Abstract
Background
The aim of this study was to evaluate the accuracy of [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography, ultrasonography, and enhanced computed tomography alone in the preoperative diagnosis of lymph node metastasis in patients with papillary thyroid carcinoma.
Methods
In a prospective study performed between January 2007 and December 2009, 74 patients with a diagnosis of papillary thyroid carcinoma confirmed by fine-needle aspiration biopsy were referred to our institution for surgery. Preoperative assessment of metastasis in the central and lateral cervical lymph nodes was done using [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography, ultrasonography, and enhanced computed tomography. The results for each level of cervical node assessed using these methods were correlated with the pathology reports after surgery. We determined the sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of the three methods for all levels of cervical lymph node.
Results
There were no significant differences in the diagnostic results obtained by [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography and enhanced computed tomography. However, ultrasonography images gave significantly better results than either [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography or enhanced computed tomography alone in identifying metastases on the basis of the level of cervical lymph node. In addition, the overall diagnostic accuracy tended to be higher for the lateral compartment than for the central compartment.
Conclusions
Preoperative assessment by ultrasonography of metastases in the central and lateral cervical lymph nodes might be the best methodology for determining the extent of surgical resection required to remove metastatic lymph nodes adequately in patients with papillary thyroid carcinoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is an endocrine neoplasm with a high incidence of lymphatic metastasis. Metastasis to cervical lymph nodes occurs in 35–80% of patients [1, 2]. The metastatic spread of PTC to the neck does not seem to affect overall or disease-specific survival; however, it does increase the risk of local or regional recurrence of the tumor and the need for further surgery [3, 4]. The extent of surgical resection required for the adequate removal of metastatic lymph nodes is controversial. There is a high frequency of occult metastases to the central lymph nodes (level VI; the prelaryngeal, pretracheal, and paratracheal nodes); hence, the elective dissection of these nodes at the same time as total thyroidectomy is recommended for high-risk patients. For the other cervical lymph nodes (levels I–V), some surgeons advocate simple limited lymphadenectomy, known as “berry picking” [5]. This approach has been discontinued because of the high rate of recurrence of the tumor in the neck and the morbidity associated with multiple surgeries, which often involves recurrent laryngeal nerve paralysis and hypoparathyroidism. Other surgeons recommend a modified radical neck dissection, preserving the internal jugular vein, the spinal accessory nerve, and the sternocleidomastoid muscle [6]. However, there are few data to support the use of this procedure for the treatment of metastases in lateral cervical lymph nodes in PTC. Disease-specific or disease-free survival in patients without evidence of macroscopic disease has not been shown to be improved by modified radical neck dissection. Therefore, current recommendations include the removal of all clinically involved metastatic lymph nodes in the central and lateral compartments, as determined by preoperative radiological investigations using, for example, ultrasonography (US), enhanced computed tomography (CT), and magnetic resonance imaging (MRI) [7]. A recent report has suggested that the evaluation of metastatic lymph nodes by US can be used to identify effectively the extent of surgical resection required [8].
Whole-body positron emission tomography (PET) using [18F]-fluoro-2-deoxy-d-glucose (18FDG) has recently emerged as a useful tool for the detection of primary tumors and metastases in a variety of cancers [9, 10]. Many reports state that 18FDG-PET/CT adequately detects recurrent disease during the follow-up of PTC patients who have undergone thyroidectomy, have shown negative diagnostic iodine-131 (131I) scans, and have abnormal serum thyroglobulin levels [11]. Several studies also reported that 18FDG-PET/CT can be useful for the preoperative evaluation of cervical nodes in patients with head and neck cancer [9, 12, 13]. However, few studies have documented the diagnostic accuracy of 18FDG-PET/CT in the initial evaluation of the involvement of cervical nodes in patients with PTC [14]. In the current study, we compared the diagnostic accuracy of 18FDG-PET/CT, US, and enhanced CT alone in the initial preoperative evaluation of cervical lymph node metastases in patients with PTC.
Materials and methods
Patients and study design
All patients provided informed consent for examination and treatment, and the protocol was approved by our institutional review board. This prospective study was carried out between January 2007 and December 2009 on 74 patients who were referred to our institution for surgery with a diagnosis of PTC confirmed by fine-needle aspiration (FNA) biopsy. The patients included 62 women and 12 men, with an age range of 16–84 years and a mean age of 65.6 years. Preoperative assessments were made of metastases in the central and lateral cervical lymph nodes by 18FDG-PET/CT, high-resolution US, and enhanced CT. The node locations were classified by the operating surgeon using the system proposed by the American Head and Neck Society, and the American Academy of Otolaryngology-Head and Neck Surgery [15]. All patients subsequently underwent total or subtotal thyroidectomy and cervical lymph node dissection based on the preoperative evaluation of the presence of lymph node metastasis.
US
The evaluation of lymph nodes by US was performed by a surgeon using a high-resolution instrument (Nemio SSA-550A; Toshiba Medical Systems, Japan) equipped with a high-frequency linear-array 12-MHz transducer. The lymph nodes were characterized as highly suggestive of metastasis on the basis of any one of the following criteria: a minor axis diameter greater than 10 mm, a minor axis diameter greater than 50% of the major axis diameter, or hyperechogenicity with or without microcalcification. The area scanned included the central compartment medial to the carotid artery, the entire length of the bilateral internal jugular chain from the mandible to the head of the clavicle, and the posterior lymph node groups along the course of the spinal accessory nerve.
Enhanced CT scanning
Enhanced CT scans of the neck were performed using a standard LightSpeed VCT scanner (GE Healthcare, Milwaukee, WI) with the following parameters: 30–200 mAs, 120 keV, a section width of 5 mm, and a table feed of 5 mm per rotation. For contrast enhancement, 60 ml of the iodinated contrast medium Iohexol 300 (Fuji Pharma Co., Tokyo, Japan) was injected intravenously at 2.0 ml/s using an automated injector and a scan delay time of 30 s. Lymph nodes were characterized as highly suggestive of metastasis on the basis of any of the following criteria: a long axis diameter greater than 10 mm, a lymph node with a focal translucency suggestive of necrosis, marginal enhancement, or focal calcification.
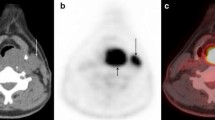
18FDG-PET/CT
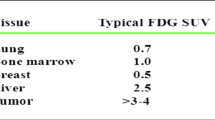
All patients fasted for at least 5 h prior to the PET study. PET/CT scans were performed using a GE Discovery ST Elite scanner (GE Healthcare) with the following parameters: 30–200 mAs, 120 keV, a section width of 5 mm, and a table feed of 5 mm per rotation. No intravenous or oral contrast agents were used. After the CT scan, an emission scan was performed from the thigh to the head for 5 min per frame for a total of 45 min after the intravenous injection of 200–300 MBq FDG. The attenuation-corrected PET images using the CT data were reconstructed using an ordered subset expectation-maximization algorithm. The standardized uptake values (SUVs) were adjusted using the attenuation-corrected images, the amount of injected FDG, the body weight of each patient, and the cross-calibration factors between the PET and the dose calibrator. The PET/CT scans were interpreted by a nuclear medicine radiologist and scored as positive or negative for residual cervical metastatic disease. The radiologist was unaware of each patient’s clinical status. Lesions showing FDG uptake were graded on a scale of 0–4 (0, definitely benign; 1, probably benign; 2, equivocal; 3, probably malignant; and 4, definitely malignant). Only lymph nodes with lesions scoring 3 or 4 were considered positive for metastases.
Surgical procedures
After assessing metastases in the cervical lymph nodes, all patients underwent total or subtotal thyroidectomy and central compartment (level VI) neck dissection. If metastases were detected in the lateral compartment of the neck by preoperative radiological investigations, patients underwent a modified radical neck dissection that included level II–V lymph nodes with preservation of the internal jugular vein, sternocleidomastoid muscle, and spinal accessory nerve as far as possible. The removed cervical lymph nodes were divided according to level in the operating room by the same surgeon.
Statistical analysis
We determined the sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of 18FDG-PET/CT, US, and enhanced CT for cervical lymph nodes from different levels. The status of each node established preoperatively was correlated with the pathological reports, which confirmed the presence or absence of metastases. Sensitivity was defined as the number of true-positive cases divided by the sum of true-positive and false-negative cases. Specificity was defined as the number of true-negative cases divided by the sum of true-negative and false-positive cases. Positive predictive value was defined as the number of true-positive cases divided by the sum of true-positive and false-positive cases. Negative predictive value was defined as the number of true-negative cases divided by the sum of true-negative and false-negative cases. Diagnostic accuracy was defined as the sum of true-positive and true-negative cases divided by the total number of cases. Statistical analyses were done using SPSS software v2.0 (SPSS, Inc., Chicago, IL). Statistical differences were analyzed using the Mann–Whitney test. A two-tailed p < 0.05 was considered significant.
Results
In this study we focused on classifying lymph nodes by level, rather than by individual node, because the presence of malignant tissues at each lymph node level affects the extent of treatment. Lymph nodes from the 74 patients who underwent cervical lymph node dissection were examined pathologically in a total of 349 groups, according to cervical level. Of these groups, 148 were from the central compartment and 201 were from the lateral compartment. The groups of lymph nodes pathologically confirmed to contain metastases are summarized in Table 1.
Figure 1 shows the results of using the three different diagnostic imaging methods to evaluate all cervical lymph nodes, analyzed by level (levels II–VI), compared with the pathological findings. Metastases were identified in 111 of the groups of cervical lymph nodes examined. There were no significant differences in the diagnostic results obtained by 18FDG-PET/CT and enhanced CT. However the US images showed significantly better agreement with the pathological results than either 18FDG-PET/CT or enhanced CT alone, with the exception of the negative predictive value.
Comparison of diagnostic results for 18FDG-PET/CT, enhanced CT, and US in evaluation of all cervical nodes (levels II–VI). The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy for 18FDG-PET/CT were 29.7, 93.3, 67.3, 74.0, and 73.1%, respectively; those for enhanced CT were 22.5, 94.1, 64.1, 72.3, and 71.3%, respectively; and those for US were 71.2, 97.1, 91.9, 87.8, and 88.8%, respectively
The results focusing on only the lymph nodes in the central compartment are summarized in Fig. 2. Metastases were identified in 66 of the groups of cervical lymph nodes. In the central compartment, the diagnostic results significantly differed among 18FDG-PET/CT, US, and enhanced CT only with respect to sensitivity and diagnostic accuracy.
Comparison of diagnostic results for 18FDG-PET/CT, enhanced CT, and US in evaluation of central cervical nodes (level VI). The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy for 18FDG-PET/CT were 22.7, 98.8, 93.8, 61.4, and 64.9%, respectively; those for enhanced CT were 15.1, 98.8, 90.9, 59.1, and 61.5%, respectively; and those for US were 63.6, 97.6, 95.5, 76.9, and 82.0%, respectively
The results focusing on only the lymph nodes from the lateral compartment (levels II–V) are summarized in Fig. 3. Metastases were identified in 45 groups of lymph nodes at these levels. The diagnostic results from all three imaging techniques were in better agreement with the pathological results for the lateral compartment than for the central compartment. For all five diagnostic indicators, the US images gave significantly better results than 18FDG-PET/CT and enhanced CT alone.
Comparison of diagnostic results for 18FDG-PET/CT, enhanced CT, and US in evaluation of lateral cervical nodes (levels II–V). The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy for 18FDG-PET/CT were 40.0, 90.4, 54.5, 83.9, and 79.1%, respectively; those for enhanced CT were 33.3, 91.7, 53.6, 82.7, and 78.6%, respectively; and those for US were 82.2, 96.8, 88.1, 95.0, and 94.0%, respectively
Discussion
PTC carries a high risk of cervical lymph node metastasis. Most commonly, a central compartment neck dissection is performed at the same time as thyroidectomy, with or without lateral compartment dissection [16]. However, the management of lateral neck metastasis remains controversial. A modified lateral neck dissection has not been shown to improve disease-specific or disease-free survival in patients with no evidence of lateral lymph node metastases [3, 4]; by contrast, it has been reported to improve survival in patients with clinical evidence of lateral lymph node metastases [17]. Thus, imaging the neck before surgery for thyroid carcinoma is necessary to determine the appropriate extent of surgical resection.
The preoperative radiological investigations commonly used are US, enhanced CT, and MRI. In particular, the evaluation of metastatic lymph nodes by US has recently been reported to be effective for assessing the extent of surgical resection required [8]. At present, US imaging is used to predict the malignancy of thyroid nodules, and US-guided FNA can be used to obtain samples for cytological diagnosis on initial presentation of patients [18]. At the same time, US examination of the neck is easy and inexpensive. 18FDG-PET/CT has recently been shown to be a remarkable tool for detecting primary tumors and metastases in a variety of cancers [9, 10]. However, its diagnostic accuracy in the initial evaluation of cervical lymph nodes at different levels in patients with PTC has not been documented [14].
This prospective study focused on PTC and compared the diagnostic accuracy of an initial evaluation of the level of cervical lymph nodes involved using 18FDG-PET/CT, US, and enhanced CT alone. The US images gave significantly better results than either 18FDG-PET/CT or enhanced CT alone for the detection of cervical lymph node metastasis in the total neck compartment. However, the overall diagnostic accuracy of all three methodologies tended to be lower for lymph nodes of the central compartment than for those of the lateral compartment. In addition, the negative predictive values were lower for the central compartment. This confirms that central compartment neck dissection should be performed with thyroidectomy regardless of whether suspicious lymph node metastases are found in preoperative radiological investigations. The poorer diagnostic accuracy for the central compartment lymph nodes could result from the anatomical complexity of the thoracic inlet and the difficulty in interpreting images of individual lymph nodes.
Our finding that the overall diagnostic accuracy of all methodologies was higher for the lateral than for the central compartment was similar to those of previous studies [14, 19, 20]. In addition, the US images showed significantly better results than 18FDG-PET/CT or enhanced CT alone for the detection of cervical lymph node metastases in the lateral compartment. Performing a modified lateral neck dissection in patients with clinical evidence of lateral lymph node metastases has been reported to improve survival [17]. Therefore, a modified radical neck dissection should be performed in patients in whom just one lymph node metastasis is detected by US in cervical levels II–V. However, observations such as the low incidence of nodal metastasis at levels I and V [21] and the low incidence of “skip” metastasis [6] have caused controversy about the extent of lateral neck dissection that should be carried out at thyroidectomy. The incidence of metastasis in level IIb lymph nodes has been reported to be low if level IIa nodes are not involved, in which case level IIb node dissection is probably unnecessary [6].
When cervical node dissection above the spinal accessory nerve is performed, there is a possibility of shoulder disability and pain from damage to the nerve, even if it is preserved during surgery. However, the shoulder pain and disability after surgery are temporary [22].
In our study, 25 patients underwent a modified radical neck dissection that included levels II–V cervical lymph nodes because metastases had been detected by US in cervical lymph nodes in the lateral neck compartment. For the level IIb lymph nodes, three of the five cases were false negatives, as were four of the nine cases for level V nodes. Our results showed that the false negatives initially identified by US tended to be at high cervical lymph node levels. Thus, a modified radical neck dissection that includes levels II–V lymph nodes should be performed when metastasis in the lateral cervical lymph nodes is detected by US.
Although the relatively small number of subjects in our study limited our conclusions to some extent, our results showed that 18FDG-PET/CT did not provide any additional benefit over either US or enhanced CT in the initial evaluation of cervical lymph nodes in patients with PTC. The ability of 18FDG-PET/CT to visualize tumors is based on the increased carbohydrate metabolism in malignant cells, which results in elevated glucose utilization and selective 18FDG uptake by these cells. After phosphorylation by hexokinase, 18FDG accumulates intracellularly as it cannot be metabolized as glucose. Well-differentiated thyroid carcinomas that show adequate uptake of 131I are associated with a reduced glucose metabolism [11]. Lymphatic metastases, as well as the primary tumor, are relatively slow growing and have relatively low levels of glucose metabolism. By contrast, dedifferentiated tumors that do not accumulate 131I show an elevated level of glucose utilization. Therefore, 18FDG-PET/CT is considered a worthwhile method for assessing recurrent or residual PTC but not for evaluating the initial primary tumor and cervical lymph node metastases [11, 14]. In recurrent disease, imaging using 131I is often negative and responses to 131I ablative therapies can be poor; 18FDG-PET/CT might be useful in predicting the response to such treatments.
In conclusion, our results showed that US provided significantly better results than 18FDG-PET/CT and enhanced CT alone for the detection of cervical lymph node metastasis in the total neck compartment in patients with PTC. In addition, the overall diagnostic accuracy tended to be higher for the lateral compartment than for the central compartment. Preoperative assessment of central and lateral cervical lymph node metastases by US might be used to determine the extent of surgical resection needed to remove metastatic lymph nodes in these patients. A central compartment neck dissection should be performed with thyroidectomy because the negative predictive values were lower for the central compartment than for the lateral compartment. Moreover, the false-negative rate for US images tended to be high for cervical lymph node levels IIb and V. Thus, a modified radical neck dissection that includes levels II–V should be performed when metastases are detected by US in the lateral cervical lymph node compartment.
References
Gilliland FD, Hunt WC, Morris DM et al (1997) Prognostic factors for thyroid carcinoma: a population-based study of 15, 698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973–1991. Cancer 79:564–573
Clark OH (1996) Predictors of thyroid tumor aggressiveness. West J Med 165:131–138
Grebe SK, Hay ID (1996) Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 5:43–63
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 86:1447–1463
Noguchi S, Murakami N (1987) The value of lymph-node dissection in patients with differentiated thyroid cancer. Surg Clin North Am 24:325–330
Lee BJ, Wang SG, Lee JC et al (2007) Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 133:1028–1030
Cooper DS, Doherty GM, Haugen BR et al (2006) American Thyroid Association Guidelines Taskforce. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–142
Langer JE, Mandel SJ (2008) Sonographic imaging of cervical lymph nodes in patients with thyroid cancer. Neuroimaging Clin N Am 18:479–489
McGuirt WF, Williams DW 3rd, Keyes JW Jr et al (1995) A comparative diagnostic study of head and neck nodal metastases using positron emission tomography. Laryngoscope 105:373–375
Bochuslavitzki KH, Klutmann S, Kröger S et al (2000) FDG PET detection of unknown primary tumors. J Nucl Med 41:816–822
Frilling A, Tecklenborg K, Gorges R et al (2001) Preoperative diagnostic value of 18fluorodeoxyglucose positron emission tomography in patients with radioiodine-negative recurrent well-differentiated thyroid carcinoma. Ann Surg 234:804–811
Stokkel MP, ten Broek FW, Hordijk GJ et al (2000) Postoperative evaluation of patients with primary head and neck cancer using dual-head 18fluoro-deoxyglucose positron emission tomography. Ann Surg 231:229–234
Jeong HS, Baek CH, Son YI et al (2007) Use of integrated 18F-FDG PET/CT to improve the accuracy of initial cervical nodal evaluation in patients with head and neck squamous cell carcinoma. Head Neck 29:203–210
Jeong HS, Baek CH, Son YI et al (2006) Integrated 18F-FDG PET/CT for the initial evaluation of cervical node level of patients with papillary thyroid carcinoma: comparison with ultrasound and contrast-enhanced CT. Clin Endocrinol (Oxf) 65:402–407
Robbins KT, Clayman G, Lavine PA et al (2002) Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg 128:751–758
Bhattacharyya N (2003) Surgical treatment of cervical nodal metastases in patients with papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 129:1101–1104
Noguchi S, Murakami N, Yamashita H (1998) Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg 133:276–280
Fish SA, Langer JE, Mandel SJ (2008) Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am 37:401–417
Ahn JE, Lee JH, Yi JS et al (2008) Diagnostic accuracy of CT and ultrasonography for evaluating metastatic cervical lymph nodes in patients with thyroid cancer. World J Surg 32:1552–1558
Kouvaraki MA, Shapiro SE, Fornage BD et al (2003) Role of preoperative ultrasonography in surgical management of patients with thyroid cancer. Surgery 134:946–954; discussion 954–955
Caron NR, Tan YY, Ogilvie JB et al (2006) Selective modified radical neck dissection for papillary thyroid cancer-is level I, II and V dissection always necessary? World J Surg 30:833–840
Köybasioglu A, Tokcaer AB, Uslu S et al (2000) Accessory nerve function after modified radical and lateral neck dissection. Laryngoscope 110:73–77
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morita, S., Mizoguchi, K., Suzuki, M. et al. The Accuracy of 18[F]-Fluoro-2-Deoxy-d-Glucose-Positron Emission Tomography/Computed Tomography, Ultrasonography, and Enhanced Computed Tomography Alone in the Preoperative Diagnosis of Cervical Lymph Node Metastasis in Patients with Papillary Thyroid Carcinoma. World J Surg 34, 2564–2569 (2010). https://doi.org/10.1007/s00268-010-0733-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0733-8