Abstract
Background
In the present study we present a unique maneuver, using both fibrin glue and polyglycolic acid (PGA) sheets, for repairing intraoperative pulmonary air leakage, and report our clinical results.
Methods
Based on the results from in vitro experiments, we retrospectively investigated the clinical effects of our method for repairing intraoperative pulmonary air leakage in 377 consecutive patients, who underwent a pulmonary resection for primary lung cancer or metastatic lung tumors from 2004 to 2009. From April 2004 through September 2007, repair of intraoperative pulmonary air leakage was performed in 204 patients using only fibrin glue. From October 2007 through December 2009, the repair was performed in 173 patients with a unique application of both fibrin glue and PGA sheets, i.e., (1) rubbing fibrin glue A solution, (2) applying a PGA sheet cut to an appropriate size, (3) rubbing fibrin glue B solution on the PGA sheet, and (4) reapplying fibrin glue A solution and rubbing.
Results
The mean duration of postoperative pleural drainage was significantly shorter in the latter time period when both fibrin glue and PGA sheets were used than in the former period when fibrin glue was used alone. The incidence of prolonged air leakage longer than 1 week was also significantly lower in the latter era than in the former era.
Conclusion
Our unique application of both fibrin glue and PGA sheets for the intraoperative repair of pulmonary air leakage effectively resulted in a shortening of the duration of postoperative pleural drainage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative air leakage from the residual lung is a potential complication after pulmonary resection, resulting in prolonged hospitalization [1, 2]. Although various postoperative management strategies for pulmonary air leakage have been applied, including a water-sealing technique of pleural drainage [3–5], intraoperative repair of pulmonary fistulas from dissected lung parenchyma or suture lines on the lung is considered essential for prevention of postoperative persistent air leakage [6–10]. To protect against prolonged air leakage after a pulmonary resection, an intrapleural injection of OK-432, a lyophilized preparation of the heat- and penicillin-treated Su strain of the Streptococcus pyogenes group A3 bacterium, is often performed for pleurodesis in Japan; however, this has several disadvantages due to the inflammatory reaction [11]. Recently, the advent of both fibrin glue and polyglycolic acid (PGA) sheets has improved the repair of pulmonary air leakage [9, 10, 12]. However, the most effective method for applying both the fibrin glue and the PGA sheets has not yet been established.
In the present study we present a unique maneuver using both fibrin glue and PGA sheets for intraoperative pneumostasis, and report our clinical experiences using this new application method.
Patients and methods
The sealing effect of combined fibrin glue and PGA sheets
The sealing ability of the combined fibrin glue and PGA sheets was evaluated by the pressure test model, as reported by Terasaka et al. [13]. As shown in Fig. 1, a 3-cm-diameter orifice in a 240-ml plastic bottle was covered with skin from an 11–20-week-old female Japanese white rabbit; the skin had a 1.5-cm-diameter hole in the center (A in Fig. 1). The hole was repaired with both fibrin glue (1 ml) and a PGA sheet (2.5 cm × 2.5 cm) using either the simple over-spraying method of fibrin glue to the PGA sheet or the present unique maneuver described below. Then, the inside of the bottle was pressurized through a connected pressure syringe (B in Fig. 1). Seal-breaking pressures were measured with an interconnected manometer (C in Fig. 1; POP760, Okano, Osaka, Japan). All animals received humane care in accordance with the Japanese Government Animal Protection and Management Law.
a, b Experimental equipment used for the sealing test. The equipment included (A) a 3-cm-diameter orifice cut out of a 240-ml plastic bottle and covered with rabbit skin, which had a 1.5-cm-diameter hole in the center; (B) the pressure syringe; and (C) an interconnected manometer measuring seal-breaking pressures
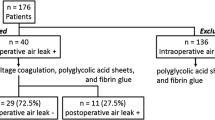
Patients
We retrospectively investigated 377 consecutive patients who underwent a pulmonary resection (lobectomy, segmentectomy, or wedge resection) for primary lung cancer or metastatic lung tumors from April 2004 to December 2009 at our hospital. In the 204 patients who underwent surgery from April 2004 through September 2007, pulmonary air leaks during surgery were treated using only fibrin glue. In the more recent 173 patients who underwent surgery from October 2007 through December 2009, pulmonary air leaks during surgery were treated with the combined use of both fibrin glue and PGA sheets. Informed consent for the use of fibrin glue with or without PGA sheets was preoperatively obtained from all the patients. This study was approved by the Kyushu University Institutional Review Board for Clinical Research.
Management of chest tubes
The detailed perioperative care for patients who underwent pulmonary resection was described elsewhere [14]. Before the closure of the wounds, a 24-Fr chest tube was placed in the pleural cavity of the surgical site. Postoperatively, the chest tube was continuously suctioned at −5 cm H2O. If air leakage was absent and the volume of pleural effusion was less than 200 ml/day, the chest tube was removed the next day. Persistent air leakage of longer than 1 week was defined as “prolonged air leakage.”
Sealants for alveolar air leakage
PGA sheets (Neoveil®, Gunze, Kyoto, Japan) are made from a homopolymer nonwoven fabric with a thickness of 0.15 mm. The fibrin glue (Bolheal®, Chemo-Sero Therapeutic Research Institute, Kumamoto, Japan; Beriplast P®, CSL-Behring KK, Tokyo, Japan) is composed of solution A containing human fibrinogen and solution B containing human thrombin.
Intraoperative maneuver to repair pulmonary air leakage
After pulmonary resection, the saline submersion test with an inspiratory hold pressure of +20 cm H2O was routinely performed. In the presence of alveolar air leakage, fibrin glue was applied in patients from April 2004 through September 2007. Fibrin glue A solution was first rubbed into the dissected pulmonary parenchyma or stapled lines, and then the B solution was applied. Those maneuvers were repeated until pneumostasis was achieved. From October 2007 through December 2009, both fibrin glue and PGA sheets were used for pneumostasis. The procedure is shown in Fig. 2 and consisted of (1) rubbing the parenchyma or staple lines with fibrin glue A solution, (2) applying a PGA sheet cut to an appropriate size, (3) rubbing fibrin glue B solution on the PGA sheet with the handle of a pair of tweezers, and (4) reapplying fibrin glue A solution and rubbing with the handle of the tweezers. Ninety-eight patients were treated with this pneumostasis method. Figure 3 is an intraoperative photo of the final application of the treatment procedures.
Statistical analysis
Comparisons of clinical variables between the two groups were performed using Fisher’s exact test for nominal variables and Student’s t-test for continuous variables. A two-sided P value <0.05 was considered to be statistically significant.
Results
Experimental sealing using fibrin glue and PGA sheets
The in vitro sealing experiment was performed ten times for each method. With the simple over-spraying method, the measured seal-breaking pressure ranged from 31 to 150 mmHg, with a mean of 107.5 mmHg. On the other hand, the pressure in the experiment of our unique method, which ranged from 83 to 320 mmHg with a mean of 206 mmHg, was about twofold higher than that for the simple over-spraying method (P = 0.003) (Fig. 4).
Patients’ backgrounds
A comparison of the profiles of the patients from the two time periods, i.e., April 2004 through September 2007 (fibrin glue alone) and October 2007 through December 2009 (fibrin glue plus PGA sheets), is given in Table 1. There were no significant differences between the two groups of patients in gender, pulmonary function (presence of chronic obstructive diseases), disease type, the administration of preoperative chemotherapy (with or without radiotherapy), or extent of pulmonary resection. The group that was treated with a combination of both fibrin glue and PGA sheets was slightly younger than the group treated with only fibrin glue.
Postoperative air leakage
As shown in Table 2, the mean duration of postoperative plural drainage was significantly shorter in the latter era with the use of both fibrin glue and PGA sheets than in the former era treated with fibrin glue alone (2.7 ± 1.55 vs. 4.2 ± 2.10 days, P < 0.01). The incidence of prolonged air leakage longer than 1 week was also significantly lower in the latter era than in the former era (Table 2). All of the patients with prolonged air leakage required pleurodesis with OK-432, a lyophilized preparation of the heat- and penicillin-treated Su strain of the S. pyogenes group A3 bacterium.
Discussion
The present study clearly showed that the use of a combination of fibrin glue and PGA sheets for the intraoperative repair of pulmonary air leakage could shorten the duration of postoperative pleural drainage and also decrease the incidence of prolonged postoperative air leakage in comparison with the use of fibrin glue alone. In the present study we included all of the patients operated on in the study time period, not just the patients who experienced intraoperative air leakage, and compared the postoperative results between the two eras. We did this for two reasons: first, the present study was a retrospective observational study. We usually applied each repair method and confirmed the repair by examining the patients for the presence of intraoperative air leakage under +20 cm H2O pressure in the respective era. However, in practice, even in the absence of air leakage under +20 cm H2O pressure during the operation, some patients still suffered from postoperative air leakage, especially emphysematous patients. Therefore, we occasionally applied repair methods in such patients who were considered to be likely to develop air leakage postoperatively. Accordingly, especially in consideration of the retrospective nature of the present study, it is better to include all the patients regardless of the presence of intraoperative air leakage or the application of this repair method. Second, in order to assess the effects of the repair methods, we also compared the incidence of prolonged air leakage. Except for the use of PGA sheets, we did not change the perioperative management between the two eras, including the type or model of staplers used. Of interest, we noted even during surgery that the combined application of PGA sheets with the fibrin glue could ease and reinforce pneumostasis in comparison with the use of the fibrin glue alone. Based on the present results, we recommend that the PGA sheets should be used in combination with fibrin glue as follows: (1) rub the fibrin glue A solution over the lung parenchyma or staple line, (2) apply a PGA sheet cut to an appropriate size, (3) rub the fibrin glue B solution over the PGA sheet with the handle of a pair of tweezers, and (4) reapply the fibrin glue A solution and rub with the handle of the tweezers.
Usually, the PGA sheet is applied to the air leakage surface first and then over-sprayed with both fibrin glue A solution and B solution. Using this maneuver, the pulmonary fistula is covered with only the PGA sheet and is thus more likely to burst as a result of incidentally high alveolar air pressure. Using our method, the pulmonary fistula is first sealed with fibrin glue before the PGA sheet is overlaid and fixed. The fibrin glue A solution first penetrates into the dissected pulmonary parenchyma and then forms fibrin with solution B through the PGA sheet (①–③ in Fig. 2). Furthermore, reapplication of the A solution rigidly fixes the PGA sheet both inside and out (④ in Fig. 2).
Methods that suggest first rubbing the fibrin glue solution A over the dissected pulmonary parenchyma have been reported by other investigators [9, 15]. However, they sprayed both fibrin glue B solution and A solution after they rubbed A solution and applied the PGA sheet. In our method fibrin glue B solution is not sprayed but dropped and rubbed over the PGA sheet with the handle of a pair of tweezers. Thereafter, fibrin glue A solution is also reapplied in the same manner. The use of the handle of a pair of tweezers gently fixes the PGA sheet over the ruptured lung surface through a minithoracotomy window. In comparison to the spraying method, the dropping-and-rubbing method enables better penetration of the fibrin glue B solution into the PGA sheet and saves both fibrin glue B solution and A solution.
PGA sheets are now widely used for repairing air leaks in general thoracic surgery without any significant adverse effects. However, Nakamura et al. [16] reported the induction of a fibrotic reaction and pleural adhesion around the applied PGA material. Therefore, limited usage of PGA should be taken into consideration. In our method, the PGA sheet is cut to an appropriate size for the dissected lung parenchyma or suture lines of the lung prior to its application. This minimal usage of PGA sheets is thought to contribute to the procedure being safe and cost-effective.
Since the present study was retrospective, there is a flaw in the study design in that it lacks data about the duration of pleural drainage of a control group without any treatment to prevent or repair intraoperative air leakage. However, the absence of prolonged air leakage in the second period of the study in which a combination of fibrin glue and PGA sheets was used is considered to be noteworthy. In conclusion, our new method for repairing pulmonary air leaks using both fibrin glue and PGA sheets might therefore be useful for chest surgeons as a better procedure for preventing air leaks due to pulmonary resection.
References
Lackey A, Mitchell JD (2010) The cost of air leak: physicians’ and patients’ perspectives. Thorac Surg Clin 20:407–411
Shoji F, Yano T, Yoshino I, Kawano D et al (2009) The dynamics and clinical significance of alpha 2 plasmin inhibitor–plasmin complex and thrombin–antithrombin complex in postoperative pleural effusion following a pulmonary lobectomy. Surg Today 39:320–325
Cerfolio RJ, Bass C, Katholi CR (2001) Prospective randomized trial compares suction versus water seal for air leaks. Ann Thorac Surg 71:1613–1617
Okamoto J, Okamoto T, Fukuyama Y et al (2006) The use of a water seal to manage air leaks after a pulmonary lobectomy: a retrospective study. Ann Thorac Cardiovasc Surg 12:242–244
Bertholet JWM, Joosten JJA, Keemers-Gels ME et al (2010) Chest tube management following pulmonary lobectomy: change of protocol results in few air leaks. Interact Cardiovasc Thorac Surg 112:28–31
Porte HL, Jany T, Akkad R et al (2001) Randomized controlled trial of a synthetic sealant for preventing alveolar leaks after lobectomy. Ann Thorac Surg 71:1618–1622
Kawamura M, Gika M, Izumi Y et al (2005) The sealing effect of fibrin glue against alveolar air leakage evaluated up to 48 h; comparison between different methods of application. Eur J Cardiothorac Surg 28:39–42
Fabian T, Federico JA, Ponn RB (2003) Fibrin glue in pulmonary resection: a prospective, randomized, blinded study. Ann Thorac Surg 75:1587–1592
Miyamoto H, Futagawa T, Wang Z et al (2003) Fibrin glue and bioabsorbable felt patch for intraoperative intractable air leaks. Jpn J Thorac Cardiovasc Surg 51:232–236
Ueda K, Tanaka T, Jinbo M et al (2007) Sutureless pneumostasis using polyglycolic acid mesh as artificial pleura during video-assisted major pulmonary resection. Ann Thorac Surg 84:1858–1861
Uehara T, Yano T, Kuninaka S et al (2000) The influence of enhanced postoperative inflammation by the intrapleural administration of streptococcal preparation (OK432) on the prognosis of completely resected non-small-cell lung cancer. J Surg Oncol 5:51–54
Ueda K, Tanaka T, Jinbo M et al (2010) Sutureless pneumostasis using bioabsorbable mesh and glue during major pulmonary resection for cancer: who are the best candidates? J Thorac Cardiovasc Surg 139:100–105
Terasaka S, Iwasaki Y, Shinya N, Uchida T (2006) Fibrin glue and polyglycolic acid nonwoven fabric as a biocompatible dual substitute. Neurosurgery 58:134–139
Yano T, Shoji F, Koga T (2006) Is oxygen supplementation needed after standard pulmonary resection for primary lung cancer? Ann Thorac Cardiovasc Surg 12:393–396
Gika M, Kawamura M, Izumi Y, Kobayashi K (2007) The short-term efficacy of fibrin glue combined with absorptive sheet material in visceral pleural defect repair. Interact Cardiovasc Thorac Surg 6:12–15
Nakamura T, Suzuki K, Mochizuki T et al (2010) An evaluation of the surgical morbidity of polyglycolic acid felt in pulmonary resections. Surg Today 40:734–737
Acknowledgments
We thank the Chemo-Therapeutic Research Institute, Kumamoto, Japan, for their valuable experimental assistance.
Conflicts of interest
The authors have no conflicts of interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yano, T., Haro, A., Shikada, Y. et al. A Unique Method for Repairing Intraoperative Pulmonary Air Leakage with Both Polyglycolic Acid Sheets and Fibrin Glue. World J Surg 36, 463–467 (2012). https://doi.org/10.1007/s00268-011-1355-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-011-1355-5