gunshot wounds: routine laparotomy or selective management? World J Surg 22:1034–1038
Velmahos GC, Demetriades D, Foianini E et al (1997) A selective approach to the management of gunshot wounds to the back. Am J Surg 174:342–346
Velmahos GC, Demetriades D, Toutouzas KG et al (2001) Selective nonoperative management in 1,856 patients with abdominal gunshot wounds: should routine laparotomy still be the standard of care? Ann Surg 234:395–402 discussion 402–393
Como JJ, Bokhari F, Chiu WC et al (2010) Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma 68:721–733
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Laing GL, Skinner DL, Bruce JL et al (2014) A multi faceted quality improvement programme results in improved outcomes for the selective non-operative management of penetrating abdominal trauma in a developing world trauma centre. Injury 45:327–332
Zafar SN, Rushing A, Haut ER et al (2012) Outcome of selective non-operative management of penetrating abdominal injuries from the North American National Trauma Database. Br J Surg 99(Suppl 1):155–164
Hope WW, Smith ST, Medieros B et al (2012) Non-operative management in penetrating abdominal trauma: is it feasible at a Level II trauma center? J Emerg Med 43:190–195
Moore EE, Moore JB, Van Duzer-Moore S et al (1980) Mandatory laparotomy for gunshot wounds penetrating the abdomen. Am J Surg 140:847–851
Lowe RJ, Saletta JD, Read DR et al (1977) Should laparotomy be mandatory or selective in gunshot wounds of the abdomen? J Trauma 17:903–907
Fikry K, Velmahos GC, Bramos A et al (2011) Successful selective nonoperative management of abdominal gunshot wounds despite low penetrating trauma volumes. Arch Surg 146:528–532
Sosa JL, Arrillaga A, Puente I et al (1995) Laparoscopy in 121 consecutive patients with abdominal gunshot wounds. J Trauma 39:501–504 discussion 504–506
Schnuriger B, Lam L, Inaba K et al (2012) Negative laparotomy in trauma: are we getting better? Am Surg 78:1219–1223
Velmahos GC, Demetriades D, Cornwell EE et al (1997) Gunshot wounds to the buttocks: predicting the need for operation. Dis Colon Rectum 40:307–311
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Peev, M.P., Chang, Y., King, D.R. et al. Delayed Laparotomy After Selective Non-operative Management of Penetrating Abdominal Injuries. World J Surg 39, 380–386 (2015). https://doi.org/10.1007/s00268-014-2813-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2813-7