Abstract
We evaluated our experience of subtotal parathyroidectomy (SP) for secondary hyperparathyroidism (SHP) cases. We evaluated retrospectively our 150 SP operations due to SHP. Serious hypocalcemia (< 6.5 mg/dL) developed in 23 (15.3%) patients, and we performed cryopreserved parathyroid cell autotransplantation in four cases with successful results. Recurrent hyperparathyroidism developed in 3 (2%) cases, and persistent hyperparathyroidism was observed in 22 (14.6%) cases. Upon reoperation in nine persistent hyperparathyroidism cases, we found supernumerary parathyroid glands in three cases, remnant tissue hyperplasia in four cases, and ectopic parathyroid glands in two cases. Among cases in which four glands cannot be found during surgery, the permanent HP rate is high. Serious hypocalcemia may develop postoperatively, and cryopreserved parathyroid autotransplantation may be inevitable in some of these cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most common cause of secondary hyperparathyroidism (SHP) is chronic renal failure. The mechanism of SHP in chronic renal failure is not clear, but imbalance among serum levels of calcium, phosphate, and vitamin D is an important part of the physiopathological process. Regardless of the mechanism, serum levels of parathormone (PTH) are markedly high and all parathyroid glands exhibit nodular or diffuse hyperplasia [1]. Although the first step in the treatment of SHP is the administration of vitamin D preparations, phosphate-binding pharmaceuticals, and calcimimetic agents, 15–40% of patients do not respond to this treatment and their serum levels of calcium, phosphate, and PTH continue to increase [2].
Subtotal parathyroidectomy (SP) may be necessary in such cases. Successful parathyroid surgery increases patients’ quality of life and contributes to the success of renal transplantation [3, 4]. In this study, we evaluated the results of SPs that we performed in 150 patients with SHP.
Methods
The protocol for this retrospective clinical study was approved by the human ethics committee of Bezmialem Vakif University. All patients were informed about the study, and written informed consent was obtained. Of the 178 patients diagnosed with SHP in the Bezmialem Vakif University Endocrine Surgery outpatient clinic between June 2013 and December 2017, 150 patients (82 men, 68 women; sex ratio, 1.2; age range, 26–69 years; mean age, 39.5 years) were randomized according to the following criteria and underwent SP. Two surgeons with endocrinology experience performed all SPs. Operated cases met the following criteria, defined according to the 2012 and 2016 Kidney Disease Improving Global Outcomes guidelines (10): end-stage chronic renal failure; renal dialysis not less than twice per week; serum levels of PTH > 500 pg/mL; hyperphosphatemia and/or hypercalcemia and/or Ca × P > 70 mg; resistance to conventional medical therapy; and one or more of the following intensified clinical symptoms: ostalgia and arthralgia, pruritus, pathological fracture, metastatic and vascular calcifications, and signs of calciphylaxis.
Patients were evaluated preoperatively by neck ultrasonography and methoxy isobutyl isonitrile scanning. Serum calcium (normal range, 8.0–10.2 mg/dL) and phosphorus (normal range, 2.5–4.5 mg/dL) levels of all patients were evaluated after normalizing serum vitamin D (normal range, 20–50 ng/mL) level. When the serum albumin level is lower than normal range (3.4–5.4 g/dL), we used serum albumin level correction formulation for evaluation of serum calcium level (serum calcium [mg/dL] + 0.8 (4.0 − serum albumin [g/dL]). Hemodialysis was performed without heparinization on the day before surgery or the morning of the operative day. According to the standard SP procedure, four parathyroid glands were searched intraoperatively; three glands were completely resected and the fourth gland was partially resected, leaving about 1 cm3 tissue volume. The parathyroid tissue to be left in the patient was marked with two medium metallic clips.
When four glands were found, the surgeons did not search for supernumerary glands. When four glands were not found, the thyrothymic ligament, peritracheal, periesophageal, and pericarotideal regions were investigated. Thymectomy was performed when the gland(s) was not found.
All excised glands were bisected; one-half of each gland was sent to the pathology laboratory for routine histopathological evaluation and the other half was sent to our cryopreservation laboratory in an Eppendorf tube under sterile conditions.
Patients were not discharged for at least 2 days after surgery. Patients who exhibited significant reduction in serum levels of calcium (to ˂ 7 mg/dL) and/or significant hypocalcemic symptoms were admitted and treated with calcium and vitamin D preparations until they reached a normocalcemic, asymptomatic state.
Patients underwent blood testing and physical examination on postoperative days 1, 3, and 7 and then at 1, 3, and 6 months. Persistent HP was defined as serum levels of PTH > 300 pg/mL and/or calcium levels > 10 mg/dL in the first 6 months postoperatively. Recurrent HP was defined as serum levels of PTH > 300 pg/mL and/or calcium levels > 10 mg/dL after 6 months postoperatively.
Results
The mean duration of chronic kidney disease was 92 months (range, 12–153 months) and hemodialysis was 53 months (range, 16–137 months). The mean duration of the SP operations was 58 min (range, 35–205 min). The mean follow-up period was 28 months (range, 2–55 months). The mean duration of hospitalization was nearly 3.5 days (range, 2–13 days). Four parathyroid glands were found intraoperatively in 141 (94%) patients but not in 9 (6%) patients. Four (45%) of these nine cases progressed to permanent HP, but no permanent HP or recurrent HP was observed in the remaining five (55%) cases. Three hemithyroidectomies were performed due to an intrathyroidal parathyroid gland (n = 1) and suspected malignant thyroid nodules (n = 2). No recurrent laryngeal nerve injuries occurred, but transient unilateral paresis was noted in two (1.3%) cases. Serious hypocalcemia (serum calcium < 6.5 mg/dL) was observed in 23 (15.3%) patients; the mean serum levels of calcium were 5.6 mg/dL (range, 3.4–6.5 mg/dL). Serum levels of PTH on postoperative day 1 were < 50 pg/mL in 11 of these 23 cases, < 100 pg/mL in nine cases, and < 300 pg/mL in three cases (Table 1). Four (2.6%) of these patients did not reach a normocalcemic and/or asymptomatic state. Their serum levels of calcium on postoperative day 1 were < 50 pg/mL, and we performed parathyroid autotransplantation at a mean of 8 days after surgery (range, 6–10 days; Table 1).
For autotransplantation, we gradually dissolved cryopreserved parathyroid tissues by removing them from a freezer at − 80 °C. The tissues were disrupted by mechanical isolation and autotransplanted by injection into the deltoid muscle with 2 mL of physiological serum. After transplantation, all of these patients became asymptomatic and were discharged within several days.
Nine patients died. One patient (a 66-year-old woman) died on postoperative day 4 due to acute myocardial infarction in the intensive care unit. The other eight patients died of nonsurgical (metabolic) reasons with a mean of 16 months (range, 9–51 months) after surgery.
Three (2%) cases progressed to recurrent HP in postoperative months 9, 14, and 23, respectively (Table 1). Twenty-two (14.6%) cases progressed to persistent HP. In 16 of these cases, we readily found four parathyroid glands in natural anatomic locations intraoperatively and had no intraoperative difficulties (e.g., prolonged operation time, thyroid anomalies, ectopic or supernumerary parathyroid glands). In 4 of the 22 cases, one gland was not found intraoperatively; we experienced some difficulty with two of these cases due to ectopic thyroid tissue and location of both inferior parathyroid glands in the thymus, respectively. Nine of these patients had persistent HP and underwent reoperation; three of these patients had supernumerary glands (five in two cases, six in one case), four had remnant parathyroid tissue hyperplasia, and two had ectopic parathyroid tissues (one in the superior mediastinum, excised with a neck incision; one in the inferior mediastinum, excised with a thoracoscopic approach; Table 2).
Discussion
SHP may cause serious complications, including metabolic bone disease, severe atherosclerosis, and cardiovascular events [5]. Although vitamin D, phosphate-binding drugs, and calcimimetic agents are options for medical treatment, parathyroid surgery is required in about 20% of patients after 3–10 years of dialysis and in up to 40% of patients after 20 years [6, 7].
Surgical approaches for the treatment of SHP have some controversial aspects, including indications for operation [8,9,10], type of surgery selected (total or subtotal parathyroidectomy, immediate autotransplantation or not) [9, 11], and postoperative observation procedures (calcium supplementation alone, vitamin D and calcium supplementation, or none) [12, 13].
Hypercalcemia, hyperphosphatemia, and HP are silent and asymptomatic conditions when no serious bone damage occurs. Patients do not want to accept surgical intervention in the absence of serious symptoms or drug-related side effects (particularly those related to new-generation phosphate-binding agents) [14, 15].
Medical center and surgeon experience is the most important factor for successful SHP surgery, as with some other rare surgical interventions. Results of inexperienced centers are directly related to persistent and recurrent HP [6, 16].
Bezmialem Vakif University is the only center in Turkey that is licensed to perform parathyroid allotransplantation. Our donors are patients with SHP, and we have very close relationships with dialysis centers with so many SHP cases that are referred to our clinic. Hence, we have abundant experience with SHP surgery.
In our series, only 2% of patients developed recurrent HP. Other studies have reported rates of 4–10% [6, 17, 18]. Close follow-up to ensure calcium sensing receptor stimulation and secretion balance clearly prevents or delays the hyperplasic stimulation of remnant tissue [16, 17]. Thus, we follow our patients very closely postoperatively, with careful use of calcium and vitamin D supplementation and organized regular dialysis. Our relatively low rate of recurrence may be related to this approach.
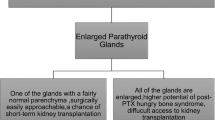
We observed persistent HP in 22 (14.6%) cases. This percentage ranges from 5 to 34% in the literature [11, 19]. We did not have any technical difficulties during surgery in 16/22 cases of persistent HP; we readily found four parathyroid glands and no ectopic parathyroid tissue or congenital anomalies affecting the thyroid and/or parathyroid glands, with no prolongation of the operation time. The main factor for preventing permanent HP is the identification of four parathyroid glands during surgery. The surgeon must insist on finding four glands in difficult cases, and, when necessary, not hesitate to perform thymectomy [20, 21]. According to this recommendation, we insisted on finding four glands in all of our operations and performed thymectomy when necessary, but we did not find all of the glands in nine (6%) cases. Four of these nine patients developed permanent HP, as expected, but surprisingly, five of these patients were normoparathyroidic and normocalcemic at a mean of 28 months postoperatively. The mechanism of this situation is not clear, but the missing glands may have been healthy, rather than hyperplastic.
We reoperated in nine cases of persistent HP and found supernumerary parathyroid glands in three cases (five in two cases, six in one case), remnant tissue hyperplasia in four cases, and ectopic parathyroid tissue in the superior and inferior mediastinum, respectively, in two cases. Dumitras et al. found supernumerary glands in 7% of 202 SHP cases [27], and Akerstrom found them in 13% of 503 autopsies of healthy people. The authors do not recommend exploration for supernumerary glands when intraoperative anomalies are not detected and suggest that unnecessary exploration may increase morbidity [20,21,22].
Pronounced postoperative hypocalcemia (Ca ˂ 7 mg/dL) is a serious clinical situation. In this study, patients with serum levels of PTH ˂ 50 pg/mL on postoperative day 1 were not discharged, and they received supplementation with oral and/or intravenous calcium and vitamin D preparations. When symptomatic hypocalcemia persists despite aggressive calcium and vitamin D supplementation therapy, autotransplantation is indicated. For successful autotransplantation in the postoperative period, patients’ parathyroid tissue must be cryopreserved and appropriate laboratory conditions with trained staff are necessary [23,24,25].
Because we perform parathyroid allotransplantation, we have a specific parathyroid cryopreservation laboratory and trained staff. When no contagious disease is detected preoperatively, in SHP cases, we routinely send one-half of the excised parathyroid tissue to the pathology laboratory and the other half to the cryopreservation laboratory. Reported success rates of autotransplantation of cryopreserved parathyroid tissue range from 20 to 100% [22, 25]. Many factors affect the success of the procedure, but viability and functionality are the main factors [26, 27]. All transplantations were successful, and the patients were free from serious hypocalcemia and other symptoms and discharged within 13 days in this study.
Therefore, the effort to find four parathyroid glands in each SP operation is very important. Among cases in which four glands cannot be found during surgery, the permanent HP rate is high; however, about half of these patients become normoparathyroidic postoperatively for unknown reasons. On the other hand, persistent or recurrent HP may develop in cases in which four glands are found intraoperatively. Serious hypocalcemia may develop postoperatively, and cryopreserved parathyroid autotransplantation is inevitable in some of these cases.
References
Tominaga Y, Kohara S, Namii Y, Nagasaka T, Haba T, Uchida K, Numano M, Tanaka Y, Takagi H (1996) Clonal analysis of nodular parathyroid hyperplasia in renal hyperparathyroidism. World J Surg 20:744–752
Fassbinder W, Brunner FP, Brynger H, Ehrich JHH, Geerlings W, Raine AEG, Rizzone G, Selwood NH, Tuveson G, Wing AJ (1991) Combined report on regular dialysis and transplantation in Europe XX. Nephrol Dial Transplant 6:5–35
Abraham T (2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 113:1–130
Jha V, Arici M, Collins AJ, Garcia-Garcia G, Hemmelgarn BR, Jafar TH, Pecoits-Filho R, Sola L, Swanepoel CR, Tchokhonelidze I, Wang AY, Kasiske BL, Wheeler DC, Spasovski G, Conference Participants (2016) Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int 90:1164–1174. https://doi.org/10.1016/j.kint.2016.09.009
Malberti F, Marcelli D, Conte F, Limido A, Spotti D, Locatelli F (2001) Parathyroidectomy in patients on renal replacement therapy: an epidemiologic study. J Am Soc Nephrol 12:1242–1248
Tominaga Y, Uchida K, Haba T, Katayama A, Sato T, Hibi Y (2001) More than 1,000 cases of total parathyroidectomy with forearm autograft for renal hyperparathyroidism. Am J Kidney Dis 38:168–171
Fassbinder W, Brunner FP, Brynger H, Ehrich JH, Geerlings W, Raine AE (1991) Combined report on regular dialysis and transplantation in Europe, XX, 1989. Nephrol Dial Transplant 1:5–35
Madorin C, Owen RP, Fraser WD, Pellitteri PK, Radbill B, Rinaldo A (2012) The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol 269:1565–1576
Tominaga Y, Matsuoka S, Uno N (2009) Surgical and medical treatment of secondary hyperparathyroidism in patients on continuous dialysis. World J Surg 33:2335–2342
Fukagawa M, Yokoyama K, Koiwa F (2013) Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Therapher Dial 17:247–288
Lorenz K, Ukkat J, Sekulla C, Gimm O, Brauckhoff M, Dralle H (2006) Total parathyroidectomy without autotransplantation for renal hyperparathyroidism: experience with a qPTH-controlled protocol. World J Surg 30:743–751
Viaene L, Evenepoel P, Bammens B, Claes K, Kuypers D, Vanrenterghem Y (2008) Calcium requirements after parathyroidectomy in patients with refractory secondary hyperparathyroidism. Nephron Clin Pract 110:80–85
Bratucu MN, Garofil ND, Radu PA, Paic V, Zurzu M, Goleanu V, Popa F, Strambu V, Straja DN (2015) Surgical attitude in patients with secondary hyperparathyroidism undergoing dialysis. Chirurgia 110:418–424
Mircescu G, Stanescu B (2010) Surgical or medical therapy for severe hyperparathyroidism of chronic kidney disease? An appraisal of current practice guidelines. Acta Endo (Buc) 6:541–576
Ozmen T, Manukyan M, Sen S, Kahveci A, Yegen C, Gulluoglu B (2014) Is three-gland-or-less parathyroidectomy a clinical failure for secondary hyperparathyroidism. Ulusal Cer Derg 30:201–206
Konturek A, Barczyński M, Stopa M, Nowak W (2016) Subtotal parathyroidectomy for secondary renal hyperparathyroidism: a 20-year surgical outcome study. Langenbeck's Arch Surg 401:965–974
Low TH, Yoo J (2017) Subtotal parathyroidectomy and relocation of the parathyroid remnant for renal hyperparathyroidism: modification of a traditional operation. J Otolaryngol Head Neck Surg 23:46–51. https://doi.org/10.1186/s40463-017-0238-7
Neagoe RM, Mureșan M, Voidăzan S, Pașcanu I, Radu CP, Sala DT (2016) Subtotal parathyroidectomy versus total parathyroidectomy with autotransplant in secondary hyperparathyroidism. A single-centre prospective cohort of 43 patients. Endokrynol Pol 67:202–209. https://doi.org/10.5603/EP.a2016.0013
Kinnaert P, Tielemans C, Dhaene M, Decoster-Gervy C (1998) Evaluation of surgical treatment of renal hyperparathyroidism by measuring intact parathormone blood levels on fist postoperative day. World J Surg 22:695–699
Madorin C, Owen RP, Fraser WD (2012) The surgical management of renal hyperparathyroidism. Eur Arch Oto-Rhino-L 269:1565–1576
Low TH, Clark J, Gao K (2009) Outcome of parathyroidectomy for patients with renal disease and hyperparathyroidism: predictors for recurrent hyperparathyroidism. ANZ J Surg 79:378–382
Akerstrom G, Malmaeus J, Bergstrom R (1984) Surgical anatomy of human parathyroid glands. Surgery 95:14–21
Saxe AW, Spiegel AM, Marx SJ, Brennan MF (1982) Deferred parathyroid autografts with cryopreserved tissue after reoperative parathyroid surgery. Arch Surg 117:538–543
Wagner PK, Seesko HG, Rothmund M (1991) Replantation of cryopreserved human parathyroid tissue. World J Surg 15:751–755
Caccitolo JA, Farley DR, van Heerden JA, Grant CS, Thompson GB, Sterioff S (1997) The current role of parathyroid cryopreservation and autotransplantation in parathyroid surgery: an institutional experience. Surgery 122:1062–1067
Cohen MS, Dilley WG, Wells SA, Moley JF, Doherty GM, Sicard GA, Skinner MA, Norton JA, DeBenedetti MK, Lairmore TC (2005) Long-term functionality of cryopreserved parathyroid autografts: a 13-year prospective analysis. Surgery 138:1033–1040
Borot S, Lapierre V, Carnaille B, Goudet P, Penfornis A (2010) Results of cryopreserved parathyroid autografts: a retrospective multicenter study. Surgery 147:529–535
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol for this retrospective clinical study was approved by the human ethics committee of Bezmialem Vakif University. All patients were informed about the study, and written informed consent was obtained.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aysan, E., Piraliyev, E. & Yigman, S. Results of 150 Subtotal Parathyroidectomies for Secondary Hyperparathyroidism. Indian J Surg 82, 801–805 (2020). https://doi.org/10.1007/s12262-020-02119-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02119-9