Abstract
Background
The aim of the present study was to analyze the results of our experience with elective placement of self-expandable metallic stents (SEMS) in patients with stage IV obstructing colorectal cancer. A systematic review of the literature was also carried out to analyze the factors influencing the results of SEMS placement and to determine if there has been any improvement in the more recent period.
Materials and methods
The results of a personal series of 100 patients were analyzed. There was no case of mortality or major morbidity. The systematic review included 27 articles published from April 2007 to December 2011.
Results
In our experience the technical success rate was 96 % and the clinical success rate was 92 %. During the follow-up period a repeat colonoscopy was needed in 31 % of the patients for recurrent symptoms of obstruction due to fecal impaction (19 %), tumor growth (8 %), or stent dislodgment (4 %). Review of the literature showed similar results, with a significant improvement in the reports of the last 6 years; procedures performed on an emergency basis had poorer results.
Conclusions
Self-expandable metallic stent placement offers a valid alternative to surgery in patients with obstructing stage IV colorectal cancer, but careful follow-up is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-expandable metallic stents (SEMS) are metallic tubes, which once placed at the level of the colorectal obstruction, expand to resume their primitive diameter. This natural expansion derives from the elasticity of the nickel-titanium compound Nitinol, which resumes its initial diameter at body temperature. The procedure presents many advantages in patients with stage IV colorectal cancer causing obstruction, in comparison with a diverting colostomy, which is associated with many negative psychological aspects. Self-expandable metallic stents can be placed under light sedation without the need for laparotomy with all its related matters; hospital stay is shorter, with reduced costs and less discomfort for the patient and his/her family [1–6]. In the last 12 years, we have resorted to this technique in patients with stage IV not resectable colorectal obstructing cancer.
Here we report our experience, which has the advantage of presenting the perspectives of surgeons and not, as usual, of gastroenterologists. A systematic review of the literature is also included.
Particular attention was paid to technical and clinical results of the procedure.
Materials and methods
From December 1999 to December 2011, 100 patients with stage IV colorectal cancer were treated at Department Pietro Valdoni with SEMS placement. They were prospectively evaluated. The cancer was located in the rectum or the sigmoid colon. The procedures were performed by one or two surgeons. The majority of the patients were referred from another hospital. All procedures were performed electively.
Inclusion criteria were (1) patients with proven adenocarcinoma, (2) symptoms of obstruction lasting longer than 3 months, (3) cancer causing significant reduction in lumen diameter, (4) stage IV disease as demonstrated by preoperative computed tomography (CT) scan, (5) procedure performed under elective conditions by experienced surgeon.
Patients had a diagnosis of obstructing sigmoid rectal cancer on the basis of preoperative colonoscopy with biopsies. A CT scan showed distant metastases, and the tumor was considered stage IV. All patients were fully evaluated, and any fluid or electrolyte imbalance was corrected before the procedure was carried out. A complete cardiologic and respiratory evaluation was conducted and the proper therapy started. All patients, except the ones with complete obstruction as determined by preoperative colonoscopy, underwent bowel preparation the day before the procedure (Golytely, Colite, Nulytely, 3 liters). A few hours before the procedure a low-pressure water enema was administered. The stent placement procedure was performed under light sedation with benzodiazepine at a dosage depending on the patient’s body weight.
SEMS placement
A guidewire was passed through the obstruction. In the initial experience the guidewire was passed blindly through the obstruction under fluoroscopic and endoscopic guidance. The guidewire was directed toward the obstruction with a colonoscope, which remained in position distal to the tumor, to avoid the risk of perforation. More recently we have adopted a modification of the technique in which a pediatric nasogastroscope (4.8 mm in diameter) is used to pass the obstruction. In this way it is possible to have direct vision of the anatomy and pathology, and to pass the guidewire above the obstruction through the nasogastroscope. This has made the procedure much simpler, faster, and, at least theoretically, has reduced the risk of perforation or bleeding. The SEMS apparatus (Precision Colonic Stent System, Boston Scientific Microvasive, Natick, MA) was placed at the level of the obstruction through the guidewire previously inserted, and finally deployed under fluoroscopic guidance. The length of the stent ranged from 9 to 12 cm. Initially we used the Ultraflex OTS stent; recently, we have used the Wallflex TTS stent (Boston Scientific, Boston, MA). The majority of the patients had one stent placed. In 10 patients two stents were required.
Clinical characteristics of the patients
The clinical characteristics of the 100 patients included in the study are summarized in Tables 1 and 2. The mean age of the 100 patients was 77 years; 62 were men and 38 were women. The cancer was located in the rectum in 55 patients and in the sigmoid colon in 45 (in 7 of these 45 patients the tumor was located just at the junction between sigmoid colon and descending colon). Symptoms of obstruction were present in all patients. Ten patients had a previous admission to the hospital with an acute obstruction that had resolved spontaneously. All patients were admitted in a condition of fluid and electrolyte imbalance. A previous CT scan showed distant metastases and/or ascites and peritoneal implants in all patients.
Review of the literature
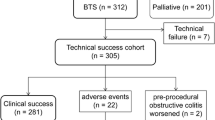
A systematic search in the literature (Pub Med) was done to December 2011. The search included the terms “endoscopic stenting for colorectal cancer,” “colorectal cancer obstruction,” “palliative management of colorectal cancer.” The search aimed to review the mortality and morbidity rates after endoscopic stenting in patients with obstructing colorectal cancer. One particular goal was to determine whether the results of the procedure had improved after the initial experiences. For these reasons recent articles were compared to the systematic review published by Watt et al. in 2007 [3], which included 1,785 patients collected from 88 reports. In our review, 26 articles published from April 2007 to December 2011 were analyzed.
Inclusion criteria
No language restriction was applied. For publications by the same authors, only the more recent article with the largest number of cases was included. Articles were selected if they presented sufficient data concerning mortality and complications. Ten articles were not included because data were incomplete or because results for fewer than 8 patients were reported. Overall 2,209 patients were included in our review (Table 3), and their clinical outcome was compared to the 1,785 patients reported by Watt et al. [3]. There were 8 prospective studies and 18 retrospective reviews of clinical series. The aim of our analysis was to determine (1) factors affecting results of SEMS placement and (2) any improvement in results in comparison to the previous meta-analysis.
Data extraction
Data were extracted using standardized tables developed a priori. Because of the significant heterogeneity, data were presented grouped and split according to possible variables. The variables analyzed, when possible, were clinical indication for the procedure (acute versus chronic obstruction), clinical conditions in which the procedure was performed (emergency or elective conditions), and clinical and anatomic variables.
Statistical analysis
Both paired and unpaired Student’s t-tests and Fisher’s exact test were used where appropriate. Differences were considered significant at a p value of < 0.05.
Results
Personal experience
Early results
There were no deaths in our series. The technical success rate was 96 %. In 4 patients the procedure was not possible because of sharp angulation of the obstruction. In another 4 patients, despite the technical success, symptoms of obstruction persisted: all 4 of the patients had ascites and peritoneal carcinosis. Overall clinical success was achieved in 92 % of the patients (92/100).
Technical failures were more common in patients with cancer of the sigmoid colon, or with complete obstruction, but these differences were not statistically significant. There was no technical failure (0/14) with the pediatric nasogastroscope to pass the obstruction, in comparison with 4 failures (4/86) with the standard technique (p = NS). In the postoperative period there were three cases of minor bleeding treated conservatively.
Late results
During the follow-up period there were 4 cases of stent dislodgement (4 %). All 4 patients had a new stent inserted with long-term success. More than 50 % of the patients had chemotherapy and no case of perforation was noted. The two most common complications were fecal impaction (19 %) resolved with a repeat colonoscopy in all cases, and tumor ingrowth within the stent (8 %), which was resolved with placement of a new stent.
Review of the literature
Early results
In our review, mortality after SEMS placement ranged from 0 % to 10 %, with a mean of 1.2 % (Tables 3 and 4). This was statistically lower than that reported in the meta-analysis of Watt et al. [3] (p < 0.05). Mortality was higher when the procedure was performed under “emergency” conditions (0.3 % versus 4.2 %; p < 0.05). However, this difference was not evident when the procedure was performed under elective or “semi-elective” conditions in patients with admission to the hospital for acute obstruction versus patients with chronic obstruction. In our review the most detailed complication reported was colorectal perforation, which ranged from 0 % to 13 % (mean: 3 %). Even in this case, the complication was more common in patients who had the procedure performed in an emergency situation. The risk of perforation is lower than that reported in the meta-analysis of Watt et al. [3] (p < 0.05). Technical success ranged from 92 % to 100 % (mean: 97 %) and again it was higher when the procedure was performed under elective conditions. Technical success and clinical success rates were higher than those reported in the 1,785 cases collected by Watt et al. [3] (p < 0.05).
Late results
Covered or uncovered stents seem to have similar results, with a higher incidence of tumor ingrowth in patients who had uncovered stents and a higher possibility of dislodgment in patients who had a covered stent [7]. Complete information about the increased risk of perforation in patients who had a SEMS and chemotherapy was not available. Two reports [8, 9] demonstrated an increased risk of perforation at the site of the stent in patients who had chemotherapy, and two other studies did not show any increased risk [7, 10]. Because data were incomplete, it was not possible to explore the possibility that this risk was associated with a particular chemotherapeutic agent. In our review three prospective studies [4, 11, 12] and one retrospective study [13] analyzed the late results in patients with stage IV obstructing colorectal cancer who underwent SEMS placement versus diverting colostomy. Three showed overall satisfactory results in patients with SEMS placement. One study [12] showed the poorest results in patients who had endoscopic stenting for the high incidence of late colonic perforation (6/11 = 55 %)..
Discussion
Self-expandable metallic stent placement in patients with stage IV not resectable obstructing colorectal cancer offers many advantages over diverting colostomy. The procedure can be performed under light sedation, the hospital stay is short, and colostomy is avoided, which can represent a significant burden in the relationship between the patient and the surrounding world in his/her last period of life.
In our 12-year experience, results have been satisfactory, with no operative mortality and no major complications. Technical success is achievable in the majority of patients, with early canalization and short hospital stay (in our experience mean postoperative hospital stay was 2 or 3 days). The one problem that prohibits SEMS placement is the presence of sharp angulation of the obstruction, with difficulty in passing the guidewire. To overcome this limitation, we recently adopted the technique of using a pediatric nasogastroscope (4.8 mm), to pass the obstruction in such a way that the guidewire can go through the obstruction not blindly, but under direct vision. This technique also provides the theoretical possibility of avoiding bowel perforation above the level of the obstruction, where the wall of the colon is dilated and thin. Perforation in this situation is commonly caused by blind passage of the guidewire around the distorted anatomy. In all cases in which we have used the nasogastroscope under direct vision, the SEMS was placed more easily and without complications.
In our review of the literature, results seem improved in comparison to the earlier experience reported by Watt et al. [3]. This could reflect many factors, including increased experience (we compared 2,209 patients from 26 reports to 1,785 patients from 88 reports), better patient selection, increased technology in SEMS placement, and, almost certainly, a significant preference for performing the procedure under elective or semi-elective conditions. In our review the percentage of procedures performed under emergency conditions was much lower than that reported by Watt et al. [3]. The advantage of performing SEMS placement as an elective procedure has been confirmed in our analysis, where outcome was better than when the procedure was performed as an emergency. In a patient who comes to the emergency department with acute obstruction and with a diagnosis of colorectal cancer obstruction (easily made today with CT scan), unless there is evidence of perforation, SEMS placement can be deferred until the general status of the patient is equilibrated with a proper therapy, and the procedure can be performed in elective/semi-elective conditions, by an experienced endoscopist, with good assistance, in the right environment.
Endoscopic stenting can also be offered as a bridge to resection in patients with acute obstruction. A recently published randomized trial [9] has shown poor results with emergency endoscopic stenting as a bridge to elective surgery versus immediate emergency surgery. These findings testify to the fact that endoscopic stenting performed under emergency conditions is a challenging procedure and every effort should be made to place the SEMS in elective-semi-elective conditions, even in patients with an acute obstruction.
It is evident that in patients with SEMS careful follow-up is required. In our experience a repeat colonoscopy because of symptoms of recurrent obstruction was needed in about 31 % of the patients during their reduced life expectancy. In the majority of the cases the obstruction was secondary to fecal impaction or tumor ingrowth within the stent. Both these complications can be treated in an outpatient basis with colonoscopy. In selected cases placement of a new stent is required.
In our opinion a patient with stage IV not resectable colorectal cancer who cannot be carefully followed is much better off with a diverting colostomy. At the same time, the need for such a careful follow-up can reduce the difference in costs between the two forms of palliative treatment in these patients.
In our series no patient had bowel perforation at the site of the stent, and more than 50 % of the patients received chemotherapy. We did not analyze in detail the chemotherapeutic agents given to our patients by our oncologist colleagues. Two recent multicenter studies [8, 12] have shown increased occurrence of perforation at the stent site in patients who had also chemotherapy, a matter that raises concerns about this form of treatment in this setting. However, other reports have not confirmed this finding [10], even if the chemotherapeutic regimens administered are not always described.
In conclusion, SEMS placement offers a valid alternative to diverting colostomy as a form of palliative therapy in patients with obstructing stage IV colorectal cancer. However, a respectful and wise attitude toward this form of therapy is required, including proper selection of the patients, experienced operators, and careful follow-up.
References
Dohmoto M (1991) New method; endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Digest 3:1507–1512
Tejero E, Mainar A, Fernandez L et al (1994) New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum 37:1558–1559
Watt AM, Faragher IG, Griffin TT et al (2007) Self-expanding metal stents for relieving malignant colorectal obstruction; a systematic review. Ann Surg 246:24–30
Nagula S, Ishill N, Nash C et al (2010) Quality of life and symptoms control after stent placement or surgical palliation of malignant colorectal obstructions. J Am Coll Surg 210:45–53
Baron TH (2010) Colonic stenting: a palliative measure only or a bridge to surgery? Endoscopy 42:163–168
Lee JH, Ross WA, Davila R (2010) Self-expandable metal stents (SEMS) can serve as a bridge to surgery or as a definitive therapy in patients with an advanced stage of cancer: clinical experience of a tertiary cancer center. Dig Dis Sci 55:3530–3536
Park JK, Lee MS, Ko BM et al (2011) Outcome of palliative self-expanding metal stent placement in malignant colorectal obstruction according to the stent type and manufacturer. Surg Endosc 25:1293–1299
Manes G, de Bellis M, Fuccio L et al (2011) Endoscopic palliation in patients with incurabile malignant obstruction by means of self-expanding metal stents; analysis of results and predictors of outcomes in a large multicenter series. Arch Surg 146:1157–1162
Van Hooft JE, Bemelman WA, Oldenburg B et al (2011) Colonic stenting versus emergency surgery for acute left sided malignant colonic obstruction: a multicentre randomized trial. Lancet Oncol 12:344–352
Bielawska B, Hookey LC, Jalink D (2010) Large-diameter self expanding metal stents appear to be safe and effective for malignant colonic obstruction with and without concurrent use of chemotherapy. Surg Endosc 24:2814–2821
Fiori E, Lamazza A, Schillaci A et al (2012) Palliative management for patients with subacute obstruction and stage IV unresectable rectosigmoid cancer: colostomy versus endoscopic stenting: final results of a prospective randomized trial. Am J Surg 204:321–326
Van Hooft JE, Fockens P, Marinelli AW et al (2008) Early closure of a multicenter clinical trial of endoscopic stenting versus surgery for stage IV left sided colorectal cancer. Endoscopy 40:184–191
Lee HJ, Hong SP, Cheon JH et al (2011) Long-term outcome of palliative therapy for malignant colorectal obstruction in patients with unresectable metastatic colorectal cancers; endoscopic stenting versus surgery. Gastrointest Endosc 73:535–542
Song HY, Kim JH, Shin JH et al (2007) A dual-design expandable colorectal stent for malignant colorectal obstruction: results of a multicenter study. Endoscopy 39:448–454
Repici A, Fregonese D, Costamagna G et al (2007) Ultraflex precision colonic stent placement for palliation of malignant colonic obstruction: a prospective multicenter study. Gastrointest Endosc 66:920–927
Fregonese D, Naspetti R, Ferrer S et al (2008) Ultraflex precision colonic stent placement as a bridge to surgery in patients with colonic malignant obstruction. Gastrointest Endosc 67:68–73
Alcantara M, Serra X, Bombardò J (2007) Colorectal stenting as an effective therapy for preoperative and palliative treatment of large bowel obstruction: 9 year experience. Tech Coloproctol 11:316–322
Shrivastava V, Tariq O, Tiam R et al (2008) Palliation of obstructing malignant colonic lesions using self expanding metal stents: a single-center experience. Cardiovasc Interv Radiol 31:931–936
Im JP, Kim SG, Kang HW et al (2008) Clinical outcomes and patency of self-expanding metal stents in patients with malignant colorectal obstruction: a prospective single center study. Int J Colorect Dis 23:789–794
Kim H, Kim SH, Choi SY et al (2008) Fluoroscopically guided placement of self expandable metallic stents and stent grafts in the treatment of malignant colorectal obstruction. J Vasc Interv Radiol 19:1709–1716
Keswani RN, Azar RR, Edmundowicz SA et al (2009) Stenting for malignant colonic obstruction: a comparison of efficacy and complications for colonic versus extracolonic malignancy. Gastrointest Endosc 69:675–680
Jung MK, Park SY, Jeon SW et al (2010) Factors associated with the long term outcome of a self-expandable colon stent used for palliation of malignant colorectal obstruction. Surg Endosc 24:525–530
Vemulapalli R, Lara LF, Sreenarasinhaiah J et al (2010) A comparison of palliative stenting or emergent surgery for obstructing incurable colon cancer. Dig Dis Sci 55:1732–1737
Al Samaaree A, Fasih T, Hayat M (2010) Use of self-expandable stent for obstructive distal and proximal large bowel: a retrospective study in a single center. J Gastrointest Cancer 41:43–46
Small AJ, Coelho-Prabhu N, Baron TH (2010) Endoscopic placement of self expandable metal stents for malignant colonic obstruction: long-term outcome and complication factors. Gastrointest Endosc 71:560–572
Donnellan F, Cullen G, Cagney D (2010) Efficacy and safety of colonic stenting for malignant diseasse in the elderly. Int J Colorectal Dis 25:747–750
Branger F, Thibadeau E, Mucci-Hennekinne S et al (2010) Management of acute malignant large-bowel obstruction with self-expanding metal stents. Int J Colorectal Dis 25:1481–1485
Luigiano C, Ferrara F, Fabbri C et al (2011) Through-the-scope large-diameter self-expanding metal stent placement as a safe and effective technique for palliation of malignant colorectal obstruction: a single centre experience with long term follow-up. Scand J Gastroenterol 46:591–596
Arya N, Blair N, Arya P (2011) Community experience of colonic stenting in patients with acute large bowel obstruction. Can J Surg 54:282–285
DeGregorio MA, Laborda A, Tejero E et al (2011) Ten year retrospective study of treatment of malignant colonic obstructions with self expandable stents. J Vasc Intrervent Radiol 22:870–878
Saida Y, Enomoto T, Takabayashi K et al (2011) Outcome of 141 patients of self-expandable metallic stent placements for malignant and benign colorectal strictures in a single center. Surg Endosc 25:1748–1752
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lamazza, A., Fiori, E., Schillaci, A. et al. Self-expandable Metallic Stents in Patients with Stage IV Obstructing Colorectal Cancer. World J Surg 36, 2931–2936 (2012). https://doi.org/10.1007/s00268-012-1767-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1767-x