Abstract
Background
Intraoperative nerve monitoring (IONM) of the recurrent laryngeal nerve and the vagal nerve can detect nonfunctioning nerves (recurrent laryngeal nerve palsy, RLNP) that are visibly intact. The use of IONM is questionable, however, as we still lack evidence that it reduces the rate of postoperative nerve injuries. Since negative IONM results after thyroid dissection of the first side could change our surgical strategy and thus could prevent patients from bilateral RLNP, we questioned whether IONM results are reliable enough to base changes in surgical strategy and whether this has any effect on surgical outcome.
Methods
We retrospectively analyzed the data of 1333 consecutive patients with suggested benign bilateral thyroid disease who had been operated on under a defined protocol, including the use of a specific IONM technique (tube electrodes and stimulation of the vagal nerve and the inferior recurrent nerve before and after thyroid resection), between January 1, 2006 and December 31, 2008.
Results
In four patients the IONM system did not work, two nerves had not been found, and in eight patients the tube had to be readjusted. Of five permanent nerve injuries, four were visible during surgery and one was suspected. Sensitivity of IONM in detecting temporary nerve injuries of macroscopically normal-appearing nerves was 93%. Specificity was 75–83% at first side of dissection and 55–67% at the second side, with an overall specificity of 77%. In 11 of 13 patients (85%) with known nerve injury (preexisting or visible) and in 20 of 36 patients (56%) with negative IONM stimulation at the first side of dissection, the surgical strategy was changed (specific surgeon or restricted resection) with no postoperative bilateral RLNP. This was in contrast to 3 of 18 (17%) bilateral RLNP (p < 0.05), when surgeons were not aware of a preexisting or highly likely nerve injury at the first side of thyroid dissection.
Conclusions
Failed IONM stimulation of the vagal or recurrent laryngeal nerve after resection of the first thyroid lobe is specific enough to reconsider the surgical strategy in patients with bilateral thyroid disease to surely prevent bilateral RLNP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent laryngeal nerve palsy (RLNP) is still a major problem in thyroid surgery. It may become a life-threatening disaster, however, when it occurs bilaterally. This problem may not exist in units with only specialists in endocrine surgery operating, but it still occurs with a frequency of 0.2–0.8% in academic and educational hospitals with a large workflow [1, 2]. Since RLNP occurs even when the nerve has been visibly identified and preserved, we questioned whether intraoperative nerve monitoring (IONM) could surely prevent patients from bilateral RLNP when total or subtotal thyroid gland resection is attempted [2–8]. Thus, IONM may help to identify patients with unilateral vocal cord paralysis (VCP) after dissection of the first side [2–8], but the high rate of false pathologic findings in IONM jeopardizes possible consequences [5, 7]. Some authors questioned whether changes in operative strategy can be based on these rather vague results [5]. Having used different IONM techniques in more than 1000 thyroid operations since 1998, we now follow a strict protocol that includes IONM in all thyroid operations. This retrospective analysis of more than 1000 patients demonstrates that surgeons intending to perform bilateral thyroid operations for primarily benign thyroid diseases should respond to negative nerve stimulation by IONM at the first side of thyroid dissection. Even when no reason for nerve injury can be found and nerve visualization has been optimal, nerve injuries are possible [2, 3]. In most of these cases, a two-stage operation is advisable in order not to jeopardize the final outcome with a temporary bilateral RLNP.
Material and methods
Patients
Of 2022 patients operated on between January 1, 2006 and December 31, 2008 for thyroid diseases, 197 patients (9.7%) had proven thyroid malignancy and 486 (24.0%) had only unilateral thyroid disorders. Both groups were excluded from further investigation, leaving 1339 of the 2022 patients (66.2%) for inclusion in the study. In 2 of the 1339 patients with bilateral disease, the inferior laryngeal nerve was not found at operation, and in 4 patients technical IONM equipment was defective and could not be repaired during the operation. These six patients showed normal vocal cord movement postoperatively but were also excluded from the study, leaving 1333 patients for further evaluation (Table 1). Four of these patients (0.3%) had a nonrecurrent inferior laryngeal nerve at the right side that we did not see on the left side. The number of patients with early bifurcation of laryngeal nerves was not documented systematically.
Methods
Different neuromonitoring devices (IONM) have been used by us to control the intraoperative function of the inferior laryngeal nerve (recurrent laryngeal nerve, RNL) since 1998. Techniques in which electrodes are inserted into the vocal muscles and techniques in which electrodes surround the tracheal tube were tested in more than 1000 patients (in the first few years these techniques were used only for patients with difficult operations). In 2005, a standard protocol for all further thyroid operations was approved and the use of IONM devices and dissection devices in all thyroid operations was required.
The protocol included the indication for thyroid surgery, the diagnosis and analysis of thyroid function, preoperative thyroid ultrasonography with optional scintigraphy, and a preoperative transoral laryngoscopy by an ENT specialist. The operation started with intubation of patients using an IONM-specific tracheal tube (Medtronic, Jacksonville, FL, USA), and anesthesiologists were instructed to restrain from the use of long-acting muscle relaxants. Then a 4–6-cm collar transverse incision was made, strap muscles were divided in the midline, and the carotid artery, cephalic vein, and vagal nerve were visualized at the predominant thyroid side [side of the goiter or questionable malignant nodule(s)] lateral to the upper thyroid pole. Stimulation of the vagal nerve with registration of the result on paper (V1) followed, and a vessel loop was placed around the nerve. All stimulations of the vagal nerves and the inferior laryngeal nerves were performed with a current amplitude of 1 mA. Stimulation was judged positive when a characteristic stimulation curve could be registered with a peak altitude of more than 100 µV.
After dissecting of the upper side of the thyroid lobe with dissection devices (Precise® as described before [9]), the inferior laryngeal nerve was visualized caudal to the lower thyroid pole. The inferior laryngeal nerve was stimulated by IONM and the result was registered (R1). During further dissection of the thyroid lobe, the vagal nerve as well as the inferior laryngeal nerve may have been checked again; doing so was optional to the needs of the operating surgeon (Vx; Rx). After thyroid lobe resection the inferior laryngeal nerve and the vagal nerve were stimulated again and the results were registered (R2, V2). The second lobe was dissected and nerve activity was registered as described for the first side.
Negative IONM stimulation was defined as failure to create a typical stimulation curve when using a current amplitude of 1 mA. Loss of signal was defined as total loss of the primary normal stimulation curve or as reduced stimulation amplitude to less than 100 μV.
In the case of negative IONM signals, the responsible surgeon (registered general surgeon or specialist in endocrine surgery) was free to decide whether to proceed with the operation as intended or whether to change the operative strategy. Changed operative strategy included calling for the most experienced surgeon in endocrine surgery to take over the operation or finishing the surgery after resection of only one thyroid lobe with or without only partial resection (less than subtotal means the rest of more than 2–3 ml) of the other side.
After a primary postoperative check of vocal cord activity by the anesthesiologist during extubation, all patients with preoperative VCP, visible or questionable injury during dissection of the vagal or inferior laryngeal nerve, visible normal nerves but negative IONM stimulation, pathologic findings at microlaryngoscopy during extubation, and objective or subjective voice changes were investigated by ENT specialists using direct laryngoscopy. This was performed at the ENT clinic of our hospital the day after surgery. All other patients were advised to see the primary ENT specialist for postoperative laryngoscopy during the first week after surgery.
In case of VCP or major mobility dysfunction of the vocal cords (also categorized as vocal cord paralysis if no direct injury by intubation could be proven), speech therapy (logopedic therapy) was initiated and ENT investigations with direct laryngoscopy were repeated after 1, 2, 3, 4 weeks, and 2, 3, 6, 12, and 18 months postoperatively, or until definite full recovery of vocal cord movement. Vocal cord paralysis 18 months after thyroid surgery was defined as permanent.
The data of all patients were registered prospectively, inserted into a database (Excel, Microsoft Corp., Redmond, WA, USA), and evaluated by using descriptive statistical analysis. Differences between results of groups were analyzed using Fisher’s exact test and were accepted as different when the significance level of greater than 95% was reached.
Results
The female-to-male ratio in the 1333 patients with bilateral disease was 3.2 to 1 with 1019 women (76.4%) and 314 men (23.6%). Age ranged between 6 and 97 years, with a mean ± standard deviation of 51.7 ± 14.4 years. In 1219 patients (91.4%) the operation was the first and in 114 patients (8.5%) it was the second, third, or fourth thyroid operation. Histology was similar in both groups (Table 2).
Preexisting VCP and RLNP
Eight of 1333 patients (0.6%) demonstrated preoperative unilateral VCP. It was diagnosed in 4 of the 1219 patients (0.3%) who underwent a primary thyroid operation and in 4 of the 114 patients with recurrent disease (3.5%) (Table 1). Unilateral VCP was due to compression of the nerve by an enlarged thyroid gland in three of four patients with primary disease and to surgical injury during the first thyroid operation in all four patients with recurrent disease. One patient (BK) who had a primary thyroid operation had suffered from a central stroke and thus had developed VCP (Table 3).
In BK and in another patient (MR) with permanent VCP after the first thyroid operation, IONM was positive for vagus and inferior laryngeal nerve stimulation at the side of VCP. Thus, two of eight (25%) patients with long-standing permanent laryngeal nerve paralysis demonstrated false-positive IONM for vagal and inferior laryngeal nerve (Table 1).
In one patient (BKK), preoperative laryngoscopy had shown unilateral VCP and contralateral decreased vocal cord activity. In addition, tracheal malacia was proven and the patient suffered from stridor preoperatively. IONM was negative for both nerves at first but became positive on the second side during surgery. Vocal cord examination the day after surgery demonstrated minimal vocal cord disturbances, with normal findings at the second side 1 week later. Vocal cord function contralateral to the paralyzed side was thus normal in all cases postoperatively (Table 3).
A visible injury of the inferior laryngeal nerve occurred in 5 of the remaining 1215 patients (0.4%) with bilateral disease and who had a primary operation and in none of the 110 patients with recurrent disease (Table 1). The injury was assigned to the first side in four patients and to the second side in one patient (Table 3). It was confirmed by loss of IONM stimulation proximal to the dissection area. In two (AM and FN) of these five patients the upper branch of an early divided inferior laryngeal nerve was injured, in one patient (TG) the recurrent nerve was stretched due to blunt mediastinal dissection of the deep-reaching thyroid capsule, and in two patients (SS and QG) a direct cut of the recurrent laryngeal nerve was visible. In one (AM) of the four patients with nerve injury at the first side, surgery was terminated after unilateral resection, and in two patients the operation proceeded with partial resection of the second side. All four patients demonstrated permanent VCP at 12–18 months postoperatively, with normal function of the opposite vocal cord (Table 3).
Visible normal but nonfunctioning RLN/VCP
In ten patients (0.8%) with normal vocal cord movement at both sides, vagal and inferior laryngeal nerve stimulation curves were primarily negative because of the use of relaxants by the anesthesiologist in two patients, and they showed absence of a signal during the operation caused by tracheal tube dislocation in eight patients. In all these patients IONM signals recovered during the operation and postoperative bilateral vocal cord movement was normal, as expected (Table 1).
Forty-six of 1321 patients (3.5%) with visible intact nerves demonstrated pathologic IONM signals during surgery. In 36 patients this was seen at first side of the thyroid operation, in 10 patients at the second side, and in 3 patients at both sides. Forty of these 52 nerves at risk (77%) showed VCP postoperatively (Tables 4 and 5). Vocal cord paralysis occurred to the first dissected side in 30 of 36 patients (83.3%) with pathologic IONM and to the second side in 10 of 16 (63%) (Table 4).
Sensitivity and specificity of IONM
IONM at first side of dissection showed vanishing stimulation curves in 22 patients with vagal stimulation and in 14 patients with RLN stimulation, and it could not be restored by tracheal tube readjustment. Vocal cord paralysis was proven in 19 of the 22 patients (86%) and 13 of the 14 patients (93%), respectively (Tables 4 and 5).
In addition to the 30 patients with pathologic IONM signals at the first side, two patients with visible normal nerves and normal IONM stimulation curves suffered from VCP postoperatively (2 of 1285 = 0.16% false normal IONM curves). The same happened to one patient after dissection of the second side (1 of 1327 = 0.08% false normal IONM stimulation). The predictive value for normal RLN function thus was 99.8% for the first side and 99.9% for the second side of operation.
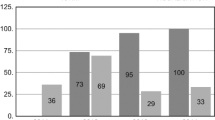
Sensitivity and specificity of IONM were 30 of 32 (94%) and 30 of 36 (83%) for the first side of dissection, and 10 of 11 (91%) and 10 of 16 (63%) for the second side of thyroid dissection, respectively (Table 5).
Change of operative strategy
Thyroid surgery in all eight patients with preexisting unilateral VCP was performed by endocrine surgery specialists (3 of the 12 different surgeons who performed the operations). It started at the side of the paralyzed vocal cord, and in one patient surgery was restricted to this side. Four of eight patients underwent total thyroidectomy, and in three patients thyroidectomy on one side (hemithyroidectomy) was combined with partial resection on the opposite side (Table 3). The policy for changing the surgical strategy in case of unilateral nerve injury was to call in the most experienced surgeon in charge. This occurred in four of five patients (80%).
Altogether, changes in operative strategy for patients with known unilateral VCP were undertaken in 12 of 13 cases (92%), and a less radical approach was chosen for the second side in 6 of 12 patients (50%) (Table 6). Under these circumstances no further problems at the second side of operation occurred. In one patient with preoperative stridor and bilateral problems in IONM (BKK), the danger of possible bilateral VCP resolved directly and vocal cord movement was normal within 1 week due to decompression, as mentioned above (Tables 3, 6).
After pathologic IONM signals were seen at first side, thyroidectomy in three patients was continued almost as intended but by a more experienced surgeon. In one of these three patients and in an additional two patients, hemithyroidectomy of the first side was combined with only partial contralateral resection. In 15 of these 20 patients (75%) surgery was restricted to only hemithyroidectomy (Table 6). In nine patients resection of the other side was performed after full recovery of the normal vocal cord movement 1 day to 4 months after the first operation. One patient is still scheduled for hemithyroidectomy of the other side and in five other patients no further operation is intended.
None of the 20 patients whose operative procedure was adjusted after the first thyroid side dissection suffered from bilateral VCP postoperatively (Table 6). Altogether, 18 of 20 patients (90%) with changes in surgical strategy proved to have unilateral VCP postoperatively (Tables 4 and 6).
In 16 of 36 patients (44%) with pathologic IONM findings at the first thyroid side, the surgeons did not change their strategy, nor did they call for further help. In four of these 16 patients (25%), postoperative laryngoscopy proved intact vocal cord movement bilaterally the day after surgery. In 9 of the 16 patients (56%), VCP of the first side was confirmed and persisted for 1 week to 3 months. Three of these 16 patients (19%), however, suffered from bilateral vocal cord paralysis for 1–9 weeks postoperatively (Table 6). In two of these three patients the operation proceeded as intended because muscle contractions at the larynx were demonstrable during vagal nerve stimulation, leading to the wrong suggestion of a false-negative IONM finding. None of the three patients with early postoperative bilateral VCP had to have a tracheostomy, and bilateral vocal cord movement regained normal activity within 4 weeks to 14 months (Table 6).
Postoperative voice changes
Fifteen patients with normal IONM findings but subjectively changed voice quality were investigated by direct laryngoscopy the day after surgery. Of these 15 patients, 2 had unilateral VCP at the first side and 1 at the second side for 1 week to 3 months (Table 4; pat. Nr. 46–48). Four patients suffered from swelling of the larynx and vocal cords postoperatively, which was interpreted as intubation injury. No reason for the notable voice problem in eight patients was found by us or by the postoperative ENT specialist, including by measurements of the superior laryngeal nerve by stroboscopy.
VCP after postoperative bleeding
In addition to the 36 patients with pathologic IONM, the 5 patients with visible nerve injury, and the 3 patients with unexpected postoperative RLNP, 3 other patients demonstrated VCP postoperatively. All three patients, who primarily had a normal voice, had to be reoperated on because of acute postoperative bleeding. Revision surgery had to be performed in 19 patients (19 of 1333 = 1.4%), including these 3. Thus, 3 of 19 patients (16%) with reoperation for bleeding developed RLNP. Of these three patients, two had VCP at one side (one at first primary side and one at secondary side) and one patient suffered from bilateral RLNP. The latter patient was treated by tracheostomy to prevent suffocation and was the only one of our 1839 patients (0.05%) with postoperative tracheostomy. In all three patients vocal cord movement regained normal activity within 2 weeks to 2 months, and the tracheostomy was closed 8 weeks after reoperation with no further operative complications.
Altogether, 5 of 1333 patients (0.4%) with bilateral thyroid disease suffered from permanent unilateral vocal cord paralysis, with 4 patients at the first side of dissection and 1 patient at the second side. In 46 patients with transient VCP, 32 (69%) were at first side and 9 (20%) at the second side, with 5 patients (11%) showing temporary bilateral vocal cord paralysis. Three of 5 with bilateral temporary RLNP could have been prevented when the negative IONM findings at the first side would have caused the operative strategy to change, as in 20 other patients.
With respect to specificity and sensitivity of VCP and IONM findings, all permanent nerve injuries as well as 93% of all transient nerve injuries were demonstrated by a negative IONM signal. False-negative findings were diagnosed in about 20–30%; however, this varied depending on time and location of IONM (Table 5).
Nerve injuries at the second side were visible in only 1 of 1325 patients (0.08%) who were operated on bilaterally, and negative IONM findings were registered in 16 patients (1.2%). Vocal cord paralysis was diagnosed in 10 of these 16 patients (63%). An undetected VCP at the second side was proven in only 1 of our patients (0.08 %), and in 10 of 11 patients (81%) a temporary vocal cord paralysis of the second side was diagnosed by IONM (Table 5).
Discussion
Meticulous surgery, experience, and specialization have steadily reduced temporary and permanent inferior laryngeal nerve paralysis (RLNP) in thyroid surgery [1–3, 9–11]. It still occurs occasionally, however, and can become a disaster when it occurs bilaterally—some patients end up having a tracheostoma and some have to go to ICU for days. Therefore, IONM may help prevent this despite the fact that it is still debatable whether IONM reduces transient and permanent unilateral RLNP [2–6, 8, 11–14]. Our present data do not support the hypothesis that IONM has a significant impact on permanent or transient unilateral RLNP in our patients compared to earlier results [1, 14]. As visible nerve preparation had always been an integral part of our surgical technique, we primarily suggested—before starting our study—that a reduction of RLNP via IONM may be demonstrable only in difficult cases such as those with nerves sticking to surrounding tissue and covered by scar tissue (i.e., reoperations). This is in contrast with the findings of Barczynski et al. [4]. They performed a prospective randomized trial in 500 patients with and 500 patients without IONM and could reduce total RLNP from 5.0 to 2.7% [4], a percentage identical to that which we registered before the use of IONM in our patients [14]. In the study by Barczynski et al., permanent RLNP was diagnosed in 12 of 50 patients (24%) with postoperative RLNP in whom IONM was not used and in 8 of 27 patients (30%) with postoperative RLNP in whom IONM was used [4]. Both results of permanent RLNP in relation to postoperative RLNP are quite high compared to our experience in which there was permanent RLNP in 5 of 66 patients with RLNP (8%).
The significant number of patients with visibly undamaged but nevertheless nonfunctioning nerves (45 of 2647 = 1.7%) was surprising to us but has been reported by others [2, 3, 8, 15] with a rate of 0–7.1%. Because the situation of a normal-appearing but nonfunctioning RLN can play an important role in deciding the direction of the operation in benign thyroid disease, most German surgeons who use IONM were not willing to take part in a prospective randomized trial of the use of IONM in thyroid surgery [2]. IONM is of little help in patients with visible nerve injuries (0.2% in our study and 0–2.5% in the present literature) [2, 3, 15] and only proves the existing problem. Therefore, many surgeons questioned whether IONM is useful at all [7, 12].
We asked whether IONM can help revise our surgical strategy for patients with benign multinodular goiter and visible unexpected nerve injury at the first side of thyroid dissection to prevent a possible bilateral RLNP. This is different for patients with malignant thyroid disease where increased risks may be acceptable. Investigating the impact of IONM on the surgical strategy for benign multinodular goiter, the study had to meet the requirements of our educational demands (12 different surgeons performing thyroid surgery and outside surgeons being trained in thyroid surgery) and that of a large workflow of more than 1000 thyroid operations per year. Surgery was therefore not restricted to specialists in endocrine surgery as in other studies [4].
Requisite for the influence of IONM on surgical strategy was a high specificity and sensitivity of pathologic IONM results in demonstrating vocal cord paralysis (VCP). Our earlier experiences showed that sensitivity was not a problem but specificity was, as noticed by many other authors [2–8]. Only increasing knowledge in the use of one specific technique (tube electrodes) and experience with more than 1000 thyroid operations over a period of 5 years enabled us to reduce false-positive results from pathologic IONM to less than 25% at the first side of dissection (Table 5). In particular, the problems of tube malrotation, tube insertion that is too deep or too high, and the use of an improper tube size (too small) by the anesthesiologist could be diminished, as it has been shown by Dionigi et al. [13]. It was supposed from our earlier experience, and now confirmed, that necessary readjustment of the tracheal tube occurs more often in men (7 of 315 = 2.2%) than in women (1 of 1024 = 0.1%) (p < 0.001); to our knowledge this has not yet been reported. We also had a different specificity of IONM results, depending on the time of testing (start of operation, after resection) and the nerve being tested (vagal nerve, inferior laryngeal nerve) (Table 5). Earlier studies concentrated on the comparison of results in direct (inferior laryngeal nerve) and indirect (vagal nerve) nerve stimulation but did not assess results at different stages of the operation (Table 3) [2–5]. In particular, differences between IONM data from the first side and the second side of thyroid dissection have not been shown this definitively before (Table 5).
In this article we intentionally did not focus on differentiating results in low-risk and high-risk patients, although 444 of 1339 of our patients (33%) would have met the criteria for high-risk patients of other groups (recurrent operation, mediastinal extension, large goiter size “III”, thyroiditis, and Graves’ disease) (Table 2) [4, 16]. Instead, we focused on the impact of IONM results on surgical strategy after resection of the first thyroid lobe.
Chiang et al. [5] reported that 5 of 12 patients (42%) with pathologic IONM results regained normal nerve activity during surgery, and in only 4 patients normal vocal cord mobility, judged as false-negative stimulation, was demonstrated during surgery. We saw very early recovery of nerve activity and vocal cord movement or false pathologic IONM in 9 of 48 patients (19%) (Table 1). In contrast to Chiang et al., we used direct laryngoscopy by ENT as control the day after surgery. This was done because intraoperative microlaryngoscopy was not precise enough, in our hands, as has been demonstrated by others [17, 18]. Therefore, early recovery during wound closure might have occurred in some of our patients with “false-negative stimulation” results (Table 1). Since direct laryngoscopy is accepted as the gold standard for measuring vocal cord movement and since we lack a specific voice analysis program [19], we also investigated all patients (n = 15) with subjective and objective changes of voice quality by direct laryngoscopy (3 of 15 had RLNP).
Recovery of all macroscopic normal-appearing inferior laryngeal nerves with negative stimulation results was surprisingly high (46 of 47) compared to special patient cohorts with vocal cord paralysis, for whom full recovery was reported as low as 18–61% [17]. Good results comparable to our data were reported by Chiang et al. [5] with recovery in all 15 (100%) of his patients with visible undamaged nerves. Permanent laryngeal nerve paralysis was caused by direct operative injury in four of five patients (5 of 1333 = 0.4%). These include two patients with injury to the anterior branch of the RLN only and two patients with injury to the main RLN. Anterior branch injury results in permanent RLNP since all motor fibers of the RLN are positioned in the anterior branch when an early extralaryngeal branching of the inferior laryngeal nerve is present [20]. Preserving other nerve branches may not be trivial, however, as we showed in four patients with long-standing VCP and who underwent necessary reoperation [21].
In only one of our patients (TG) with permanent VCP, vigorous blunt dissection of the mediastinal thyroid gland caused stretching of the nerve that resulted in a probably permanent axonal injury [22]. This patient is the only one of our 1333 patients in whom permanent vocal cord paralysis was not visible during surgery.
Despite surgical nerve adjustment in three patients and long-term logopedic therapy in all five patients with direct nerve injury, vocal cord movement was still impeded in all five patients 1 year after surgery. Whether electromyographic investigations can terminate ineffective logopedic therapy earlier, as shown by Grosheva et al. [17], or whether locally applied growth factors may increase the probability of nerve regeneration, as demonstrated in animal models [22–24], will have to be proven in future.
Because our protocol included direct laryngoscopy in all patients with known primary changes of vocal cord movement, with pathologic intraoperative IONM results and with postoperative objective or subjective voice changes, we did not perform direct laryngoscopy in the other patients postoperatively. This weakens our results with respect to the absolute number of VCP. The results of Ortega et al. [19], using specific voice analysis and the results of many authors who used IONM [2–8], demonstrated that false-negative results have become a minor problem and merge to less than 20% under the stated investigation protocol [2–8, 17–19].
Altogether, negative IONM stimulation at the first side of dissection is specific and sensitive enough to predict early postoperative vocal cord paralysis with more than 70% certainty (Table 6). Whether this could also reduce the risk of possible bilateral vocal cord paralysis has not been proven yet. Therefore, we left it up to the surgeon in charge whether to change the surgical strategy in case of negative IONM results at the first side. In 16 of 36 patients (44%) the surgeons did perform the surgery as intended, and, surprising to us, the possibility of bilateral vocal cord paralysis after knowledge of IONM negative results at the first side of dissection rather increased compared to normal findings at the first thyroid side (Table 4) (3 of 16 = 19% vs. 7 of 1311 = 0.5%; p < 0.001) (Table 5).
The experience of three temporary bilateral RLNP during ongoing surgery as intended also contrasts our experience with patients with preexisting vocal cord paralysis. A contralateral nerve injury did not occur (p < 0.05) in any patient when surgery was taken over by a endocrine surgery specialist (Table 6).
The increased risk of injuring the contralateral nerve was not caused by postoperative bleeding, as we have seen in three other patients [25, 26], but may be explained by differences in the personal skill of each surgeon or the needed experience in endocrine surgery, when special problems occur [3, 16]. It also could be attributed to an increased stress reaction of surgeons when nerve injury has almost certainly already happened at the first side of dissection. Other explanations for an increased risk to the contralateral nerve, such as goiter extent to the mediastinum, increased goiter size, tissue adhesion in thyroiditis, or increased nerve sensitivity in some patients (i.e. Graves’ disease) is not supported by our findings [27–29].
Despite the fact that these data are still scanty, they moved us to prohibit the continuation of the surgery by the same surgeon when a negative IONM signal is noticed after resection of the first thyroid lobe. Whether they call in a specialist for endocrine surgery or terminate the operation and wait for ENT results has to be judged individually. The data, however, support a hemithyroidectomy or a two-stage operation, as it has been performed in 15 of our 20 patients (75%) with adjusted operations.
To our knowledge, the present study is the first that demonstrates the importance of IONM results in patients with visible normal-appearing but nonfunctioning nerves after resection of the first thyroid lobe, when bilateral resection was the goal. Further surgery may be postponed in these patients in order not to risk bilateral vocal cord paralysis.
References
Röher HD, Goretzki PE, Hellmann P et al (1999) Complications in thyroid surgery. Incidence and therapy. Chirurg 70:999–1010
Dralle H, Sekulla C, Lorenz K et al (2008) Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 32:1358–1366
Hermann M, Hellebart C, Freissmuth M (2004) Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg 240:9–17
Barczynski M, Konturek A, Cichon S (2009) Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 96:240–246
Chiang FY, Lu IC, Kuo WR et al (2008) The mechanism of recurrent laryngeal nerve injury during thyroid surgery–the application of intraoperative neuromonitoring. Surgery 143:743–749
Sindo M, Chheda NN (2007) Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg 133:481–485
Chan WF, Lo CY (2006) Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 30:806–812
Thomusch O, Sekulla C, Machens A et al (2004) Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg 389:499–503
Goretzki PE, Schwarz K, Lammers BJ (2009) Implementing the general use of dissection devices in thyroid surgery from prospective randomized trial to daily use. Surg Technol Int 18:87–93
Bergenfelz A, Jansson S, Kristoffersson A et al (2008) Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3, 660 patients. Langenbecks Arch Chir 393:667–673
Randolph GW, Kobler JB, Wilkins J (2004) Recurrent laryngeal nerve identification and assessment during thyroid surgery: laryngeal palpation. World J Surg 28:755–760
Sturgeon C, Sturgeon T, Angelos P (2008) Neuromonitoring in thyroid surgery: attitudes, usage patterns, and predictors of use among endocrine surgeons. World J Surg 33:417–425
Dionigi G, Bacuzzi A, Boni L et al (2008) What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg 6:S7–S12
Goretzki PE, Dotzenrath C, Witte J et al (2000) Chirurgie des Morbus Basedow. Viszeralchirurgie 35:117–123
Agarwal G, Aggarwal V (2008) Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J Surg 32:1313–1324
Pieracci FM, Fahey TJ (2008) Effect of hospital volume of thyroidectomies on outcomes following substernal thyroidectomy. World J Surg 32:740–746
Grosheva M, Wittekindt C, Pototschnig C et al (2008) Evaluation of peripheral vocal cord paralysis by electromyography. Laryngoscope 118:987–990
Sittel C, Stennert E, Thumfart WF et al (2001) Prognostic value of laryngeal electromyography in vocal fold paralysis. Arch Otolaryngol Head Neck Surg 127:155–160
Ortega J, Cassinello N, Dorcaratto D et al (2009) Computerized acoustic voice analysis and subjective scaled evaluation of the voice can avoid the need for laryngoscopy after thyroid surgery. Surgery 145:265–271
Serpell JW, Yeung MJ, Grodski S (2009) The motor fibres of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg 249:648–652
Chi SY, Lammers B, Boehner H et al (2008) Is it meaningful to preserve a palsied recurrent laryngeal nerve? Thyroid 18:363–366
Hydman J (2008) Recurrent laryngeal nerve injury. Karolinska Institutet, Larserics Digital Print AB, Bromma, Sweden
Mattsson P, Björck G, Remahl S et al (2005) Nimodipine and microsurgery induced recovery of the vocal cord after recurrent laryngeal nerve resection. Laryngoscope 115:1863–1865
Moskalenko V, Hüller M, Gasser M et al (2009) Investigation of the regeneration potential of the recurrent laryngeal nerve (RLN) after compression injury, using neuromonitoring. Langenbecks Arch Surg 394:469–474
Rosenbaum MA, Haroidas M, McHenry CR (2008) Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg 195:339–343
Leyre P, Desurmont T, Lacoste L et al (2008) Does the risk of compression hematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg 393:733–737
Polednak AP (2009) Vocal fold palsy after surgery in elderly thyroid cancer patients with versus without comorbid diabetes. Surgery 144:688–689
Henry JF, Audiffret J, Denizot A et al (1988) The non-recurrent inferior laryngeal nerve: review of 33 cases, including 2 on the left side. Surgery 104:977–984
Weiand G, Mangold G (2004) Verlaufsvarietäten des Nervus laryngeus inferior. Chirurg 75:187–195
Disclosures
The clinic acts as an educational center for IONM for outside surgeons to be trained in the use of IONM in thyroid surgery and is supported financially by Medtronic, Germany. The authors were sponsored by Medtronic, Germany, when reporting their experience of IONM in thyroid surgery to the scientific community.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goretzki, P.E., Schwarz, K., Brinkmann, J. et al. The Impact of Intraoperative Neuromonitoring (IONM) on Surgical Strategy in Bilateral Thyroid Diseases: Is it Worth the Effort?. World J Surg 34, 1274–1284 (2010). https://doi.org/10.1007/s00268-009-0353-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0353-3