Abstract
Objective
We evaluated the efficacy of low-voltage coagulation (LVC) with polyglycolic acid (PGA) sheets (Neoveil, GUNZE Ltd., Japan) and fibrin glue to control intraoperative alveolar air leaks after lung surgery.
Methods
We included 176 patients with non-small cell lung cancer who underwent thoracoscopic lobectomies. When alveolar air leak was confirmed after lung resection, we applied LVC system to the pleural defect followed by layers of PGA sheets and fibrin glue (n = 40). We then analyzed postoperative air leaks (rate of occurrence and duration time).
Results
73% of patients (29/40 cases) experienced no postoperative air leaks. Although 11 patients experienced air leaks after surgery, there were no prolonged air leaks (>7 days) (resolution time, 3.5 ± 1.4 days; range, 2–6 days). Two patients required drainage for late-onset air leaks, but their conditions improved without further treatment. There were no further adverse events.
Conclusions
The use of LVC with PGA sheets and fibrin glue following pulmonary resection efficiently prevented both intraoperative air leaks and prolonged air leaks after lung surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intraoperative alveolar air leaks are a common complication following pulmonary resection [1, 2], and they result in prolonged chest tube drainage time and potentially longer lengths of hospital stay [3]. In particular, air leaks that persist for more than 7 days after surgery, which have traditionally been defined as prolonged air leaks, are associated with greater risk and increased length of hospitalization [4], and occur in 6–7% of patients after pulmonary resection [5, 6]. Therefore, the prevention of prolonged air leaks after lung surgery has been a major clinical objective. Fibrin glue has been used for the last 20 years [7,8,9,10,11] to prevent alveolar air leaks and is considered effective [12]. However, we have observed air leaks after lung surgery with fibrin glue applications. In this study, we developed a more effective method of using fibrin glue by applying low-voltage coagulation (LVC) before covering damaged tissue with polyglycolic acid (PGA) sheets (Neoveil, Gunze Ltd., Kyoto, Japan) and fibrin glue to prevent air leaks after lung resection.
Materials and methods
Patients
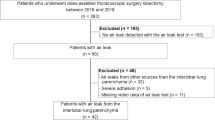
This study was performed with the approval of the Nara Medical University Ethics Committee (Approval Number 1270). We performed a retrospective review of prospectively collected chart data for 176 patients with non-small cell lung cancer who underwent thoracoscopic lobectomy at Nara Medical University Hospital, Japan, from January 2014 to December 2015. Intraoperative air leaks were observed in 40/176 patients, and these patients were eligible and enrolled in this study. On the assumption that this operative method must be adaptable to any lung surgery, there were no exclusion criteria and all pulmonary resection in our institution were potential subjects for this study during this period. To suppress variations in the research subjects, we examined patients who underwent lobectomy with lung cancer in this study.
Low-voltage coagulation (LVC)
We used LVC system (energy platform: ForceTriad™, Covidien, Boulder, CO; electrosurgical pencil: Two-Way Hand Control Mes-Holder 3P, SEMCO, Tokyo, Japan) in the cut mode with 15-W output power. A round-tipped electrode (electrosurgical electrode: Valleylab™ Ball Electrode, 5 mm, Covidien) was used to reduce contact resistance between the electrode and the coagulated tissue and to prevent sparks and carbonization.
Operative procedures
All patients received general anesthesia and were intubated with a double-lumen endotracheal tube to allow selective contralateral ventilation, then placed in the lateral decubitus position. The initial thoracoscope incision was made in the 7th or 8th intercostal space along the midaxillary line. A 1.5-cm incision was then made in the 4th or 5th intercostal space in the anterior axillary line, and an access incision (4–6 cm) was also located in the 4th or 5th intercostal space along the posterior axillary line in all patients for all the types of pulmonary resection. Interlobar dissection was completed using a stapler (iDrive™ Ultra Powered Stapling System, Covidien or ECHELON FLEX™ Powered ENDOPATH® Stapler, Ethicon), and an energy device (LigaSure™, Covidien or ENSEAL®, Ethicon) as both a vessel sealer and for lymph node dissection, transecting small sections of lung parenchyma with ligation, repeatedly. Once lobectomy and mediastinal lymph node dissection were complete, we performed an air leak test with 20-cm H2O pressure load. We excluded 136/176 patients with no air leakage or a small amount of air leak from the stapler line alone (Fig. 1). These patients were treated by applying layers of PGA sheets and fibrin glue (Beriplast P Combi-Set®, CSL Behring Pharma, Tokyo) to prevent further air leaks without LVC. When alveolar air leakage occurred from the pulmonary parenchyma (n = 40), it was managed as follows: LVC was applied to the pleural defect followed by applying layers of PGA sheets and fibrin glue to prevent further air leaks (Fig. 2).
Thoracoscopic views showing operation steps. a Air leakage from lung parenchyma. b Injured pulmonary parenchyma beside the intralobular stapler line and application of a low-voltage coagulation system on this pleural defect part of the lung. c Polyglycolic acid sheets attached to damaged lung tissue with fibrin glue. d Damaged lung tissue covered by polyglycolic acid sheets with fibrin glue
Evaluation items and statistical analyses
All patients received a 20-F chest tube at the end of the operation. The primary objective of this study was to analyze postoperative air leaks (rate of occurrence and duration time). Results were expressed as the mean ± standard deviation (SD) and range values. The patient characteristics in the study group were compared to the excluded patients, who did not have intraoperative air leak, using a Chi-square test.
Results
A total of 40/176 patients with lung resection fulfilled the inclusion criterion for the intraoperative water-sealing test and were enrolled in this study to evaluate LVC with PGA sheet and fibrin glue to prevent air leak (Table 1). 29 patients (72.5%) had no postoperative air leak. Although 11 patients (27.5%) experienced air leak after surgery, there were no prolonged air leaks (>7 days; time to resolution, 3.5 ± 1.4 days; range, 2–6 days) (Table 2). Two patients required drainage for late-onset air leak, but their conditions improved without further treatment. There were no further adverse events.
Discussion
Intraoperative options for alveolar air leak repair include suturing, stapling, and sealing with surgical sealants. The most popular sealant for lung surgery is fibrin glue, which has been used to prevent air leaks for the last 20 years [7,8,9,10,11]. However, fibrin glue has been reported to yield inconsistent results [7, 8] because of its inadequate bonding strength [13]. For this reason, PGA sheets are often used with fibrin glue in Japan. This combination has been reported to be more effective than using fibrin glue alone [12, 14, 15], and several application methods have been studied [12]. However, we still occasionally observe air leaks after lung surgery, even when using fibrin glue with PGA sheets.
Adhesion of fibrin glue to tissues results from the anchoring effect of the glue. Therefore, it is important to form a secure bond between the sealing material and the tissue, which is the reason for the addition of PGA sheets [12]. Although application methods of fibrin glue with or without PGA sheets have been extensively investigated, there are few studies of the application surfaces. If the surface is not dry, a secure bond cannot form, and the expected effect of fibrin glue is reduced. This was confirmed in a basic experiment showing that the bonding strength of the glue increases on a dry surface [16]. However, the condition of application surface has not been studied in clinical practice. Intraoperatively, the surface of the residual lung often contains moisture such as blood or effusion that prevents penetration of the fibrin glue and results in insufficient tissue-glue bonding. For this reason, we revised the fibrin glue method to be more appropriate by using LVC with electrocautery to maintain a dry surface by preventing seepage of blood and effusion. One of the major systems of LVC is soft-coagulation system (VIO 300 D; ERBE, Marietta, GA). Soft-coagulation systems efficiently control intraoperative bleeding without increasing bile leakage in liver surgery [17]. In thoracic surgery, soft-coagulation system efficiently stopped bleeding from the pulmonary artery [18] and was shown to be feasible for pulmonary resections [19]. In general, many surgeons have experienced that LVC prevents alveolar air leak. However, there is no experimental report to clearly present its effect. In clinical practices, solely LVC sometimes cannot control air leak completely, and is considered insufficient as a treatment to prevent air leak in some cases [20]. Therefore, we applied combination of LVC with PGA sheets and fibrin glue. In addition, the combination of soft coagulation with PGA sheets and fibrin glue has been shown to prevent pancreatic fistula after distal pancreatectomy [21]. In our study, we used LVC as soft-coagulation system with PGA sheets and fibrin glue to prevent alveolar air leaks. This method is simple without a need for special tools. However, when damage was too deep, we used either staple (in three cases) or suture methods (in one case).
Several reports have discussed the risk of bacterial infections leading to a higher incidence of empyema when polymeric synthetic products were used [22, 23]. We encountered no empyema cases in our study, although one case has occurred outside the study group that was caused by wound infection and that resolved with drainage and antibiotics without further surgery. Two patients required drainage for late-onset air leak, but the relationship with our method was unclear, and their conditions improved greatly with drainage alone, without adhesion therapy or surgical revision. However, as coagulation causes tissue damage, we are careful not to do unnecessary coagulation. There were no further adverse events associated with this technique, which was performed safely.
In the current study (n = 40), the mean duration of postoperative air leaks was 0.7 ± 1.4 days and the mean drain placement period was 3.1 ± 1.9 days (range, 1–10 days). Although a prospective randomized study is necessary to verify the effectiveness of this method, our results compare favorably with those of other recently reported methods of controlling alveolar air leak, with slight differences in study designs [24, 25]. We have experienced that the rate of occurrence of postoperative air leak in this method was 27.5%. On the other hand, in the case of using only PGA sheets and fibrin glue, Murakami and colleagues have reported that 53/112 (47.3%) was unsuccessful to stop intraoperative air leak [26]. In addition, based on an accurate predictive score for prolonged air leak (“the index of prolonged air leak”) [5, 6], the average score in our study group was >13.3, and the risk of prolonged air leak was greater than 10% (high risk). However, no prolonged air leaks were observed. The patient characteristics in this study were significantly different in sex, body mass index, and localization of the lung, compared to the excluded group who did not have intraoperative air leak (Table 1). Furthermore, in the patient factors who had postoperative air leak, we recognized that there is a tendency of male and superior lobe resection (Table 2).
The limitations of this study are that it was retrospectively performed without a control group, and this technique is still not appropriately prepared with enough basic and clinical evidences. Thus, the result is to be interpreted carefully, and further basic and prospective randomized studies are necessary to verify the effectiveness and safety of this method.
Preparing appropriate dry surface conditions when using LVC maximized the bonding strength of fibrin glue (with PGA sheets), and this combination was effectively used for postoperative air leakage prevention in our study. LVC combined with PGA sheets and fibrin glue after pulmonary resection efficiently prevented both intraoperative alveolar air leaks and prolonged air leaks.
References
Brunelli A, Varela G, Refai M, Jimenez MF, Pompili C, Sabbatini A, et al. A scoring system to predict the risk of prolonged air leak after lobectomy. Ann Thorac Surg. 2010;90:204–9.
Filosso PL, Ruffini E, Sandri A, Lausi PO, Giobbe R, Oliaro A. Efficacy and safety of human fibrinogen-thrombin patch (TachoSil®) in the treatment of postoperative air leakage in patients submitted to redo surgery for lung malignancies: a randomized trial. Interact Cardiovasc Thorac Surg. 2013;16:661–6.
Belda-Sanchis J, Serra-Mitjans M, Iglesias Sentis M, Rami R. Surgical sealant for preventing air leaks after pulmonary resections in patients with lung cancer. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.CD003051.pub3.
Anegg U, Rychlik R, Smolle-Juttner F. Do the benefits of shorter hospital stay associated with the use of fleece-bound sealing outweigh the cost of the materials? Interact Cardiovasc Thorac Surg. 2008;7:292–6. (discussion 26).
Rivera C, Bernard A, Falcoz PE, Thomas P, Schmidt A, Benard S, et al. Characterization and prediction of prolonged air leak after pulmonary resection: a nationwide study setting up the index of prolonged air leak. Ann Thorac Surg. 2011;92:1062–8. (discussion 68).
Orsini B, Baste JM, Gossot D, Berthet JP, Assouad J, Dahan M, et al. Index of prolonged air leak score validation in case of video-assisted thoracoscopic surgery anatomical lung resection: results of a nationwide study based on the French national thoracic database, EPITHOR. Eur J Cardiothorac Surg. 2015;48:608–11.
Fleisher AG, Evans KG, Nelems B, Finley RJ. Effect of routine fibrin glue use on the duration of air leaks after lobectomy. Ann Thorac Surg. 1990;49:133–4.
Wong K, Goldstraw P. Effect of fibrin glue in the reduction of postthoracotomy alveolar air leak. Ann Thorac Surg. 1997;64:979–81.
McCarthy PM, Trastek VF, Bell DG, Buttermann GR, Piehler JM, Payne WS, et al. The effectiveness of fibrin glue sealant for reducing experimental pulmonary air leak. Ann Thorac Surg. 1988;45:203–5.
Fabian T, Federico JA, Ponn RB. Fibrin glue in pulmonary resection: a prospective, randomized, blinded study. Ann Thorac Surg. 2003;75:1587–92.
Matar AF, Hill JG, Duncan W, Orfanakis N, Law I. Use of biological glue to control pulmonary air leaks. Thorax. 1990;45:670–4.
Itano H. The optimal technique for combined application of fibrin sealant and bioabsorbable felt against alveolar air leakage. Eur J Cardiothorac Surg. 2008;33:457–60.
Pedersen TB, Honge JL, Pilegaard HK, Hasenkam JM. Comparative study of lung sealants in a porcine ex vivo model. Ann Thorac Surg. 2012;94:234–40.
Gika M, Kawamura M, Izumi Y, Kobayashi K. The short-term efficacy of fibrin glue combined with absorptive sheet material in visceral pleural defect repair. Interact Cardiovasc Thorac Surg. 2007;6:12–5.
Kawai H, Harada K, Ohta H, Tokushima T, Oka S. Prevention of alveolar air leakage after video-assisted thoracic surgery: comparison of the efficacy of methods involving the use of fibrin glue. Thorac Cardiovasc Surg. 2012;60:351–5.
Albes JM, Krettek C, Hausen B, Rohde R, Haverich A, Borst HG. Biophysical properties of the gelatin-resorcin-formaldehyde/glutaraldehyde adhesive. Ann Thorac Surg. 1993;56:910–5.
Hirokawa F, Hayashi M, Miyamoto Y, Iwamoto M, Tsunematsu I, Asakuma M, et al. A novel method using the VIO soft-coagulation system for liver resection. Surgery. 2011;149:438–44.
Sakuragi T, Ohma H, Ohteki H. Efficacy of SOFT COAG for intraoperative bleeding in thoracic surgery. Interact Cardiovasc Thorac Surg. 2009;9:767–8.
Uchiyama A, Miyoshi K, Nakamura K. VIO soft-coagulation system for major pulmonary resections: results in 68 patients with primary lung cancer. Gen Thorac Cardiovasc Surg. 2011;59:175–8.
Toyazaki T, Tomioka Y, Chiba N, Ueda Y, Sakaguchi Y, Gotoh M, et al. Thoracoscopic partial resection without using a stapler (complete republication). Gen Thorac Cardiovasc Surg. 2017;65:449–54.
Ikegami T, Maeda T, Kayashima H, Oki E, Yoshizumi T, Sakaguchi Y, et al. Soft coagulation, polyglycolic acid felt, and fibrin glue for prevention of pancreatic fistula after distal pancreatectomy. Surg Today. 2011;41:1224–7.
Porte HL, Jany T, Akkad R, Conti M, Gillet PA, Guidat A, et al. Randomized controlled trial of a synthetic sealant for preventing alveolar air leaks after lobectomy. Ann Thorac Surg. 2001;71:1618–22.
Wain JC, Kaiser LR, Johnstone DW, Yang SC, Wright CD, Friedberg JS, et al. Trial of a novel synthetic sealant in preventing air leaks after lung resection. Ann Thorac Surg. 2001;71:1623–8. (discussion 28–9).
Ikeda T, Sasaki M, Yamada N, Takamori A, Tanabe S, Okada A, et al. Controlling air leaks using free pericardial fat pads as surgical sealant in pulmonary resection. Ann Thorac Surg. 2015;99:1170–5.
Shintani Y, Inoue M, Funaki S, Kawamura T, Minami M, Okumura M. Clinical usefulness of free subcutaneous fat pad for reduction of intraoperative air leakage during thoracoscopic pulmonary resection in lung cancer cases. Surg Endosc. 2015;29:2910–3.
Murakami J, Ueda K, Tanaka T, Kobayashi T, Kunihiro Y, Hamano K. The validation of a no-drain policy after thoracoscopic major lung resection. Ann Thorac Surg. 2017;104:1005–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Thoracic and Cardiovascular Surgery unit at Nara Medical University has no financial interest in the materials or methods used, nor any financial relationship with any of the manufacturers mentioned in this report. The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kawai, N., Kawaguchi, T., Suzuki, S. et al. Low-voltage coagulation, polyglycolic acid sheets, and fibrin glue to control air leaks in lung surgery. Gen Thorac Cardiovasc Surg 65, 705–709 (2017). https://doi.org/10.1007/s11748-017-0829-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-017-0829-2