Abstract
Background
Metachronous autotransplantation of cryopreserved parathyroid tissue is a technique for treating postoperative hypoparathyroidism after parathyroid surgery for renal hyperparathyroidism (rHPT). The aim of the present study was to evaluate our institution’s experience with metachronous autotransplantation to analyze the role of cryopreservation in the treatment of rHPT and to determine for whom and when cryopreservation of parathyroid tissue should be deemed necessary.
Methods
A prospective database of patients with rHPT who underwent surgery between 1976 and 2011 was screened for patients with hypoparathyroidism who received a metachronous autotransplantation. Data were analyzed regarding clinical data, histopathological findings of the cryopreserved parathyroid tissues, and patient outcome after metachronous replantation of parathyroid tissue.
Results
Fifteen of 883 patients with rHPT underwent a metachronous autotransplantation under local anesthesia at a mean time of 23 months following the last cervical surgery. Histopathology of the parathyroid tissue chosen for transplantation revealed a necrosis rate of 0 % in 14 and 70 % in one patient. Mean preoperative serum calcium and parathyroid hormone (PTH) levels were 2.0 mmol/l and 3.7 pg/ml, respectively. Autotransplantation raised mean serum calcium and PTH levels to 2.2 mmol/l and 97.5 pg/ml, respectively, after a mean follow-up of 78 months.
Conclusions
Metachronous autotransplantation following parathyroid surgery in patients with rHPT effectively normalizes PTH and calcium levels. The success rate is high if an adequate cryopreservation procedure is applied. However, it is rarely necessary, and therefore the cryopreservation of parathyroid tissue in all patients has to be questioned, at least from an economic point of view.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subtotal parathyroidectomy (SPTX) and total parathyroidectomy with autotransplantation of fresh parathyroid tissue (TPTX + AT), each combined with a bilateral cervical thymectomy, are established surgical procedures in patients with otherwise uncontrollable renal hyperparathyroidism (rHPT) [1]. Total parathyroidectomy with autotransplantation of fresh parathyroid tissue reduces the risk of persistent or recurrent cervical hyperparathyroidism as compared to SPTX [2]. Postoperative hypoparathyroidism may result from a non-functioning remnant within the neck following SPTX or after failed engraftment of transplanted parathyroid fragments [3]. Levels of calcium and parathyroid hormone (PTH) in the immediate postoperative setting (1–3 days after surgery) are informative about the function of the parathyroid remnant within the neck [4, 5]. Parathyroid fragments at the site of the autograft may require up to 6 months to resume adequate function [4–6].
Permanent hypoparathyroidism is defined as persistent hypocalcemia requiring calcium and vitamin D supplementation more than 6 months after parathyroid surgery [6], and it is a feared complication of both thyroid and parathyroid surgery. Although the risk of permanent hypoparathyroidism is typically about 1 % after initial parathyroid surgery [7], it is as high as 30 % after reoperative interventions for recurrent or persistent hyperparathyroidism [8]. Persistent hypoparathyroidism leads to a reduced quality of life with lifelong medical supplementation, frequent laboratory testing, and the potential for repeated hospital admissions [9]. Moreover, in patients on permanent hemodialysis, decreased PTH levels are associated with a suppression of bone turnover that may provoke the development of adynamic bone disease [10]. To hinder the development of the latter, PTH levels ranging from 150–300 pg/ml have been recommended for patients with stage 5 chronic kidney disease within actual guidelines [11]. If available, hypoparathyroidism persisting for more than 6 months after parathyroid surgery should be treated by autotransplantation of autologous cryopreserved parathyroid tissue [12].
The history of parathyroid autotransplantation started in 1909 with Halsted’s [13] first transplant in dogs, and it continued with Lahey and Clute’s [14] first successful human autotransplantation. Wells and co-workers [5, 15–18] were the first to show that cryopreserved parathyroid tissue can be thawed and grafted. Metachronous autotransplantation of cryopreserved parathyroid tissue is now an established method for treating permanent hypoparathyroidism after parathyroid surgery [12]. Parathyroid autografts can be heterotopically transplanted in the sternocleidomastoid muscle, the muscle of the forearm, or the thigh, as well as in the subcutaneous tissue of the anterior chest or abdominal wall. Autotransplantation can be performed at the time of parathyroid surgery (synchronous) or at a later date (metachronous) in the case of hypofunctional residual parathyroid tissue in the neck or at the site of a parathyroid autograft [19].
Metachronous autotransplantation has been associated with decreased success rates when compared to synchronous autotransplantation [4, 8, 12, 20–23]. Functionality rates of synchronous autotransplantation have been reported to exceed 80 %, whereas functionality ranges from 17 to 83 % in the case of metachronous autotransplantation of cryopreserved parathyroid tissue [4, 8, 12, 20–23]. However, the success rates of metachronous autotransplantation seem to be dependent on the cryopreservation process, the autotransplantation technique (e.g., amount and size of parathyroid fragments transplanted), and the time between freezing and thawing [4, 8, 12, 20–23].
The aim of the present study was to evaluate our institution’s experience with metachronous autotransplantation to analyze the role of cryopreservation in the treatment of rHPT and to determine for whom and when cryopreservation of parathyroid tissue is necessary.
Material and methods
A prospective database of patients who underwent parathyroid surgery for rHPT between 1976 and 2011 was screened for those who underwent a metachronous autotransplantation of cryopreserved parathyroid tissue. Indications for a metachronous autotransplantation were permanent hypoparathyroidism with non-measurable PTH or PTH below the lower normal limit of the assay applied accompanied by hypocalcemia despite daily calcium and vitamin D supplementation. Data were analyzed regarding age, gender, clinical presentation ahead of parathyroid replantation, previous surgical procedures, mean time between last cervical surgery and replantation, pathology of cryopreserved tissue, pre- and postoperative total serum calcium and PTH levels, as well as outcome after replantation.
The process to cryopreserve parathyroid tissue at our institution is standardized. Tissue removed fresh at the time of operation was stored in cold sterile 0.9 % saline solution at +4 °C. After verification of the parathyroid origin of a part of each gland by frozen section, the remaining tissue was immediately transferred in 0.9 % sterile cold saline solution to the research laboratory. Under sterile conditions, the tissue was divided into fragments of 1 mm³. Tissue was then placed in a cryoprotective sterile culture medium containing Roswell Park Memorial Institute 1640 solution (RPMI 1640), dimethyl sulfoxide solution (DMSO), and autologous serum at a temperature of +4 °C. At this point, 40–60 particles were placed into vials and frozen with a programmed freezer that cools the temperature at a speed of 1 °C/min until −80 °C was achieved. The tissue was stored therein for 4–24 h and then transferred to liquid nitrogen for long-term storage at −196 °C.
Prior to metachronous autotransplantation, viability was estimated by determining the ratio of viable and necrotic cells in a sample of the tissue within the vial of parathyroid tissue intended for replantation. Several pieces of frozen parathyroid tissue from the vial intended for replantation were, thawed and sent to the Pathology Department. An additional microbiological culture of another part of this tissue was tested to exclude bacterial contamination.
When the necrosis rate was found to be below 50 % and microbiological examination revealed no evidence of contamination, the remaining parathyroid tissue from the vial was thawed in a 37 °C water bath and the tissue then was washed five times with 80 % RPMI 1640 and 20 % fresh autologous serum and preserved on ice. In the operating room, parathyroid tissue was separated into 30 pieces measuring 1 mm³ each (Fig. 1). A longitudinal incision was made above the brachioradial muscle of the nondominant and non-shunt-bearing forearm. Parathyroid fragments were then placed into pockets in the brachioradial muscle, each closed separately with clips (Fig. 2).
Clinical assessment of graft function after metachronous autotransplantation comprised repeated measurements of total serum calcium and PTH in an outpatient setting to evaluate the necessity of additional calcium and vitamin D supplementation, and to identify symptoms of hypocalcemia such as tingling, numbness, and spasms or diarrhea caused by high calcium supplementation.
Since 1999, intact PTH has been measured with a commercially available immunoluminescence assay with a normal range of 11–65 ng/ml. Total serum calcium was measured with a normal range of 2.2–2.7 mmol/l. Parathyroid hormone and calcium were measured one day before and 4 weeks after metachronous autotransplantation. Follow-up data were acquired by the attending nephrologist.
Cryopreservation has been performed on all patients undergoing PTX for rHPT in our department since 1987. To evaluate the influence of the duration between freezing and thawing on the rate of necrosis in tissue used for metachronous autotransplantation, we randomly selected five patients who underwent surgery in 1990, 1995, 2000, 2005, and 2010 and assessed the ratio of viable and necrotic cells in each of these patients.
Cryopreservation is performed at our institution’s research lab. No extra costs resulted for the patients as the cryopreservation process is integrated as a part of the research working schedule. However, to estimate the costs associated with cryopreservation, we calculated the costs for vials, reagents, and liquid nitrogen, as well as the salary, prior to taxes, for the laboratory assistant to prepare, freeze, and thaw parathyroid tissue in one and a half hours.
Furthermore, companies offering professional cryopreservation in Germany were asked to give a quote for the cryopreservation and storage of parathyroid tissue over a period of 5 years.
Data were analyzed using SPSS software (Statistical Product and Services Solutions, version 16.0, SPSS Inc, Chicago, IL). All results were expressed as means ± standard error of the mean and percentages. Fisher’s exact test was used to determine statistically significant differences among the groups; p ≤ 0.05 was considered statistically significant.
Results
Of the 883 parathyroid surgeries for rHPT, 673 were initial interventions. Of these, 550 surgeries were accompanied by a simultaneous parathyroid autotransplantation. In the remaining 123 patients no simultaneous autotransplantation was performed at the time of initial PTX for the following reasons: patients with a supposed three gland resection with a later detection of the fourth gland within the resected thymus, a 3.5 gland resection (SPTX) or patient participation in the pre-TOPAR or TOPAR PILOT trial (prospective randomized comparison of TPTX + AT with TPTX without AT) [24], and randomization in the group receiving TPTX without autotransplantation (Fig. 3).
Of 883 parathyroid surgeries, 210 were reoperations for recurrent or persistent rHPT or for persistent hypoparathyroidism. Of these, 121 patients (57.6 %) underwent a re-exploration of the neck, and 89 (42.4 %) underwent reoperative surgery on the side of the autograft. Seventy-four of the latter 89 patients (83.1 %) received a reduction of a parathyroid autograft for recurrent or persistent rHPT, and 15 (16.9 %) suffered from persistent hypoparathyroidism and underwent a metachronous autotransplantation of cryopreserved parathyroid tissue. The 15 patients who underwent a metachronous autotransplantation were further analyzed.
Seven patients (7/15; 46.7 %) were women and eight (8/15; 53.3 %) were men, with a mean age of 46.1 ± 4.2 years. Two patients (13.3 %) were predialytic and one patient (6.7 %) had a functioning kidney graft. Nine of 15 patients had a preoperative supplementation with vitamin D and calcium, two patients received calcium only, and another patient received vitamin D only. Three patients had an inconsistent vitamin D and calcium supplementation due to poor compliance of the patients themselves.
Eleven of 15 patients (73.3 %) underwent a metachronous autotransplantation after initial surgery. Five of these 11 patients had a simultaneous but later nonfunctional autotransplantation within the initial surgery. The remaining patients had undergone a TPTX without autotransplantation (n = 1) or a suspected incomplete resection with fewer than four glands identified (n = 5).
Four of 15 patients (26.7 %) underwent a metachronous autotransplantation after reoperations for recurrent or persistent rHPT within the neck. Two of these patients had a TPTX + AT as initial surgery and a cervical reoperation for removal of supernumerary parathyroid glands. The nonfunctioning of the autograft in these patients may be attributed to suppression of the grafted tissue by persistent rHPT. In the remaining two patients had incomplete resections, with only one or two glands initially resected. Both patients had undergone initial surgery for suspected primary hyperparathyroidism with mild chronic kidney disease (stages 3 at the time of initial surgery). With a progression of kidney failure, HPT recurred, and these patients developed hypoparathyroidism after repeated surgery with removal of the remaining glands prior to replantation.
The history of previous surgeries in our patients who required a metachronous parathyroid autotransplantation is displayed in Figure 3. The mean time between last cervical surgery and metachronous autotransplantation was 23.3 ± 6.8 months (range 1–86 months). In four patients replantation was performed more than two years after the last neck surgery. Four weeks after replantation, mean calcium increased from 2.0 ± 0.07 to 2.1 ± 0.2 mmol/l. The serum PTH level increased from 3.7 ± 1.3 to 39.7 ± 11.5 pg/ml. After a mean follow-up of 78.1 ± 30.6 months, mean calcium measured 2.2 ± 0.2 mmol/l and PTH was 97.5 ± 14.5 pg/ml. Flow of PTH and calcium levels are delineated within Figs. 4 and 5. None of the 15 patients required reoperation for either hyper- or hypoparathyroidism thereafter.
Pathologic evaluation of the sample probes revealed a necrosis rate of 0 % in all samples from 1990, 2000, 2005, and 2010. In one of five samples dating back to the year 1995 only, a necrosis rate of 70 % was determined (Fig. 6), whereas in the other four samples from that year no necrotic cells were detected. It is surprising that such a high necrosis rate (70 %) was found in this one patient. A closer look into the chart revealed no specific co-morbidities or any complications with storage. Also no perioperative alterations were recorded.
An estimation of institutional costs for parathyroid cryopreservation is displayed in Table 1. The quotes for the cryopreservation and storage over 5 years obtained from a company offering industrial parathyroid cryopreservation in Germany were €892.50 for the first year and €249.90 for each succeeding year for one patient.
Discussion
Synchronous and metachronous autotransplantations of parathyroid tissue are well-established procedures. A replantation of autologous cryopreserved parathyroid tissue is indicated to avoid long-term supplementation of calcium and/or vitamin D in case of persistent hypoparathyroidism [12]. The necessity for metachronous autotransplantations is extremely rare. After TPTX + AT for rHPT, postoperative hypocalcemia due to inadequate functionality of the autograft is reported to occur in up to 4 % of cases [25]. However, in our collective only 7/550 patients (1.3 %) required a replantation due to a nonfunctioning autograft. In five of them, nonfunctionality of the tissue occurred without a detectable reason for the failed engraftment. In two patients, the nonfunctionality may be attributed to suppression of the grafted tissue due to persistent rHPT caused by a supernumerary cervical parathyroid gland.
Although the success rates of metachronous parathyroid autotransplantations are reported to be lower than those of synchronous autotransplantations [4, 8, 12, 20–23], all of our metachronous grafts were functional. In several other published studies, the rate of fully functional metachronous autografts varied between 8 and 83 % [4, 8, 19, 21, 23]. The high success rate in our study may be explained by the microbiological and histological examinations prior to replantation, as only tissues without necroses or microbiological contamination were used for replantation. Another reason may be the standardized freezing and thawing protocol applied in our department. There was no necessity for prolonged transportation with unstable temperatures because the laboratory is located close to the operating suite. As a result, the time between resection and freezing was always shorter than 1 h.
The success of metachronous autotransplantation is also related to the number of replanted fragments [26]. In case of a synchronous or metachronous autotransplantation with a preoperative determination of a necrosis rate of 0 %, implantation of 20 pieces of 1 mm³ is reported to be sufficient; if the histological examination is abdicated, implantation of 30–40 pieces is recommended [26]. Reasons for failed parathyroid engraftment may be lack of angiogenesis and vascularization of transplanted tissue, as well as a disturbed transport and delivery of autocrine and paracrine hormonal factors influencing the response of transplanted parathyroid cells to calcium levels. However, our findings are in concordance with the findings of others who described the functionality of cryopreserved cells to be similar to that of fresh tissue [12, 27, 28].
The mean time of cryopreservation in our study was 23.3 months, at most 86 months. In other studies the viability of cryopreserved cells was analyzed after 3, 6, and 26 months after cryopreservation. Several in vitro and in vivo studies have shown that very few parathyroid tissue samples are potentially functional after two years of cryopreservation [19, 29]. Because of extremely low success rates in establishing a cell culture of parathyroid cells, we did not explicitly examine the cell viability. Nevertheless our results demonstrate the cell viability to be good enough to compensate for hypoparathyroidism. Unfortunately, no data exist about functionality and viability of cryopreserved parathyroid tissue after more than 26 months of freezing. However, the exemplary assessment of the necrosis rate in samples 5, 10, 15, and 20 years after initial parathyroid surgery and cryopreservation demonstrated no necrosis in almost all tissues examined.
The most appropriate time for replantation is difficult to define. Criteria should be assessed based on the degree of patient’s symptoms, on the necessity for calcium and vitamin D supplementation, and on the presence of an adynamic bone disease detected within bone histology. However, one always has to consider that the cryopreserved parathyroid tissue to be grafted is activated and proliferated, and it is therefore a potential reason for recurrent disease after replantation. A persistent failure to measure PTH accompanied by the necessity for constant calcium and vitamin D supplementation to maintain normocalcemia 6 months after parathyroid surgery are considered indications for replantation [12]. However, prolonged hypocalcemia is well known, especially in patients with a distinct renal osteopathy due to the immense “bone hunger” post-parathyroidectomy [30]. The long range of up to 86 months in our patients demonstrates that hypoparathyroidism may become evident even a long time after surgery. It may result from a disturbed perfusion of the transplanted parathyroid tissue due to surgery at the grafted arm (e.g., after establishing a new arteriovenous fistula), a delayed referral through the attending nephrologists, or the preference of patients to wait for delayed graft functionality.
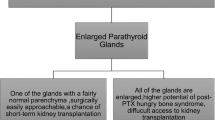
Cryopreservation and storage of parathyroid tissues are costly, and these costs are not covered by health insurance in Germany. Furthermore, cryopreservation requires a complex infrastructure to maintain a good quality of tissue preservation. Our data underline a very low risk of 1.3 % of developing persistent hypocalcemia after initial surgery with simultaneous autotransplantation. The risk seems to be highest among patients with suspected incomplete resections and in those who undergo cervical reoperations or total parathyroidectomy without simultaneous autotransplantation. At least in the latter scenarios, cryopreservation of parathyroid tissue seems to be indispensable. From an economic point of view, the necessity to cryopreserve parathyroid tissue in all patients undergoing parathyroidectomy for rHPT seems to be questionable.
Nevertheless, one has to consider that persistent hypoparathyroidism can be life-threatening and, without having cryopreserved parathyroid tissue “up one’s sleeve,” it is difficult to treat. The only substitute parathyroid hormone available so far (Teriparatide) needs to be applied subcutaneously and is accredited only for osteoporosis [31, 32]. If nasally applicable PTH [33, 34] were available, it would alter the necessity to cryopreserve at all, and may have an influence on the autotransplantation process as well.
Conclusions
Because of the lack of reliable factors in predicting postoperative hypoparathyroidism, cryopreservation of parathyroid tissue would be desirable in any patient undergoing parathyroid surgery. In view of institutional costs and economic concerns, cryopreservation for all patients may not be realistic; it should, however, be performed at least in patients with suspected incomplete resections, patients undergoing reoperation, and patients who receive a total parathyroidectomy without autotransplantation.
The benefit for patients with permanent postoperative hypoparathyroidism mainly consists of avoidance of lifelong supplemental treatment and, possibly, prevention of adynamic bone disease. Good techniques of freezing and thawing as well as an elaborated preoperative analysis and selection of the tissue are essential for successful replantation. The functionality and viability of parathyroid tissue after more than two years of cryopreservation has to be evaluated in further cellular studies.
References
Shih ML, Duh QY, Hsieh CB et al (2009) Total parathyroidectomy without autotransplantation for secondary hyperparathyroidism. World J Surg 33:248–254. doi:10.1007/s00268-008-9765-8
Rothmund M, Wagner PK, Schark C (1991) Subtotal parathyroidectomy versus total parathyroidectomy and autotransplantation in secondary hyperparathyroidism: a randomized trial. World J Surg 15:745–750. doi:10.1007/BF01665309
Borot S, Lapierre V, Carnaille B et al (2010) Results of cryopreserved parathyroid autografts: a retrospective multicenter study. Surgery 147:529–535
Wells SA Jr, Farndon JR, Dale JK et al (1980) Long-term evaluation of patients with primary parathyroid hyperplasia managed by total parathyroidectomy and heterotopic autotransplantation. Ann Surg 192:451–458
Wells SA Jr, Gunnells JC, Gutman RA et al (1977) The successful transplantation of frozen parathyroid tissue in man. Surgery 81:86–90
Shoback D (2008) Clinical practice. Hypoparathyroidism. N Engl J Med 359:391–403
Udelsman R (2002) Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg 235:665–670
Herrera M, Grant C, van Heerden JA et al (1992) Parathyroid autotransplantation. Arch Surg 127:825–829
Guerrero MA (2010) Cryopreservation of parathyroid glands. Int J Endocrinol, article 829540. doi:10.1155/2010/829540
Andress DL (2008) Adynamic bone in patients with chronic kidney disease. Kidney Int 73:1345–1354
National Kidney Foundation (2003) K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42(4 Suppl 3):S1–S201
Rothmund M, Wagner PK (1984) Assessment of parathyroid graft function after autotransplantation of fresh and cryopreserved tissue. World J Surg 8:527–533. doi:10.1007/BF01654930
Halsted WS (1909) Auto- and isotransplantation, in dogs, of the parathyroid glandules. J Exp Med 11:175–199
Lahey FH, Clute HM (1926) Persistent and recurrent hyperparathyroidism. Ann Surg 83:199–205
Wells SA Jr, Gunnells JC, Shelburne JD et al (1975) Transplantation of the parathyroid glands in man: clinical indications and results. Surgery 78:34–44
Wells SA Jr, Gunnells JC, Gutman RA et al (1977) The successful transplantation of frozen parathyroid tissue in man. Surgery 81:86–90
Wells SA Jr, Stirman JA Jr, Bolman RM III (1977) Thyroid transplantation. World J Surg 1:747–756. doi:10.1007/BF01555931
Wells SA Jr, Gunnells JC, Leslie JB et al (1977) Transplantation of the parathyroid glands in man. Transplant Proc 9:241–243
Cohen MS, Dilley WG, Wells SA Jr et al (2005) Long-term functionality of cryopreserved parathyroid autografts: a 13-year prospective analysis. Surgery 138:1033–1040
Saxe A (1984) Parathyroid transplantation: a review. Surgery 95:507–526
Feldman AL, Sharaf RN, Skarulis MC et al (1999) Results of heterotopic parathyroid autotransplantation: a 13-year experience. Surgery 126:1042–1048
Edis AJ, Linos DA, Kao PC (1980) Parathyroid autotransplantation at the time of reoperation for persistent hyperparathyroidism. Surgery 88:588–593
Saxe AW, Spiegel AM, Marx SJ et al (1982) Deferred parathyroid autografts with cryopreserved tissue after reoperative parathyroid surgery. Arch Surg 117:538–543
Schlosser K, Veit JA, Witte S et al (2007) Comparison of total parathyroidectomy without autotransplantation and without thymectomy versus total parathyroidectomy with autotransplantation and with thymectomy for secondary hyperparathyroidism: TOPAR PILOT-trial. Trials 8:22
Rothmund M, Wagner PK (1983) Total parathyroidectomy and autotransplantation of parathyroid tissue for renal hyperparathyroidism. A one- to six-year follow-up. Ann Surg 197:7–16
Wagner PK, Rothmund M (1987) Replantation of autologous cryopreserved parathyroid tissue in permanent postoperative hypoparathyroidism. Dtsch Med Wochenschr 112:1160–1162
Herrera MF, Grant CS, van Heerden JA et al (1992) The effect of cryopreservation on cell viability and hormone secretion in human parathyroid tissue. Surgery 112:1096–1101
Wagner PK, Rumpelt HJ, Krause U et al (1986) The effect of cryopreservation on hormone secretion in vitro and morphology of human parathyroid tissue. Surgery 99:257–264
Guerrero MA, Evans DB, Lee JE et al (2008) Viability of cryopreserved parathyroid tissue: when is continued storage versus disposal indicated? World J Surg 32:836–839. doi:10.1007/s00268-007-9437-0
Wagner PK, Rothmund M (1990) Long-term results after implantation of autologous cryopreserved parathyroid tissue. Dtsch Med Wochenschr 115:1863–1867
Sowa H, Hamaya E, Yamamoto T (2011) Teriparatide: human recombinant parathyroid hormone (1–34) as a daily subcutaneous injection. Clin Calcium 21:9–16
Ishizuya T (2011) Therapeutic agents for disorders of bone and calcium metabolism: weekly subcutaneous injection of teriparatide. Clin Calcium 21:17–24
Sato K (2007) Therapeutic agents for disorders of bone and calcium metabolism. Development of nasal formulation of hPTH (1–34). Clin Calcium 17:64–71
Matsumoto T, Shiraki M, Hagino H et al (2006) Daily nasal spray of hPTH(1–34) for 3 months increases bone mass in osteoporotic subjects: a pilot study. Osteoporos Int 17:1532–1538
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schneider, R., Ramaswamy, A., Slater, E.P. et al. Cryopreservation of Parathyroid Tissue after Parathyroid Surgery for Renal Hyperparathyroidism: Does it Really Make Sense?. World J Surg 36, 2598–2604 (2012). https://doi.org/10.1007/s00268-012-1730-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1730-x