Abstract
Background
In 2010, the Japanese Society of Thyroid Surgeons (JSTS) and Japanese Association of Endocrine Surgeons (JAES) established new guidelines entitled “Treatment of Thyroid Tumors.” Since then, several new studies, including those that address the treatment of differentiated thyroid carcinoma (DTC) have been published, and the DTC treatment policy not only of Japanese physicians but those in Western countries has continued to evolve.
Methods
We selected six clinical questions regarding the treatment of DTC and revisited them based on newly published data from Western countries and Japan.
Results
More data have accumulated about treatment of low-risk papillary microcarcinoma. It has become clear that conservative treatment (observation) of low-risk papillary microcarcinoma in elderly patients is an acceptable alternative to immediate surgery. Total thyroidectomy versus hemithyroidectomy for low-risk papillary thyroid carcinoma (PTC) has become an important issue, and some publications after 2010 indicated that hemithyroidectomy is adequate for these low-risk patients. Unfortunately, no published manuscripts on prophylactic central node dissection offered good evidence regarding its indications or included a large number of patients. Also, it was not evident that prophylactic lateral node dissection improves cause-specific survival, although it might reduce lymph node recurrence especially in PTC patients with large tumors, distant metastases, or clinical central node metastases. Although completion total thyroidectomy was not recommended for minimally invasive follicular thyroid carcinoma in our guidelines, it may be better to perform it in elderly patients and those with a large tumor or extensive vascular invasion. Radioactive iodine (RAI) ablation after total thyroidectomy is still performed almost routinely in many Western institutions, although recent studies showed that ablation is not beneficial in low-risk patients. In Japan, because of legal restrictions, most patients did not undergo RAI ablation, and their prognoses are excellent.
Conclusions
Recently, policy for treating DTCs has changed not only in Western countries but also in Japan, resulting in a gradual move toward consensus between Western practice and ours. We will continue to present the best treatments for patients with thyroid carcinoma each time we revise our guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2010, the Japanese Society of Thyroid Surgeons (JSTS) and Japanese Association of Endocrine Surgeons (JAES) newly established “Treatment of Thyroid Tumor” guidelines. In addition, an English version and an extract of the guidelines for treating differentiated thyroid carcinoma (DTC) were published [1, 2]. The treatment strategies used in Japan for DTC have differed markedly from those in Western countries. Most Western institutions still perform total thyroidectomy followed by radioactive iodine (RAI) ablation regardless of the degree of progression. In Japan, we do not routinely perform total thyroidectomy, and routine RAI ablation is not possible because of legal restrictions. Despite these differences, the prognosis for Japanese patients with DTC is excellent.
It is true that some Japanese surgeons are not familiar with the concept of evidence-based standard therapy for thyroid surgery. Therefore, the goals of the new DTC guidelines are to unify standard treatments for thyroid tumor (especially thyroid carcinoma), educate Japanese surgeons about these standard treatments, and more importantly distribute information about our successful treatment outcomes to the world. We also introduced an observation guide for low-risk papillary microcarcinoma (PMC), which is papillary thyroid carcinoma (PTC) measuring ≤1 cm). In Japan, PMCs are treated by a method that is not yet performed in other countries.
Nearly 4 years have passed since our new guidelines were published, and the attitudes of both Western and Japanese surgeons and endocrinologists have changed by degrees since then. In Japan, RAI ablation using 30 mCi is permitted in outpatient clinics, and recombinant human thyroid stimulating hormone (rhTSH) is currently an option for use with RAI ablation. In contrast, as we discuss later, some Western endocrine surgeons and endocrinologists have expressed doubts about their standard therapy for DTC (i.e., routine total thyroidectomy with RAI ablation).
In this review, we revisit the 2010 JSTS/JAES guidelines, take up matters of special importance, and consider whether and how the wording of the guidelines should be changed in light of recent findings. We also introduce new knowledge from Western countries and Japan published after the guidelines’ debut, to consider whether and how the treatment guidelines should change on a worldwide scale. We describe some of these changes in the form of clinical questions (CQ).
Can simple observation be used for low-risk PMC? (CQ20)
“Low-risk” indicates the lack of distant metastases (M1 in the TNM classification), clinical node metastases (N1), and symptomatic manifestations (T4a) (e.g., recurrent laryngeal nerve paralysis) based on preoperative findings. To date, two institutions in Japan have actively performed observation for low-risk PMC, with favorable outcomes [3, 4]. The procedure was adopted and included in the 2010 guidelines based on their achievements. Since then, two additional manuscripts have been published from these institutions: Sugitani et al. [5] demonstrated the lack of a relation between thyroid-stimulating hormone (TSH) and PMC progression. Ito et al. [6] investigated the natural course of 1,235 cases of PMC. They found that PMCs were most likely to progress in young patients (<40 years), and the PMCs in those aged ≥60 years were mostly stable. The multivariate analysis in that study revealed that young age is an independent predictor of PMC progression [6].
These findings indicated that low-risk PMCs in old patients are the best candidates for observation. Interestingly, this observation-only concept is in sharp contrast with the fact that old age is one of the most significant prognostic factors for carcinoma-caused death [7]. The most important point here is that, as of this moment at both of the above-mentioned institutions, none of the patients has shown distant metastases or died of PTC during observation or after surgery that was conducted when a progression sign such as size enlargement and/or novel appearance of node metastasis was detected. Therefore, observation without immediate surgery can be a good alternative in low-risk PMC cases. The recent results of the two institutions regarding low-risk PMC observation are summarized in Table 1.
In some Western countries, ultrasonography is costly, and repeated visits to thyroid specialist clinics are difficult for some patients because of the distance (there are relatively few of these clinics). Another problem is that the ethics committees of individual hospitals may not allow physicians to implement observation alone in light of the perceived risk. These various circumstances might prevent this strategy from spreading to other countries and even to many institutions in Japan.
At least in Japan, however, we have accumulated data over a two-decade span for a large number of patients. Fortunately, ultrasonography has been economical at these facilities. Based on their successful outcomes, we can recommend observation by ultrasonography without immediate surgery to patients as a dominant alternative to low-risk PMC therapy. We have found that this strategy is beneficial for many patients and hope that it will be adopted worldwide in the near future.
As thyroid carcinoma was found in 3.5 % of otherwise healthy women by ultrasonography [8], surgery for all low-risk PMC patients is definitely overtreatment. Also, a policy of surgery for all such patients would soon exceed the capacity of thyroid surgeons when mass screenings by thyroid ultrasonography become more common. It is time for all endocrinologists and endocrine surgeons around the world to seriously reconsider whether all incidentally detected (by ultrasonography) PMCs should be treated surgically based on the data presented here.
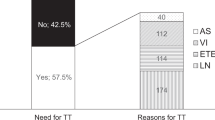
What are the indications for total thyroidectomy from the aspect of improving the prognosis of PTC patients? (CQ17)
In the 2010 JSTS/JAES guidelines, total thyroidectomy was strongly or moderately recommended for PTC patients with tumors >4 cm, clinical node metastasis (N1), distant metastasis (M1), or extrathyroid extension (Ex) to the trachea or esophagus. These indications are much narrower than those in Western guidelines such as those issued by the American Thyroid Association (ATA) [9], British Thyroid Association (BTA) [10], National Comprehensive Cancer Network (NCCN) in the United States [11], and the American Association of Clinical Endocrinologists (AACE)/American Association of Endocrine Surgeons (AAES) [12]. A revised version of the German Association of Endocrine Surgeons (GAES) practice guideline was recently published [13], in which routine total thyroidectomy is described as warranted for PTCs >10 mm.
Ito et al. [14] demonstrated that in a series of 2,638 patients with solitary T1N0M0 PTCs the 10-year disease-free survival (DFS) rate was very high, at 97 %, and only 0.4 and 0.2 % of patients showed a distant recurrence and died of PTC, respectively. They also showed that the prognosis of T1b cases (tumor size 1.1–2.0 cm) did not differ from that of T1a cases (size ≤ 1 cm) [14]. In addition, in a series of N0M0Ex(−) patients, the 10-year distant recurrence-free survival rates were 0.4 % for tumors ≤2 cm, 1.6 % for those 2.1–4.0 cm, and 3.4 % for those >4.0 cm [15].These numbers indicate that such “otherwise low-risk patients” do not frequently show distant recurrence requiring RAI therapy. Therefore, although the distant recurrence rates increased with tumor size, total thyroidectomy might not be mandatory for these patients.
More recently, Matsuzu et al. [16] investigated the prognosis of 1,088 PTC patients who underwent lobectomy and were followed up for a median of 17.6 years. They demonstrated that none of the patients without the four risk factors (age ≥ 45 years, tumor size > 4 cm, presence of clinical node metastasis [N1], and extrathyroid extension died of PTC, whereas the 22 patients who died of PTC were positive for one or more of these four factors. Those authors thus concluded that lobectomy is a valid alternative to total thyroidectomy for treating PTC patients who are <45 years with tumors measuring ≤4 cm and a lack of both clinical node metastasis and extrathyroid extension. Table 2 summarizes the prognosis of the N0M0Ex(−) patients in these two recent studies.
Total thyroidectomy has a great advantage in that thyroglobulin (Tg) can be used as a tumor marker. Also, the postoperative Tg doubling time is a useful parameter for predicting patients’ cause-specific survival (CSS) [17]. Moreover, recurrence (especially distant recurrence) is easily detected, and immediate RAI therapy can be performed. However, if total thyroidectomy is performed by a nonexpert severe complications may occur, such as bilateral recurrent laryngeal nerve paralysis and persistent hypoparathyroidism. Our guidelines were not established for experts in thyroid surgery, and the balance between the merits and demerits of a given therapy must be considered when CQs are to be addressed.
Thus, the indications for total thyroidectomy described in the 2010 JSTS/JAES guidelines are appropriate at least in Japan, an iodine-rich country. The indications may also be applicable for Western countries, although more data accumulation is necessary among western patients before any conclusion can be drawn.
Is prophylactic central node dissection beneficial? (CQ18)
The most useful tool for detecting lymph node metastasis preoperatively is ultrasound, but the diagnostic accuracy of ultrasonography for central node metastasis is not high: The reported negative predictive value and sensitivity were 37 and 12 %, respectively [18], indicating that ultrasonography frequently overlooks small and latent central node metastasis. In addition, when the recurrence manifests clinically, reoperation of the central compartment may result in severe complications such as recurrent laryngeal nerve injury and persistent hypoparathyroidism. For such cases, the 2010 JSTS/JAES guidelines recommend routine bilateral central node dissection (CND) in patients who undergo total thyroidectomy. Ito et al. [19] showed that on multivariate a tumor size >2 cm was the strongest predictor of micro-lymph node metastasis and recurrence of N0 PTC, indicating that careful prophylactic CND is preferable, especially for large PTCs.
There are pros and cons for routine prophylactic CND for PTC patients. The present ATA guideline does not recommend routine CND. Its indication is limited to T3 or T4 patients based on expert opinion [9]. Conzo et al. [20] also proposed that the indication of CND might be limited to high-risk patients in whom nodal recurrence is more frequent because only 3.75 % of N0 patients showed lymph node recurrence even though they did not undergo prophylactic CND. Monchik et al. [21] demonstrated that failure to conduct prophylactic CND in low-risk PTC cases resulted in a very low incidence (1.8 %) of persistent nodal disease and elevated Tg levels 4–6 months after surgery, but they did not report the disease-free survival (DFS) or CSS rates over a long-term follow-up. Yoo et al. [22] showed that CND did not reduce the uptake of 131I, and the preablation Tg level did not depend on whether CND was performed (0.93 vs. 1.2 %; p = 0.17). According to a study by Lang et al [23]., CND offers a more complete initial tumor resection than total thyroidectomy alone by evaluating the stimulated Tg (p = 0.020), but the difference becomes less noticeable 6 months after ablation (p = 0.292). Moreno et al. [24] performed a retrospective chart review and showed that prophylactic CND did not improve overall survival (p = 0.32), disease-specific survival (p = 0.49), or recurrence-free survival (p = 0.32) regardless of the histopathologic status of the lymph node retrieved.
In contrast, routine CND has been recommended by several studies, mainly because it is useful for accurate staging and for choosing the appropriate dose of 131I for ablation. Prophylactic CND and lateral node dissection were recommended by Hartl et al. [25] because patients staged pN0 received less 131I than those staged pN1 (median 30 vs. 100 mCi, p < 0.0001). Following a series of patients who underwent prophylactic bilateral CND, Laird et al. reported that the pathologically node-positive patients were more likely to show detectable Tg levels and require a higher dose of 131I (150 vs. 30 mCi, p < 0.001) [26]. Similar findings were reported by others [27, 28]. Bonnet et al. [28] demonstrated that after pathological examination 30 % of the tumors initially staged as T1N0 were considered for RAI ablation. Using univariate and multivariate analyses for PTCs ≤ 2 cm, Perrino et al. [29] demonstrated that performing CND prevents persisting/relapsing disease in pateints with a PTC measuring ≤2 cm. Ryu et al. [30] indicated that the lymph node ratio of the central compartment is a significant predictor (p < 0.001) according to a multivariate analysis of locoregional recurrence for patients who underwent total thyroidectomy with bilateral prophylactic CND.
There are two strategies for CND: unilateral and bilateral. Complication rates, especially for persistent hypoparathyroidism, increase in the order of no CND, unilateral CND, and bilateral CND [31–34]. The incidence of contralateral CND metastasis is not low [35, 36]. It was shown that ipsilateral lymph node metastasis significantly predicted contralateral node metastasis [37, 38]. Chae et al. [39] thus proposed routine ipsilateral CND with intraoperative reading of the frozen section to decide whether contralateral CND is also to be performed.
In 2012, the ATA investigated the design and feasibility of a prospective randomized controlled trial of prophylactic CND for PTC [40]. It concluded that this trial is not readily feasible in light of the number of patients needed and the cost. For the time being, therefore, we cannot expect any confirmative data about the utility of prophylactic CND for PTC [40]. Table 3 summarizes the merits and demerits of prophylactic CND.
Does dissection of the lateral compartment improve the prognosis of PTC patients? (CQ19)
In contrast to prophylactic CND, few studies have been published about whether dissection of the lateral compartment improves the prognosis of PTC patients. No guidelines, including the 2010 JSTS/JAES guidelines, actively recommend prophylactic lateral compartment dissection. However, there were some reports that recommended prophylactic lateral compartment dissection. In 2007, Ito et al. [41] demonstrated that the incidence of lateral node metastasis increased with tumor size. Also, in the subset of PTC patients who underwent prophylactic lateral node dissection, tumor size > 3 cm and significant extrathyroid extension were risk factors for lymph node recurrence. If these patients did not undergo lateral node dissection, their lymph node recurrence rates would be even poorer. In 2008, Sugitani et al. [42] conducted a multivariate analysis on patients who had no lateral node metastasis detectable by ultrasonography and who underwent CND only. These authors discovered that the presence of distant metastasis at diagnosis and tumor size ≥ 4 cm were independent prognostic factors of lymph node recurrence. Therefore, they recommended prophylactic lateral node dissection for such patients. In 2011, after the publication of our guidelines, Ito et al. [43] demonstrated that in the subset of patients with PTC who did not show ultrasonographically detectable lateral node metastasis and whose lesions measured 1.1–3.0 cm, N1a tumors were more likely to be associated with lymph node recurrence than N0 tumors, indicating that they may be candidates for prophylactic lateral node dissection. All of theses studies were retrospective. Nevertheless, patients with large or N1a tumors and with distant metastasis at diagnosis might be candidates for prophylactic lateral node dissection.
When is completion total thyroidectomy recommended as a second surgery for patients who underwent hemithyroidectomy and were classified as having follicular thyroid carcinoma? (CQ23)
In many Western institutions, completion total thyroidectomy is almost routinely performed in patients who underwent a hemithyroidectomy for the diagnosis of a follicular neoplasm or adenomatous nodule and were diagnosed as having follicular thyroid carcinoma (FTC). The 2010 JSTS/JAES guidelines recommend completion total thyroidectomy when the primary lesions are widely invasive FTC or have poorly differentiated components (especially insular carcinoma). However, no recommendation of completion total thyroidectomy is made for minimally invasive FTC.
Although the indications for completion total thyroidectomy for FTC still vary among the institutions in Japan, two relevant studies were recently published (Table 4) [44, 45]. Sugino et al. [44] demonstrated that patients aged <45 years showed an excellent prognosis, and completion total thyroidectomy might thus not be mandatory. The authors also showed that not only capsular but vascular invasion was unrelated to the prognosis of patients with minimally invasive FTC [44].
More recently, Ito et al. [45] showed that although the presence of vascular invasion did not affect the prognosis of their patients the recurrence rate for the patients with extensive vascular invasion (four or more lesions in total in all available H&E sections) was rather poor (20 % during a 10-year follow-up). They proposed that such patients may be candidates for completion total thyroidectomy. Both the Sugino et al. and Ito et al. studies indicated that tumor size (>4 cm) and patient age (≥45 years) are also significant prognostic factors, and they noted that physicians should decide how to treat patients with minimally invasive FTC in consideration of these factors.
One study investigated the timing of completion total thyroidectomy [46]. The results indicated that it should be performed either within 3 days of or >3 months after the primary surgery because persistent hypocalcemia was significantly decreased at these time points compared to other times. Because it takes some time to diagnose the degree of vascular invasion by pathology examination, it seems better to perform the second surgery ≥3 months after the initial surgery.
In 2002, Randolph and Daniels proposed that ablation of the remnant lobe be performed instead of completion thyroidectomy in patients who undergone previous limited thyroidectomy [47]. In 2012, Barbesino et al. [48] demonstrated that in FTC patients remnant thyroid lobe ablation with RAI resulted in outcomes similar to those of patients who underwent completion total thyroidectomy. This protocol eliminated the potential complications of a second surgery, such as hypoparathyroidism and recurrent laryngeal nerve paralysis or injury. In Japan, however, because legal restrictions regarding the use of RAI are still in place this strategy remains unrealistic.
What is the application and role of ablation? (CQ40)
Since publication of the 2010 JSTS/JAES guidelines, RAI ablation using 30 mCi (1.1 GBq) is permitted at outpatient clinics in Japan. Caglar et al. [49] showed that this dose is adequate at least for low-risk well-differentiated carcinoma [50]. The availability of rhTSH has also made ablation easier to perform in Japan, although it is costly. The issue of how to use 30 mCi RAI ablation in Japan needs to be addressed.
In Western countries, the indications for RAI ablation are broad, including tumor size > 1.5 cm, persistent disease, age ≥ 45 years, multifocality, and extrathyroid extension. Vascular invasion and lymph node metastasis are considered indications for RAI ablation [51], but these cases include many “non-high-risk” patients. In Japan, the legal restrictions and the lack of capacity make the use of RAI ablation for vascular invasion or lymph node metastasis not feasible.
Thus, a relatively new issue is whether RAI ablation is truly necessary for most patients. In a study of low-risk DTC patients, Schwartz et al. [52] reported that they failed to observe any survival benefit of RAI after surgery. Durante et al. [53] demonstrated that serum Tg values naturally dropped to undetectable levels within 5–7 years after thyroidectomy in low-risk patients. In a systematic analysis of the literature, Sacks et al. [54] concluded that postoperative RAI is not necessary.
Many endocrine surgeons in Japan have encountered patients with persistent disease (Tg detectable after total thyroidectomy), but most of these patients survived without RAI administration if their Tg levels were stable. Traditionally in Japan, RAI ablation has not been actively performed, but we do know that most DTC patients in Japan display an excellent prognosis. For example, at Kuma Hospital, the mortality rate of M0 PTC patients was slightly over 1 %, although most of these patients did not undergo RAI ablation (our unpublished data).
Iyer et al. [55] investigated the Surveillance and Epidemiology and End Results (SEER) database (http://seer.cancer.gov/) and demonstrated the rising incidence of second cancers among low-risk thyroid cancer patients who underwent RAI therapy. Hay et al. [56] showed that in patients who underwent RAI administration after surgery for PTC during childhood, 68 % of the patients who died thereafter died from nonthyroid malignancies. Taken together, these findings suggest that the indications for RAI ablation could be narrowed down: that is, to only high-risk patients, such as those with severe extrathyroid extension, a large lesion and many lymph node metastases, and aggressive histology.
Higher and therapeutic doses of RAI are preferable when a patient is classified as at high risk and when a poor CSS is predicted. For M1 patients, immediate administration of a therapeutic dose of RAI is mandatory. Miyauchi et al. [17] demonstrated that short (<2 years) Tg doubling times strongly predicted the carcinoma death of Tg antibody-negative PTC patients who underwent total thyroidectomy, regardless of preoperative and intraoperative clinicopathologic features. Thus, administration of a high dose of RAI when a patient’s Tg starts rising during the follow-up is an alternative.
Discussion
In this review, we revisited the 2010 JSTS/JAES guidelines. In doing so, we found that most of the DTC treatment strategies described in the guidelines are reasonable, although some revisions based on new findings are necessary. In addition, the appearance of novel agents should be added to the guidelines. Extensive revisions might even be mandatory in such cases.
During the past few years, the strategies used in Western countries and those used in Japan for treating DTC have become more similar. The complete body of data suggests that immediate surgery for incidentally detected PMC is overtreatment. Endocrinologists and endocrine surgeons in Western countries are thus facing or will encounter a dilemma as numerous microcarcinomas are incidentally detected with the increasing use of ultrasonography and ultrasonography-guided aspiration biopsy. The excellent prognosis for low-risk patients who underwent limited thyroidectomy raises issues concerning whether routine total thyroidectomy is truly beneficial for patients.
There is a U.S. report that patients with pT1/T2N0, well-DTCs were safely managed by thyroid lobectomy only [57]. Similarly, as indicated above, recent reports from Western countries display negative data for routine RAI ablation for low-risk patients. Unfortunately, the ATA concluded that a prospective randomized study for prophylactic CND is not feasible. Thus, we cannot expect any informative data about prophylactic CND in a large series of patients for the time being. At present, its indication may depend on institutional policy and surgeons’ skill levels.
The production of molecularly targeted agents and their applications for thyroid carcinoma have recently been initiated. For example, the effectiveness of vandetanib for medullary thyroid carcinoma was demonstrated in a Phase III study [58]. Thus, the U.S. Food and Drug Administration approved the use of vandetanib for this purpose. Vandetanib will be available in Japan in the near future. A Phase III study of vandetanib for DTC is in progress on a worldwide scale.
The effectiveness of sorafenib for advanced or metastatic (and progressive) RAI-refractory DTC was reported at the 2013 American Society for Clinical Oncology meeting [59]. At present, many other molecularly targeted agents are in Phase I–III trials, and new agents can also be expected. We do not know whether the use of these agents will bring about major changes in the therapeutic strategies for DTC, but their positive and negative data will be considered in future revisions of the JSTS/JAES guidelines.
Conclusions
Taken together, the strategies for treating DTC in Western countries and Japan are moving toward a consensus. The issue of how to treat DTC itself may change because of the prevalence of molecularly target agents. The JSTS/JAES guidelines will be revised again within a few years, and the corresponding guidelines in other countries may also be updated in the near future. However, the policies and ultimate goal is not change. That is, the starting point of the guidelines is identifying the best treatment for patients with thyroid carcinoma worldwide.
References
Takami H, Ito Y, Noguchi H et al (eds) (2013) Treatment of thyroid tumor. Springer, New York
Takami H, Ito Y, Okamoto T et al (2011) Therapeutic strategy for differentiated thyroid carcinoma in Japan based on a newly established guideline managed by Japanese Society of Thyroid Surgeons and Japanese Association of Endocrine Surgeons. World J Surg 35:111–121
Sugitani I, Toda K, Yamada K et al (2010) Three distinctly different kinds of papillary thyroid microcarcinoma should be recognized: our treatment strategies and outcomes. World J Surg 34:1222–1231
Ito Y, Miyauchi A, Inoue H et al (2010) An observation trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 34:28–35
Sugitani I, Fujimoto Y, Yamada K (2013) Association between serum thyrotropin concentration and growth of asymptomatic papillary thyroid microcarcinoma. World J Surg Nov 14. [Epub ahead of print]
Ito Y, Miyauchi A, Kihara M et al (2013) Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid 24:27–34
Ito Y, Kudo T, Kobayashi K et al (2012) Prognostic factors for recurrence of papillary thyroid carcinoma in the lymph node, lung, and bone: analysis of 5,768 patients with average 10-year follow-up. World J Surg 36:1274–1278
Takebe K, Date M, Yamamoto Y et al (1994) Mass screening for thyroid cancer with ultrasonography. KARKINOS 7:309–317 (in Japanese)
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Anonymous (2007) Guidelines for the management of thyroid cancer second edition. http://www.british-thyroid-association.org/news/Docs/Thyroid_cancer_guidelines_2007.pdf
Thyroid Carcinoma Task Force (2001) AACE/AAES medical/surgical guidelines for clinical practice management of thyroid carcinoma. Endocr Pract 7:202–220
National Comprehensive Cancer Network (2013) NCCN clinical practice guidelines in Oncology. Thyroid Carcinoma. Version 2
Dralle H, Musholt TJ, Schabram J et al (2013) German Association of Endocrine Surgeons practice guideline for the surgical management of malignant thyroid tumors. Langenbecks Arch Surg 398:347–375
Ito Y, Masuoka H, Fukushima M et al (2010) Excellent prognosis of patients with solitary T1N0M0 papillary thyroid carcinoma who underwent thyroidectomy and elective lymph node dissection without radioiodine therapy. World J Surg 34:1285–1290
Ito Y, Fukushima M, Kihara M et al (2012) Investigation of the prognosis of patient age with papillary thyroid carcinoma by size. Endocr J 59:457–464
Matsuzu K, Sugino K, Kasthikot M et al (2014) Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1088 patients. World J Surg 38:68–79
Miyauchi A, Kudo T, Miya A et al (2011) Prognostic impact of serum thyroglobulin doubling-time under thyrotropin suppression in patients with papillary thyroid carcinoma who underwent total thyroidectomy. Thyroid 21:707–716
Ito Y, Miyauchi A (2009) Prognostic factors and therapeutic strategies for differentiated carcinoma of the thyroid. Endocr J 58:177–192
Ito Y, Fukushima M, Higashiyama T et al (2013) Tumor size is the strongest predictor of microscopic lymph node metastasis and lymph node recurrence of N0 papillary thyroid carcinoma. Endocr J 60:113–117
Conzo G, Docirro G, Ruggiero R et al (2012) Surgical treatment of papillary thyroid carcinoma without lymph nodal involvement. G Chir 33:339–342
Monchik JM, Simon CJ, Caragacianu DL et al (2009) Does failure to perform prophylactic level VI node dissection leave persistent disease detectable by ultrasonography in patients with low-risk papillary carcinoma of the thyroid? Surgery 146:1182–1187
Yoo D, Ajmal S, Gowda S et al (2012) Level VI lymph node dissection does not decrease radioiodine uptake in patients undergoing radioiodine ablation for differentiated thyroid cancer. World J Surg 36:1255–1261
Lang BH, Wong KP, Wan KY et al (2012) Impact of routine unilateral central neck dissection on preablative and postablative stimulated thyroglobulin levels after total thyroidectomy in papillary thyroid carcinoma. Ann Surg Oncol 19:60–67
Moreno MA, Edeiken-Monroe BS, Siegel ER et al (2012) In papillary thyroid cancer, preoperative central neck ultrasound detects only macroscopic surgical disease, but negative findings predict excellent long-term regional control and survival. Thyroid 22:347–355
Hartl DM, Leboulleux S, Al Ghuzlan A et al (2012) Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg 255:777–783
Laird AM, Gauger PG, Miller BS et al (2012) Evaluation of postoperative radioactive iodine scans in patients who underwent prophylactic central lymph node dissection. World J Surg 36:1268–1275
Moo TA, McGill J, Allendorf J et al (2010) Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg 34:1187–1191
Bonnet S, Hartl D, Leboulleux S et al (2009) Prophylactic lymph node dissection for papillary thyroid cancer less than 2 cm: implications for radioiodine treatment. J Clin Endocrinol Metab 94:1162–1167
Perrino M, Vannucchi G, Vicentini L et al (2009) Outcome predictors and impact of central node dissection and radiometabolic treatments in papillary thyroid cancers ≤2 cm. Endocr Relat Cancer 16:201–210
Ryu IS, Song C, Choi SH et al (2013) Lymph node ratio of the central compartment is a significant predictor for locoregional recurrence after prophylactic central neck dissection in patients with thyroid papillary carcinoma. Ann Surg Oncol 21:277–283
Kwan WY, Chow TL, Choi CY et al (2013) Complication rates of central compartment dissection in papillary thyroid cancer. ANZ J Surg Jul 26. [Epub ahead of print]
Giordano D, Valcavi R, Thompson GB et al (2012) Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid 22:911–917
Khatib ZE, Lamblin J, Augert S et al (2010) Is thymectomy worthwhile in central lymph node dissection for differentiated thyroid cancer? World J Surg 34:1181–1186
Raffaelli M, De Crea C, Sessa L et al (2012) Prospective evaluation of total thyroidectomy versus ipsilateral versus bilateral central neck dissection in patients with clinically node-negative papillary thyroid carcinoma. Surgery 152:957–964
Ito Y, Jikuzono T, Higashiyama T et al (2006) Clinical significance of lymph node metastasis of thyroid papillary carcinoma located in one lobe. World J Surg 30:1821–1826
Sadowski BM, Snyder SK, Laimore TC (2009) Routine bilateral central lymph node clearance for papillary thyroid cancer. Surgery 146:696–703
Lee KE, Chung IY, Kagn E et al (2013) Ipsilateral and contralateral central lymph node metastasis in papillary thyroid cancer: patterns and predictive factors of nodal metastasis. Head Neck 35:672–676
Kim WW, Park HY, Jung JH (2013) Surgical extent of central lymph node dissection in clinically node-negative papillary thyroid cancer. Head Neck Jan 16 [Epub ahead of print]
Chae BJ, Jung CK, Lim DJ et al (2011) Performing contralateral central lymph node dissection in papillary thyroid carcinoma: a decision approach. Thyroid 21:873–877
Carling T, Carty SE, Clarlegio MM et al (2012) American Thyroid Association design and feasibility of a prospective randomized controlled trial of prophylactic central lymph node dissection for papillary thyroid carcinoma. Thyroid 22:237–244
Ito Y, Higashiyama T, Takamura Y et al (2007) Risk factors for recurrence to the lymph node in papillary thyroid carcinoma patients without preoperatively detectable lateral node metastasis: validity of prophylactic modified radical neck dissection. World J Surg 31:2085–2091
Sugitani I, Fujimoto Y, Yamada K et al (2008) Prospective outcomes of selective lymph node dissection for papillary thyroid carcinoma based on preoperative ultrasonography. World J Surg 32:2494–2502
Ito Y, Tsushima Y, Masuoka H et al (2011) Significance of prophylactic modified radical neck dissection for patients with low-risk papillary thyroid carcinoma measuring 1.1–3.0 cm: first report of a trial at Kuma Hospital. Surg Today 41:1486–1491
Sugino K, Kameyama K, Ito K et al (2012) Outcomes and prognostic factors of 251 patients with minimally invasive follicular thyroid carcinoma. Thyroid 22:798–804
Ito Y, Hirokawa M, Masuoka H et al (2013) Prognostic factors of minimally invasive follicular thyroid carcinoma: extensive vascular invasion significantly affects patient prognosis. Endocr J 60:637–642
Glockzin G, Hronung M, Klaus K et al (2013) Completion thyroidectomy: effect of timing on clinical complications and oncologic outcome in patients with differentiated thyroid cancer. World J Surg 36:1168–1173
Randolph GW, Daniels GH (2002) Radioactive iodine lobe ablation as an alternative to completion thyroidectomy for follicular carcinoma of the thyroid. Thyroid 12:989–996
Barbesino G, Goldfarb M, Parangi S et al (2012) Thyroid lobe ablation with radioactive iodine as an alternative to completion thyroidectomy after hemithyoridectomy in patients with follicular thyroid carcinoma: long-term follow-up. Thyroid 22:369–376
Caglar M, Bozkurt FM, Akca CK et al (2012) Complication of 800 and 3700 MBQ iodine-131 for the postoperative ablation of thyroid remnant in patients with low-risk differentiated thyroid cancer. Nucl Med Commun 33:268–274
Schlumberger M, Catargi B, Borget I et al (2012) Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med 366:1663–1673
Robbins RJ, Schlumberger MJ (2005) The evolving role of 131I for the treatment of differentiated thyroid carcinoma. J Nucl Med 46(Suppl 1):28S–37S
Schwartz C, Bonnetain F, Dabakuyo S et al (2012) Impact on overall survival of radioactive iodine in low-risk differentiated thyroid cancer patients. J Clin Endocrinol Metab 97:1526–1535
Durante C, Montesano T, Attard M et al (2012) Long-term surveillance of papillary thyroid cancer patients who do not undergo postoperative radioiodine remnant ablation: is there a role for serum thyroglobulin measurement? J Clin Endocrinol Metab 57:2748–2753
Sacks W, Fung CH, Chang JT et al (2010) The effectiveness of radioactive iodine for treatment of low-risk thyroid cancer: a systematic analysis of the peer-reviewed literature from 1966 to April 2008. Thyroid 20:1235–1245
Iyer NG, Morris LGT, Tuttle RM et al (2011) Rising incidence of second cancers in patients with low-risk (T1N0) thyroid cancer who receive radioactive iodine therapy. Cancer 117:4439–4446
Hay ID, Gonzalez-Losada T, Reinalda MS et al (2010) Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg 34:1192–1202
Nixon IJ, Banly I, Patel SG et al (2012) Thyroid lobectomy for treatment of well differentiated intrathyroid malignancy. Surgery 151:571–579
Wells SA, Robinson BG, Gagel RF et al (2012) Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol 30:134–141
Brose MS, Nutting C, Jarzab B et al (2013) Sorafenib in locally advanced or metastatic patients with radioactive iodine-refractory differentiated thyroid cancer: the phase III DECISION trial. Presented at the 49th annual meeting of the American Society of Clinical Oncology (ASCO) plenary session. Abstract #4
Acknowledgments
There is no grant support to report.
Conflict of interest
There are no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takami, H., Ito, Y., Okamoto, T. et al. Revisiting the Guidelines Issued by the Japanese Society of Thyroid Surgeons and Japan Association of Endocrine Surgeons: A Gradual Move Towards Consensus Between Japanese and Western Practice in the Management of Thyroid Carcinoma. World J Surg 38, 2002–2010 (2014). https://doi.org/10.1007/s00268-014-2498-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2498-y