Abstract
Background
Systematic studies of intermittent intraoperative neuromonitoring (IONM) have shown that IONM enhances recurrent laryngeal nerve (RLN) identification via functional assessment, but does not significantly reduce rates of vocal cord (VC) paralysis (VCP). The reliability of functional nerve assessment depends on the preoperative integrity of VC mobility. The present study was therefore performed to analyze the validity of IONM in patients with pre-existing VC paralysis.
Methods
Of 8,128 patients, 285 (3.5 %) with preoperative VCP underwent thyroid surgery using standardized IONM of the RLN and vagus nerves (VNs). VC function was assessed by pre- and postoperative direct videolaryngoscopy. Quantitative parameters of IONM in patients with VCP were compared with IONM in patients with intact VC function. Clinical symptoms and surgical outcomes of patients with pre-existing VCP were analyzed.
Results
A total of 244 patients revealed negative, and 41 revealed positive IONM on the side of the VCP. VCP with positive IONM revealed significantly lower amplitudes of VN and RLN than intact VN (p = 0.010) and RLN (p = 0.011). Symptoms of patients with VCP included hoarseness (25 %), dyspnea (29 %), stridor (13 %), and dysphagia (13 %); 13 % were asymptomatic. New VCP occurred in five patients, ten needed tracheostomy for various reasons, and one patient died.
Conclusions
Patients with pre-existing VCP revealed significantly reduced amplitude of ipsilateral VN and RLN, indicating retained nerve conductivity despite VC immobility. Preoperative laryngoscopy is therefore indispensable for reliable IONM and risk assessment, even in patients without voice abnormalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Today, intermittent intraoperative neuromonitoring (IONM) in thyroid and parathyroid surgery is broadly utilized, and distinctive standards have been established. IONM enhances identification of the recurrent laryngeal nerve (RLN) by functional findings of an electromyograph (EMG) that can only be generated by nerves; however, a significant reduction in the rate of postoperative vocal cord (VC) paralysis (VCP) by IONM in primary and benign goiter surgery was not demonstrated [1, 2]. Regardless, numerous authors have emphasized the virtues of IONM in challenging surgery, e.g. recurrent goiter, Graves’ disease, retrosternal and mediastinal thyroid extension, thyroid malignancy, and malignant recurrence [1–13]. Most of all, IONM is valued for preventing the most hazardous complication of thyroid surgery, bilateral VCP. IONM enables a change of surgical strategy in bilateral thyroid surgery, when nerve dysfunction is detected intraoperatively [2, 7, 9, 12]. In case of loss of signal (LOS), defined as irreproducible EMG curve and acoustic signal or reduction of amplitude to <100 μV, on the first and dominant side of resection, a planned bilateral procedure may be stopped in favor of staged thyroidectomy [13–15]. Disregarding nerve transection injury, LOS is the most reliable indicator of postoperative VCP in macroscopically impaired as well as anatomically preserved nerve integrity. In a previous study, normal quantitative IONM parameters reflecting routine everyday conditions of anesthesia and surgery were established, and it was concluded that relevant changes of those IONM parameters might be indicative of imminent danger to the RLN, prior to LOS. Corresponding surgical actions thought to be responsible included, for example, stretching and pressure as indirect causes for reduction in amplitude, increase of latency, and sometimes deconfiguration of EMG waveform [16]. However, recognition of these alterations in intermittent IONM is limited by the successive nature of preparation and stimulation, and the demanding attentiveness of the operating surgeon to EMG alterations in lack of thresholds and warning signs. Currently, the extent to which the recent development of continuous IONM (CIONM) overcomes these limitations remains to be determined and is an aspect that is presently under investigation [13, 17, 18].
The incidence of bilateral VCP in thyroid surgery with or without use of IONM is rarely reported, and considerable under-reporting must be assumed [19–21]. Given the ongoing controversies regarding the value, standard application, costs, effort, and time involved with IONM, as well as the interpretation and impact of IONM parameters, the main virtue of IONM in prevention of bilateral VCP remains outstanding [22–24]. In this context, confirmation of positive IONM in ipsilateral VCP raises questions regarding the relationship between IONM and VC function. Ultimately, positive IONM in pre-existing VCP may defy efforts and costs involved, and fundamentally challenge the validity of IONM. This study aimed to first analyze specifically positive IONM in established VCP in order to assess the reliability and consequences of IONM application. Second, it aimed to analyze surgical outcome and investigate the impact of IONM on cervical surgery in established VCP, thus highlighting the superior challenge of contralateral surgery in permanent unilateral VCP.
Materials and methods
Patients
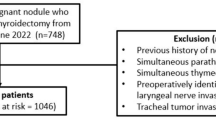
Patients with pre-existing, laryngoscopically verified VCP undergoing cervical surgery intended for benign and malignant thyroid disease were identified from a prospective database, and the data were retrospectively analyzed. All of these patients revealed completely immobilized VCs. None of these VCs appeared grossly altered; specifically, there was no VC fibrosis, VC fixation, or arytenoid luxation present in any of the patients included in the study. From June 1998 until May 2013, a total of 285 of 8,128 patients undergoing cervical surgery for thyroid disease using IONM revealed pre-existing inferior RLN paralysis, and 7,843 showed bilateral normal function of VCs. Positive intact IONM was defined according to established definitions with regular EMG, positive latency, and minimum amplitude of >100 μV [2]. IONM identified 41 positive EMGs in ipsilateral VCP, and 244 cases of VCP exhibited negative IONM (Fig. 1).
Methods
Intermittent IONM was initially applied using directly placed needle electrodes with the Neurosign 100® system (inomed GmbH, Emmendingen, Germany). In this series, this was applied in ten patients in the IONM-negative group. The IONM method was then changed to tube electrodes and was applied in all remaining patients, specifically in all 41 patients with positive IONM in pre-existing VCP. Tube electrode IONM was carried out with the Medtronic NIM1® and NIM2® systems for intermittent, and, most recently, the CIONM NIM3® system (Medtronic Co., Jacksonville, FL, USA). All patients underwent pre- and postoperative (V1 and V2) direct videolaryngoscopy for assessment of VC mobility. IONM was applied in a standard procedure; the detailed technique, materials, and procedural application have been previously described [13, 16]. Surgery started on the dominant side according to malignancy and/or size criteria. Following identification and stimulation of the ipsilateral vagus nerve (VN) (V1), the ipsilateral inferior RLN was identified and stimulated (R1). Accordingly, after completion of resection, stimulation of RLN (R2) and VN (V2) commenced, and all EMG data were printed and saved. Direct videolaryngoscopy (V2) for confirmation of VC mobility was usually performed on postoperative day 2, rarely later.
Specific EMG parameters of IONM, namely amplitude, latency, signal width of positive IONM, and the absence of reproducible EMG in VCP, were analyzed and compared with those of patients with intact functional VCs. With the aim of describing the electrophysiologic characteristics of VCP, IONM of pre-resection parameters was described for this series. The time point of pre-resection was defined as previously described in the definition of normal IONM parameters as follows: preparing the surgical field until straight forward, first exposing the VNs, and then the RLNs for application of IONM; however, preceding any resective maneuver to the thyroid and/or lymph nodes. The physiologically significant differences in latency of left versus right VNs were corrected by the additional term of 1.99 for all calculations of latency. Positive EMG in established VCP was compared in individual patients with IONM parameters of the contralateral intact VC side in order to exclude tube placement-related biased differences, and was also compared with established normal parameters according to the previous study, for overall analysis. Analysis of demographic data, clinical symptoms, laryngoscopy findings, surgical procedures performed, and surgical outcomes of all patients aimed to identify differences in patients with positive and negative IONM in pre-existing VCP.
Statistical analysis
The statistical analysis was performed using SPSS Statistics for Windows, version 20.0 (SPSS Inc., Chicago, IL, USA). Results are expressed by mean ± standard deviation (SD) or median (range) as appropriate. Data analysis for proportions, parametric, and non-parametric parameters was performed using the Wilcoxon-rank test and the Mann–Whitney U test. Statistical significance was considered to be p < 0.05.
Results
Demographics and clinical characteristics
Gender distribution of the 285 patients with pre-existing VCP was as follows: 191 female (67 %) and 94 (33 %) male. VCP was evenly distributed, with 135 (47 %) on the right side and 130 (46 %) on the left side. A total of 13 (4.6 %) patients had combined unilateral VCP and contralateral incomplete VCP (defined as impaired but residual VC mobility) (right VCP+left incomplete VCP N = 5; left VCP+right incomplete VCP N = 8), and seven (2.5 %) patients exhibited bilateral VCP. One (0.35 %) patient had a right non-recurrent inferior laryngeal nerve (NRLN) with postoperative magnetic resonance imaging (MRI) validation of associated lusorian artery in the IONM-negative group and no NRLN in the IONM-positive group [25].
The mean age was 58 (±16) years. A total of 66 (23 %) patients were scheduled for primary surgery versus 219 (77 %) patients for redo cervical surgery. Indication for surgery was benign thyroid disease in 117 (41 %) and malignancy in 168 (59 %). Surgical procedures involved thyroid resection in 226 (79 %) and/or central compartment lymph node dissection (C1) (paratracheal groove) in 159 (56 %) [26] (Table 1).
In all, 36 (13 %) patients presented with clinically asymptomatic VCP preoperatively. Five of these asymptomatic patients underwent primary cervical surgery. Of the 36 asymptomatic patients, 12 showed positive IONM ipsilateral to the VCP side, three of whom had not undergone any previous cervical or thoracic surgery. Conversely, clinical symptoms in established VCP comprised hoarseness in 72 (25 %), stridor in 26 (9 %), dyspnea in 83 (29 %), progressive cervical compression in 74 (26 %), and dysphagia in 36 (13 %) (Table 1).
In 244 patients with VCP, IONM could not produce positive EMG of the RLN and/or VNs.
Clinical characteristics in IONM-positive patients
Specific sub-analysis of the 41 IONM-positive patients showed 34 (83 %) female and seven (17 %) male patients, with a mean age of 60 (±15.3) years. Primary surgery was planned in eight (19 %) versus redo procedures in 33 (81 %). Indication for surgery was benign thyroid disease in 28 (68 %) and malignancy in 13 (32 %). Clinically asymptomatic VCP was seen in 12 (29 %), whereas 17 (42 %) demonstrated dyspnea, eight (20 %) stridor, 19 hoarseness (46 %), six cervical compression (15 %), and six (15 %) dysphagia. Mean duration of VCP was 109 (±150) months in IONM-positive patients, and could not reliably be determined in the IONM-negative patients (Table 1).
Surgical procedures
Surgical procedures in this series of patients with preoperatively diagnosed VCP involved primary and redo thyroid resections in benign disease (N = 117; 41 %), and primary and redo surgery in malignant disease (N = 168; 58.9 %) (Table 2). The maximum risk profile in regard to VC function is held by surgery contralateral to the pre-existing VCP, and was undertaken altogether in 215 patients with a spectrum of procedures performed (Table 2). Extent of thyroid resection to the ipsilateral side of pre-existing VCP (surgical low-risk category) comprised enucleation in 52 (18 %) patients, subtotal thyroid resection in four (1 %), central compartment lymph node dissection in 166 (58 %), and lobectomy in 150 (53 %). Maximum risk category surgery of contralateral (±ipsilateral) resection in pre-existing VCP in regard to the contralateral side comprised enucleation in 27 (9 %), subtotal thyroid resection in six (2 %), central compartment lymph node dissection in 130 (46 %), and lobectomy in 146 (51 %) patients (Table 2). Overall, 34 RLNs (ten right, 24 left) were resected as mandatory by oncological principle, all within the IONM-negative group.
In addition to the 34 nerves that were resected, intraoperative LOS (defined in contemporary literature as complete loss of EMG, signal sound, and/or decrease of amplitude to <100 μV) of a functional RLN and/or VN occurred in five patients in the IONM-negative group and in one patient in the IONM-positive VCP group. Despite new LOS with expectant effective bilateral VCP, intraoperative laterofixation of a VC on the side of the pre-existing VCP was not performed in this series of patients. Intraoperative tracheostomy was conducted in five patients. In three patients, protective tracheostomy was performed: for intraoperative LOS in one, and for protection of precarious reconstructive procedures involving trachea and/or esophagus with muscle flaps in two patients. Another two patients required laryngectomy, and intraoperative tracheostomy was consequently implemented.
IONM parameters in VCP
Of 285 patients with VCP, 41 (14.3 %) demonstrated positive IONM. Analysis of pre-resection quantitative IONM parameters of amplitude, latency, and signal width were intra-individually compared with the functionally intact contralateral sides, thereby diminishing the influence of inter-individual differences due to the quality of tube positioning. Additionally, these quantitative parameters were compared with established normal pre-resection parameters of IONM in functionally intact VNs and RLNs after correction for physiologic differences between left and right side by the term 1.99 [16].
Amplitude
Intra-individual pre-resection IONM of ipsilateral VCP demonstrated significantly lower median amplitude of VNs (295 μV) compared with the intact sides (513 μV) (p = 0.010), as was true for significantly lower amplitudes of inferior RLNs in VCP (372 μV) compared with intact VC (459 μV) (p = 0.011) (Table 3).
In comparison with established normal parameters for VNs (479 μV), VCP again showed significantly lower amplitudes (295 μV) (p < 0.001). Similarly, RLNs in VCP had significantly lower amplitudes (371 μV) than normal functioning RLNs (665 μV) (p < 0.001).
Latency
Pre-resection median latency of VNs was significantly greater in VCP (5.95 ms) than in intact VC (4.69 ms) (p = 0.014). Similarly, this was true for RLNs in VCP (2.34 ms) versus normal RLNs (2.25 ms) (p = 0.046) (Table 3).
Conversely, comparison of median latency of VNs in VCP (5.95 ms) to normal parameters (5.90 ms) did not reach statistical significance (p = 0.775). Surprisingly, the median latency of RLNs in VCP (2.34 ms) was significantly shorter than established normal parameters for intact RLNs (2.73 ms) (p = 0.016).
Signal width
Regarding pre-resection median signal width of VNs, no significant difference between VCP (9.77 ms) and normal functioning sides (8.22 ms) was demonstrated (p = 0.094). Likewise, RLN in VCP revealed no significant difference of signal width (8.59 ms) versus intact RLNs (8.36 ms) (p = 0.931) (Table 3).
Comparison of median signal width in VNs in VCP (9.76 ms) with normal parameters (8.98 ms) again revealed no significant difference (p = 0.139), whereas median signal width of RLNs in VCP (8.59 ms) was significantly broader versus signal width in normal functioning RLNs (7.42) (p = 0.001).
Surgical outcome
With respect to the main focus of VC function in these patients, postoperative VC mobility was routinely assessed by direct videolaryngoscopy on postoperative day 2, later in exceptional cases and as determined appropriate. Of the 285 patients with pre-existing VCP, five patients operated on in this series experienced LOS with new and permanent VCP. Consequently, there resulted 12 bilateral VCP in total, since seven patients already had bilateral VC paresis before the current operation, i.e., pre-existing unilateral and/or contralateral incomplete VC paresis (Table 4).
In cases of symptomatic postoperative VCP, conservative treatment with inhalation therapy, anti-edematous, and anti-inflammatory drugs were administered in all patients. Postoperative re-intubation was mandatory in three (1.05 %) patients. Unsatisfactory conservative measures yielded postoperative laterofixation of one VC on the side of the pre-existing VCP in four (1.4 %) patients, one sequenced by tracheostomy. Postoperative tracheostomy was conducted in five (1.75 %) patients and based on progressive respiratory insufficiency in all. Of these, two presented with unchanged pre-existing bilateral VCP, one with unchanged pre-existing unilateral VCP and two with insufficiency of reconstructive muscle flaps (Table 5).
General surgical complications included the need for reoperation due to bleeding in seven, due to wound infection in two, and for persistent lymph fistula, seroma, and secondary wound closure in 11. Secondary partial wound closure was performed in six cases for superficial wound dehiscence and in five after correction of deep wound infection or lymph fistula. The unusually high rate of postoperative hematoma was associated with prolonged and extensive repetitive redo cancer surgery cases in four, and necessary persistent anticoagulative medication in three patients. Wound infection developed in six, sternal infection in one, and seroma in 16 patients. One patient experienced secondary wound dehiscence. Pulmonary complications were evident in six, and cardiac complication occurred in one patient. Other complications totaled nine and comprised pulmonary artery embolism, transient fever, nausea and vomiting, and salivary gland inflammation (Table 4). These high rates of complications in regard to bleeding and wound problems is at least partly explained by the highly complex and lengthy cancer redo surgeries as well as comorbidity of patients included in this group. Hypoparathyroidism was defined by prevalent substitution of calcium and/or vitamin D for hypocalcemia. The preoperative rate was 4.5 %, and increased to a transient postoperative rate of 9.4 %. However, scarce follow-up data on the substitution regimen did not allow for assessment of the permanent hypoparathyroidism rate in this series.
Discussion
This study describes the largest cohort of patients undergoing thyroid surgery with IONM in the setting of pre-existing VCP, describing comprehensive characteristics with a special focus on assessment of IONM parameters and surgical outcome. Due to the scarcity of comparable data in the literature, discussion of the findings of the present study can only focus on a few representative other investigations.
Limitations of the study
Because the etiology of pre-existent VCP in primary benign surgery, as well as the nature of nerve injury in previous outward surgery remains unresolved, this series for a large part suffices with descriptive data and refrains from conclusions beyond this. Some certain factors may contribute to the phenomenon of positive IONM in established VCP, but cannot be proved, as follows. (i) During VN stimulation, an intact superior laryngeal nerve that is not routinely assessed in standard IONM application, ipsilateral to a damaged RLN, may trigger electrical responses picked up by the IONM [27]. In cases of pre-laryngeal ramification and damage to the anterior branch of RLN that usually carries the motor fibers, the intact inferior branch for the posticus muscle may preserve positive IONM of VN and recurrent (branch) stimulation even though the VCP is paralyzed [28]. (ii) Long-term restoration of electrical conductivity in a partially damaged nerve may result in positive IONM, yet degenerative changes of the VC and/or laryngeal muscles that are not accessible in direct laryngoscopy prevent VC mobility.
Due to the retrospective analysis, precise description of all identified RLN and VN in IONM-negative VCP was not available, and missing data necessitated median value correlation. Moreover, comprehensive longitudinal follow-up was not performed to enable a more thorough long-term prognostication of VC function and surgical outcome.
IONM, preoperative laryngoscopy, and quantitative parameters
The usefulness of IONM in reducing the RLN paralysis rate in thyroid surgery is debated throughout the literature, whereas the superior rate of objectivizing RLN identification by functional assessment and benefit in recurrent surgery is mostly not [3, 23, 29, 30]. In contrast, even authors who challenge the benefit of IONM in standard thyroid surgery acknowledge the usefulness and impact of IONM in facilitating prevention of bilateral VCP in bilateral surgery and benefits in ‘complicated’ thyroid surgery. Nevertheless, data to support this advantage of IONM in specifically challenging and high-risk surgery are limited [23, 24]. In this regard, the validity of IONM is especially challenged in reliably predicting postoperative VC function in high-risk thyroid surgery. Negative and positive predictive values of IONM for postoperative VC function are reported at 85–90 and 37–40 %, respectively [4, 7, 14, 23, 28, 30, 31]. Negative predictive value in regard to IONM represent negative test results, reflecting the rate of postoperative recurrent nerve palsy despite intact IONM signals. Conversely, positive predictive values in regard to IONM represent positive test results, reflecting the rate of intact VC function despite LOS in IONM. For the study group investigated, accuracy as well as inaccuracy cannot be calculated because, in established VCP, postoperative VCP was always present as diagnosed preoperatively. This background elucidates critical evaluation of positive IONM in pre-existing VCP resembling IONM in normal functioning nerves. Notably, in this study, the pre-resection amplitudes of RLN (median 372 μV; quartiles 179; 596) with preoperative palsy exhibit values decidedly above the level of the definition of LOS used in the literature of 100 μV, although amplitude ranges clearly lower than those of the intact RLN (median 459; quartiles 237; 1,069). Thereby, IONM in pre-existing VCP appears unreliable and can only be interpreted in the context of preoperative laryngoscopic functional findings of the VC. In this context, the established definition of LOS does not apply to pre-existing VCP and positive IONM. Does this phenomenon now make IONM a high-effort and futile tool? Positive IONM in this series highlights the important pre-conditions for interpretation and ingenious application of IONM. First, preoperative laryngoscopy is warranted. However, the necessity of preoperative laryngoscopy in primary surgery is controversial and some opponents even assume normal voice to be a sufficient indicator of normal VC function [32, 33]. However, empirically, VCP may develop insidiously and even present as clinically asymptomatic, as seen in 13 % of patients in this series. Therefore, preoperative investigation of VC mobility is the mainstay finding to enable reliable interpretation of IONM, regardless of primary or redo cervical surgery. Moreover, infrequent use of preoperative laryngoscopy may well under-report the prevalence of primary VCP in patients undergoing thyroid surgery.
Goretzki et al. [24] first described a subgroup of patients (2/8 ≈ 25 %) with positive IONM in pre-existing VCP; however, no specific IONM parameters were provided. On the other hand, the current study is the first to describe a hitherto unheralded large series of 41 patients with VCP and positive IONM, closely resembling normal IONM. Specific analysis of quantitative parameters for the first time revealed significantly reduced amplitudes of recurrent laryngeal and VNs in pre-existing VCP with anatomically intact RLN and VN compared with the contralateral intact VC [16]. Moreover, comparison of median latency of the VN and RLN of the ipsilateral VCP compared with the functionally intact VC side in each patient revealed significantly greater latencies (Table 3). Second, interpretation of IONM must be based on quantitative parameters in order to benefit from the method beyond the ‘all or nothing’ event of LOS. These findings underline the importance of recognizing intraoperative changes in amplitude as an early indicator for dangerous maneuvers for the RLN with impeding risk of postoperative functional impairment. In cases of synchronous increase of latency, these combined events indicate imminent danger to nerve function as affirmed by preliminary data of CIONM by Schneider et al. [13]. Conversely, the latency and signal width of the VNs and RLNs failed to indicate significant differences from normal IONM parameters in patients with intact VC mobility. Therefore, both appear to be of lesser importance in representation of VC function at the time of investigation. Nevertheless, all IONM parameters represent functional nerve integrity and, according to the data from this study, a descending hierarchy of amplitude > latency > signal width in prediction of VCP mobility is implied.
Consequently, IONM and preoperative laryngoscopy represent a unit in which one remains unreliable without the other. Recognition of quantitative IONM parameters, namely amplitude and comparison with normal parameters, are important in order to assess neural preconditions at the start of surgery, and moreover to adapt surgical measures precluding LOS. Pre-existing as well as impending nerve pathologies may therefore be detected with IONM.
IONM, ‘high-risk’ thyroid surgery, and complications
Correlations between an increasing postoperative VCP rate and progressive extent of surgery is well described. Historically, lobectomy was compared with lesser, parenchyma-sparing resections [20, 34]. Likewise, higher rates of VCP in ‘high-risk’ thyroid surgery are reported; however, no uniform definition of ‘high-risk’ thyroid surgery is globally accepted. In view of this study and the importance of functional nerve integrity, a hierarchy of progressive risk classes in regard to VCP in thyroid surgery starts with lobectomy and then proceeds to primary malignant, redo benign, and redo malignant surgery, and is topped by contralateral lobectomy with central lymph node dissection in pre-existing unilateral VCP. Goretzki et al. [24] described an incidence of pre-existing VCP of 0.6 % in a series of thyroid patients, 0.3 % in those undergoing primary surgery, and 3.5 % in those undergoing recurrent surgery. In the present large series, pre-existing VCP accounted for 3.5 % of thyroid procedures performed, representative of a uniquely highly specialized tertiary referral center in endocrine surgery with a considerable proportion of demanding and redo procedures in benign and malignant cases. Maximum challenging surgery, with contralateral lobectomy with and without lymph node dissection, accounted for 51 % of this series (Table 2). Benefit–risk evaluation in these patients led to stratification of surgical procedures, and minimum resection on the contralateral side to the prevalent VCP was performed in 33 (12 %) patients. However, in 205 (72 %) patients, a full risk exposure of the remaining functional VC was undertaken by lobectomy with or without concurrent lymph node dissection. Overall, consequent standard application of IONM in this series produced acceptable complication rates in regard to new VCP in maximum challenging thyroid surgery, with 1.75 % new VCP.
Bilateral VCP represents the most critical complication of thyroid surgery, with a high risk of compulsory tracheostomy, and significantly contributes to liability suits in endocrine surgery [35]. The total number of tracheostomy in this series was ten and these had to be performed for a variety of reasons (Table 5). Tracheostomy was assumed necessary intraoperatively in three, in two in consequence of laryngectomy. Postoperative tracheostomy was performed due to necrosis of muscle flaps after tracheal resection in two and for respiratory insufficiency in another three patients. In strict correlation to contralateral surgery in pre-existing VCP, the six patients who required tracheostomy due to surgical maneuvers represent 4.1 %. Notably, tracheostomy was not necessary in all bilateral VCP, and tracheostomy was not only performed for bilateral VCP in this series.
Visual identification of an anatomically intact RLN does not provide information on residual function or electrical conductivity. Conversely, positive IONM in established VCP supports efforts to preserve dysfunctional RLNs despite impaired VC function. Positive IONM in VCP may represent residual neural function in the form of electrical conductivity. The strength to produce an EMG can possibly influence postoperative quality of voice by retaining a stimulus to the intralaryngeal muscles, and to some degree prevent VC involution as described by Chi et al. [36]. In cases of near-normal EMG in nonfunctional VCP, it may furthermore be assumed that residual electrical conductivity also harbors the potential for preservation of laryngeal sensitivity, and therefore may assist in preventing silent aspiration with development of respiratory failure.
In regard to possible causes of VCP, data did not allow for a reliable analysis, as initial surgical notes either did not elaborate on intraoperative lesion or were not available, and, in the patients who had not been exposed to cervical surgery, remained idiopathic. According to the findings of preliminary data in CIONM, in cases of macroscopic intact RLNs without incidence of direct injury due to mechanical or thermal affection, traction injury is the most likely mechanism of injury. In cases of extralaryngeal branching, a solitary damage to the anterior branch of the nerve may be responsible for postoperative VCP in anatomically preserved RLNs; however, these data could not be assessed in this series [28, 36, 37].
The present study clearly demonstrated that preoperative laryngoscopy is indispensable for the use of IONM, and that initial significantly reduced amplitudes may indicate impaired VC function. Routine application, adherence to international standards inclusive of pre- and postoperative laryngoscopy, and knowledgeable solution of pitfall algorithm are prerequisite for realizing the full benefit of IONM in current clinical practice of thyroid surgery. Comprehensive implementation of the previous resulted in recognition of the importance of intraoperative IONM parameters as valuable information regarding pertinent functional status and possibly indicating imminent impairment of RLN function.
References
Snyder SK, Hendricks JC (2005) Intraoperative neurophysiology testing of the recurrent laryngeal nerve: plaudits and pitfalls. Surgery 138:1191–1192
Randolph GW, Dralle H, International Intraoperative Neural Monitoring Study Group et al (2011) Electrophysiologic recurrent laryngeal nerve monitoring during thyroid surgery and parathyroid surgery: international standards guideline statement. Laryngoscope 121:S1–S16
Chan WF, Lang BH, Lo CY (2006) The role of intraoperative nerve monitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1,000 nerves at risk. Surgery 140:866–873
Tomoda C, Hirokawa Y, Uruno T et al (2006) Sensitivity and specificity of intraoperative recurrent laryngeal nerve stimulation test for predicting vocal cord palsy after thyroid surgery. World J Surg 30:1230–1233. doi:10.1007/s00268-005-0351-z
Shindo M, Chheda NN (2007) Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg 133:481–485
Hopkins SK, Gal TJ, Brennan JA (2007) Prevalence and patterns of intraoperative nerve monitoring for thyroidectomy. Otolaryngol Head Neck Surg 136:954–956
Dralle H, Sekulla C, Lorenz K et al (2008) Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 32:1358–1366. doi:10.1007/s00268-008-9483-2
Sturgeon C, Sturgeon T, Angelos P (2009) Neuromonitoring in thyroid surgery: attitudes, usage patterns, and predictors of use among endocrine surgeons. World J Surg 33:417–425. doi:10.1007/s00268-008-9724-4
Dralle H, Lorenz K (2010) Intraoperative neuromonitoring of thyroid gland operations: surgical standards and aspects of expert assessment. Chirurg 81:612–619 (in German)
Chiang FY, Lee KW, Chen HC et al (2010) Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid surgery. World J Surg 34:223–229. doi:10.1007/s00268-009-0316-8
Yarborough DE, Thompson GB, Kasperbauer JL et al (2004) Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery 136:1107–1115
Hermann M, Hellebarth C, Freissmuth M (2004) Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiologic responses for the prediction of recurrent laryngeal nerve injury. Ann Surg 240:26–27
Schneider R, Randolph GW, Sekulla C et al (2013) Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck 35:1591–1598
Sadowski SM, Soardo P, Leuchter I et al (2013) Systematic use of recurrent laryngeal nerve neuromonitoring changes the operative strategy in planned bilateral thyroidectomy. Thyroid 23:329–333
Melin M, Schwarz K, Lammers BJ et al (2013) IONM-guided goiter surgery leading to two-stage thyroidectomy: indication and results. Langenbecks Arch Surg 398:411–418
Lorenz K, Sekulla C, German Monitoring Study Group et al (2010) What are normal quantitative parameters of intraoperative neuromonitoring (IONM) in thyroid surgery? Langenbecks Arch Surg 395:901–909
Lamade W, Ulmer C, Rieber F et al (2011) New backstrap vagus electrode for continuous intraoperative neuromonitoring in thyroid surgery. Surg Innov 18:206–213
Van Slycke S, Gillardin JP, Brusselaers N et al (2013) Initial experience with S-shaped electrode for continuous vagal nerve stimulation in thyroid surgery. Langenbecks Arch Surg 398:717–722
Bergenfelz A, Jansson S, Kristofferson A et al (2008) Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg 393:667–673
Dralle H, Sekulla C, Haerting J et al (2004) Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery 136:1310–1322
Chandrasehkhar SS, Randolph GW, Seidman MS et al (2013) Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg 148:S1–S37
Loch-Wilkinson TJ, Stalberg PL, Sidhu S et al (2007) Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg 77:377–380
Higgins TS, Gupta R, Ketcham AS et al (2011) Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope 121:1009–1017
Goretzki PE, Schwarz K, Brinkmann J et al (2010) The impact of intraoperative neuromonitoring (IONM) on surgical strategy in bilateral thyroid diseases: is it worth the effort? World J Surg 4:1274–1284. doi:10.1007/s00268-009-0353-3
Brauckhoff M, Machens A, Sekulla C et al (2011) Latencies shorter than 3.5 ms after vagus stimulation signify nonrecurrent inferior recurrent laryngeal nerve before dissection. Ann Surg 253:1172–1177
Dralle H, Damm I, Scheumann GF et al (1994) Compartment-oriented microdissection of regional lymph nodes in medullary thyroid carcinoma. Surg Today 24:112–121
Barczyński M, Randolph GW, Cernea CR, Dralle H, Dionigi G, Alesina PF, Mihai R, Finck C, Lombardi D, Hartl DM, Miyauchi A, Serpell J, Snyder S, Volpi E, Woodson G, Kraimps JL, Hisham AN (2013) External branch of the superior laryngeal nerve monitoring during thyroid and parathyroid surgery: International Neural Monitoring Study Group standards guideline statement. Laryngoscope 123:1–14
Casella C, Pata G, Nascimbeni R et al (2009) Does extralaryngeal branching have an impact on the rate of postoperative transient or permanent recurrent recurrent laryngeal nerve palsy? World J Surg 33:261–265. doi:10.1007/s00268-008-9832-1
Barczynski M, Konturek A, Cichon S (2009) Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 96:240–246
Cernea CR, Bandao LG, Hojaij FC, DeCarlucci D, Brandao J, Cavalheiro B, Sondermann A (2010) Negative and positive predictive values of nerve monitoring in thyroidectomy. Head Neck 34:175–179
Chan WF, Lo CY (2006) Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 30:806–812. doi:10.1007/s00268-005-0355-8
Jarhult J, Lindestad PA, Nordenstrom J et al (1991) Routine examination of the vocal cords before and after thyroid and parathyroid surgery. Br J Surg 78:357–360
Randolph GW, Kamani D (2006) The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery 139:357–362
Rosato L, Avenia N, Bernante P et al (2004) Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 28:271–276. doi:10.1007/s00268-003-6903-1
Dralle H, Lorenz K, Machens A (2012) Verdicts on malpractice claims after thyroid surgery: emerging trends and future directions. Head Neck 34:1591–1596
Chi SY, Lammers B, Boehner H et al (2008) Is it meaningful to preserve a palsied recurrent laryngeal nerve? Thyroid 18:363–366
Serpell JW, Yeung MJ, Grodski S (2009) The motor fibers of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg 249:648–652
Conflict of interest
All authors declare no potential or real conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Kerstin Lorenz and Mohammed Abuazab have equal authorship.
Rights and permissions
About this article
Cite this article
Lorenz, K., Abuazab, M., Sekulla, C. et al. Results of Intraoperative Neuromonitoring in Thyroid Surgery and Preoperative Vocal Cord Paralysis. World J Surg 38, 582–591 (2014). https://doi.org/10.1007/s00268-013-2402-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-2402-1