Abstract
Background
Although the Nuss procedure has been widely adopted as a standard procedure in children with pectus excavatum, reports focusing on its use in adults are rare. We retrospectively reviewed postoperative results to evaluate the safety and efficacy of the Nuss procedure in late adolescents and adults with pectus excavatum.
Methods
Between 2004 and 2007, a total of 44 patients (M:F = 38:6) with a median age of 20 underwent the Nuss procedure. The pectus bar was inserted under thoracoscopic guidance and the depressed sternum was lifted by means of a crane device before rotating the bar. The bar was secured with steel wires laterally at three points. A compound bar and sometimes double bar insertion was performed.
Results
The median length of hospital stay was three days. Complications occurred in nine patients, including pneumothorax in five, bar rotation in two, wound infection in two, and pericardial effusion in one. Reoperation was performed in three patients to correct bar rotation (n = 2) and incomplete repair (n = 1). Three of the 26 patients with a single bar required reoperation, whereas none of the 18 with a double bar had a second operation. There was no recurrence of the chest deformity over median follow-up of 12 months, except in one patient from whom the bar was removed prematurely.
Conclusions
Using the thoracoscope, the compound bar technique, the 3-point wire fixation, the crane technique, and sometimes double bar insertion showed that the Nuss procedure could be performed safety and effectively in late adolescent and adult patients with pectus excavatum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pectus excavatum is the most common congenital chest wall deformity in children [1]. In 1998 Nuss and associates presented a novel minimally invasive method for correction of a funnel chest [2]. The procedure is based on substernal insertion of an appropriately shaped metal bar that elevates the sternum. The Nuss procedure is widely accepted as a standard minimally invasive technique in prepubertal and early pubertal patients [1, 3]. Many studies have documented the excellent results of the Nuss procedure in children [1–3].
In adults, the modified Ravitch procedure can be performed with low morbidity, short hospital stay, and considerable improvement in physical function [4–6]. However, the Ravitch operation requires bilateral costal cartilage resection and sternal osteotomy and is more invasive than the Nuss procedure. The Nuss procedure in adult patients, whose chest wall is less compliant, is more difficult than in children. Its use in adult patients continues to be debated. Since Coln and colleagues first reported encouraging results for the Nuss procedure in adults, there have been additional reports of its use for pectus excavatum in adolescents and adults [7–14].
We have been performing the Nuss procedure since 1999 and have modified our technique in late adolescent and adult patients since 2004. Here we present the operative results of the modified Nuss procedure in late adolescent and adult patients with pectus excavatum, and evaluate the safety and efficacy of this procedure in this group of patients.
Patients and methods
We retrospectively reviewed late adolescent and adult patients (older than 15 years of age) who underwent correction of a pectus excavatum by the Nuss procedure between January 2004 and September 2007. We analyzed the clinical characteristics, computed tomography (CT) findings, operative data, and postoperative complications and outcomes.
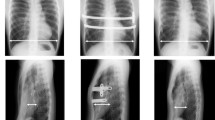
With the accumulation of experience in older patients, we modified our techniques. However, in all cases a thoracoscope was used. We designed a small central arc between each hinge-point and both lateral ends of the bar to fit the chest wall, the so called compound bar shape molding [3]. We always narrowed the intercostal space where the bar is inserted. Two wires encircle the rib above and below at the lateral edge of the hinge point. We twist the wire once to narrow the intercostal space into which the bar is inserted and then encircle and twist with the rotated bar (Fig. 1). We usually use a three-point wire fixation. Steel wires are added at the right end or at both ends of the bar. We elevate the sternum during the procedure, the so called Crane technique. Sometimes double bars are inserted at the superior and inferior levels parallel to each other.
Patients were placed in the supine position with both arms and shoulders abducted to expose the anterior and lateral chest wall. The deepest point and the bilateral highest points (thoracic entry and exit points) of the thorax bilaterally were marked. These were used to set the horizontal plane for the bar placement. Through small bilateral incisions at each of the anterior midaxillary lines at the level of the deepest chest wall depression, submuscular pockets were made by blunt dissection. A 30-degree thoracoscope (Karl Storz, 5-mm wide-angle optic thoracoscope) was placed through a 5 mm trocar inserted two intercostal spaces below the lateral thoracic skin incision. With thoracoscopic visualization, the pleura was punctured at the previously marked highest point of the funnel chest. Then each of the #5 wires (surgical steel, Ethicon, 40 mm 1/2c 50 metric, tapecut) were sutured through the upper and lower ribs nearly lateral to the punctured intercostal space on both sides. After the #5 wire was sutured onto the sternum of the anterior chest wall, we elevated the sternum by pulling the wire up with the Kent retractor (Jakasago, Tokyo, Japan) (Fig. 2). With right-side thoracoscopic visualization, a long curved Kelly clamp was inserted into the thorax and passed retrosternally through the chest to the contralateral side. It exited through the left highest chest wall marking under left side thoracoscopic guidance. Measurements were taken from the patient’s chest at the midaxillary line to the opposite midaxillary line with the aluminum bar sizer. The bar was bent to fit the patient’s chest shape with a Zimmer bar bender, after which it was inserted with the convexity facing posteriorly. After twisting once with the previously sutured wires that were located at both lateral positions of the hinge point, a bar flipper was used to turn it over while pulling up the sternum. The rotated bar was fixed by encircling and twisting the wires, which were previously twisted once, with it (Fig. 1). A #5 Steel wire was sutured with each of the above or below ribs at the right end or, sometimes, both lateral ends of the bar. After withdrawing the thoracoscope, the thoracoscopic port incisions were extended to small bilateral incisions at each of the anterior midaxillary lines. Submuscular pockets were made by blunt dissection. A 30-degree thoracoscope was placed through a 5-mm trocar inserted two intercostals spaces below the lateral thoracic skin incision. Then one more bar insertion procedure was performed in the same manner. After withdrawing the thoracoscope, two 20-French chest tubes were placed through each 5-mm port site. The lung was fully expanded and positive end-expiratory pressure was applied until the incisions were closed. The chest tubes were used to aspirate any residual air within the pleural cavity and were removed once all skin incisions were closed. If air leaks occurred, the chest tube was maintained until no air leakage was present. A chest x-ray was obtained in the post-anesthesia care unit.
All the patients were regularly followed postoperatively. In cases that were lost to follow-up, a telephone interview was conducted to obtain the late postoperative outcomes. Descriptive statistics were used to describe the patient characteristics and outcomes. Normally distributed continuous data were expressed as the median and range. Categorical data were expressed as counts and proportions. Student t-tests and chi square tests were used to compare the continuous and categorical variables, respectively. Significance was accepted at p values less than 0.05.
Results
Patient profile
A total of 199 Nuss procedures were performed in our department between January 2004 and September 2007. The number of late adolescent and adult patients (older than 15 years of age) among them was 44 (22.1%). There were 38 men and 6 women with a median age of 20 years (range: 15–32 years). The number of Nuss procedures performed in these 44 patients totaled 47 (25%), including three reoperations. The morphology of the pectus was 27 symmetric types (61.4%) and 17 asymmetric types (38.6%). The preoperative symptoms included dyspnea on exertion in six patients (13.6%), anterior chest wall pain in three (6.8%), and easy fatigue in one (2.2%). Most of the patients (81.8%) had no symptoms (Table 1). Most patients wanted a better chest contour for cosmetic reasons. Two patients had a history of sternal surgery. One patient who had a recurrence of the deformity after a sternal turnover operation at the age of 15 underwent minimally invasive repair for the pectus excavatum at age 18. Another patient, who had undergone mitral valve repair at age 4, underwent successful minimally invasive repair for a pectus excavatum at age 23.
The median operating time was 90 min (range: 50–160 min). The median hospital stay for all patients was 3 days (range: 3–4 days). In every case, we fixed the bar with steel wires, and the bar was always inserted under thoracoscopic guidance. The compound bar technique was used in all cases. A single bar was inserted in 26 patients (63.8%), and double bars in 18 patients (36.2%). The Crane technique (19 patients, 43.1%) has been used since November 2004, and it has been applied to all patients since May 2006 (Table 2).
Complications occurred in 9 patients (20.4%). Minor complications included a pneumothorax in 5 patients (10.6%), pleural effusion in 1 patient (2.2%), and a wound infection that required surgical revision in 2 patients (4.5%). Major complications that required reoperation occurred in 3 patients, incomplete correction of the pectus excavatum, pericardial effusion, and wound infection occurred in 1 (2.2%), and bar rotation occurred in 2 (4.5%) (Table 3). A single bar was inserted in one patient with asymmetric morphology; 14 months later one more pectus bar was inserted because of incomplete correction. After reoperation, bar rotation occurred; in addition the patient developed a pericardial effusion, constrictive pericarditis, and wound infection. Therefore, we repositioned the rotated bar. However, the bars had to be removed because of an ongoing pericardial effusion and constrictive pericarditis. As mentioned above, one patient underwent bar reinsertion to obtain a better chest wall shape, and the other two patients had bar repositioning to correct bar rotation. Three patients of 26 with a single pectus bar required reoperation; however, none of the patients among the 18 with initially inserted double bars required reoperation. The bars have been removed in 22 patients (50%) without any complications.
The median follow-up period after bar insertion was 34.1 months (range: 14.3–59.8 months). The median bar indwelling period was 31.1 months (range: 2.5–41.8 months). The median follow-up after bar removal was 12 months (range: 0.7–29.3 months). There have been no recurrences of the pectus excavatum, except in one patient with multiple complications whose bars had to be removed prematurely.
Conclusions
Most patients with pectus excavatum have a chest wall deformity without any clinical symptoms. At puberty, symptoms can develop as physical activity increases, or with worsening of the pectus during the second growth spurt and decreasing chest wall elasticity [6, 15]. Repair of pectus excavatum in adult patients whose chest wall is less compliant is more difficult than during childhood. Dzielicki and colleagues reported that additional procedures are required to achieve a complete correction of the deformity in patients over 15 years of age with a more rigid chest or with an asymmetric deformity [1]. The chest wall of patients between 15 and 18 year of age might be as rigid as that of patients over 18 years of age. Therefore, we defined patients as late adolescent and adult if they were 15 years or older, a group of patients who require modified minimally invasive techniques. We have performed a modified Nuss procedure in late adolescent and adult patients since 2004.
Although surgical repair of this deformity in adults is more difficult, open repair has been widely used. Fonkalsrud and colleagues successfully repaired pectus excavatum in 104 adults, by costochodrectomy, sternal osteotomy, and strut stabilization [4]. This repair can be performed in adults with low morbidity, short hospital stay, and considerable improvement in physical function [4–6]. The open repair procedures are, however, more invasive than the Nuss procedure. Coln and colleagues were the first to report encouraging results of minimally invasive repair in adulthood [9]. Subsequently, there have been several reported series in the literature using the Nuss procedure for repair of pectus excavatum in adolescent and adult patients [7–10]. Nonetheless, the application of minimally invasive repair in adults continues to be debated.
Some reports state that minimally invasive repair is as effective for correcting pectus excavatum in adults as in children [8–12]. However, in adults the bar tends to be less stable, and wound abscess formation occurs more frequently [8]. Kim et al. described their experience with 24 adolescents and adults, showing a significantly longer operating time and an increased complication rate compared to children. Their frequency of complications was 58.3%; they concluded that minimally invasive repair could not be advocated as the treatment of choice in adults [7].
We used a 5-mm thoracoscope in all patients to control the wiring needle, and the long curved Kelly clamp passing through the substernal mediastinum [1]. We had five pneumothoraces. In only one case among them, the air leak had extended the hospital stay to four days. Perhaps visualization of the wiring and passing the long curved Kelly clamp and bar through the mediastinum minimizes injury to the lungs. None of the patients developed a postoperative hemothorax on screening for bleeding at the wound site by thoracoscopic visualization.
We have designed a small central arc in the bar, between each hinge point and both lateral ends to fit the chest wall, referred to as the compound bar technique [3]. As a result, the bar can bear a heavier load on the chest wall. It is important that the lateral ends of the bar fit into the rib cage. If they do not, the dead space of the submuscular pocket will have to be maintained. This tends to cause a seroma, wound infections, or bar rotation.
Double bars are inserted at the superior and inferior levels parallel to each other. This technique decreases the risk of bar rotation by dispersing the pressure loaded onto the bars [2, 3]. We have no hesitation in inserting double bars. We have used double bar insertion when a single bar is not satisfactory for the correction of the deformity or when the chest wall deformity is very severe. We have commonly inserted double bars since February 2006. In addition, we used double bar insertion in late adolescent and adult patients that had instability with one bar fixation or had a severe deformity. The percentage of double bar insertions was 36.2%. However, 80% of the adult patients have had double bars inserted since February 2006. Although there is no statistically significant effect to date (P = 0.526), three of 26 patients with a single bar required reoperation, whereas none of the 18 patients with double bars underwent reoperation. The double bar insertion might be more stable and safer in late adolescent and adult patients with a severe pectus excavatum.
We have applied three-point, or sometimes more, wire fixation to narrow the intercostal space where the bar is inserted. To accomplish the narrowing, we twist each wire once before rotating the bar (Fig. 1). This technique prevents the bar from lacerating the intercostal muscles and from migration during rotation of the bar. We usually wire the right end and both nearby hinge points of the inserted bar, which is enough to prevent hinge point disruption, migration, of the bar, and rotation of the bar. This technique may be less costly and more effective than that using stabilizer in late adolescent and adult patients.
We usually elevated the sternum while inserting and rotating the bar, the so-called Crane technique [2]. This technique minimizes mediastinal injury while passing and rotating the bar through the mediastinum by increasing the anterior mediastinal space. In addition, intercostal muscle laceration and rotation of the bar during rotation and fixation of the bar is reduced by decreasing the elastic recoil of the rib cage (Fig. 2).
Our results demonstrate that the pectus excavatum was successfully corrected with a modified minimally invasive technique in late adolescent and adult patients; there were relatively few complications, a short hospital stay, and the patients were satisfied with the result. Our complication rate was 20.4%, lower than the complication rates reported by other studies [7, 10]. A pneumothorax occurred in only five patients; only two patients required a tube thoracotomy and this lengthened the hospital stay to four days in only one patient. The routine use of thoracoscopic visualization might have reduced the frequency of lung injury.
There was no recurrence of the chest deformity with a median follow-up of 12 months, except in one patient whose bars were removed early because of persistent pericardial effusion and wound infection.
We would not hesitate to perform the Nuss operation in patients that have had open heart surgery or a sternal turnover procedure. We could have performed the Nuss operation in these two patients without concern for complications. Minimally invasive pectus excavatum repair can also be performed safely in patients that have had previous sternal surgery.
The results of this study show that the Nuss procedure can be performed safely and effectively even in adult patients, when a compound bar technique with 3-point wire fixation, the Crane technique, and double bar insertion is employed. The findings suggest that double bar insertion might be more stable and safer in late adolescent and adult patients with a severe pectus excavatum.
References
Dzielicki J, Korlacki W, Janicka I et al (2006) Difficulties and limitations in minimally invasive repair of pectus excavatum—6 years experience with Nuss technique. Eur J Cardiothorac Surg 30:801–804
Nuss D, Kelly RE Jr, Croitoru DP et al (1988) A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 33:545–552
Park HJ, Lee SY, Lee CS, Youm W et al (2004) The Nuss procedure for pectus excavatum: evolution of techniques and early results on 322 patients. Ann Thorac Surg 77:289–295
Fonkalsrud EW, DeUgarte D, Choi E (2002) Repair of pectus excavatum and carinatum deformities in 116 adults. Ann Surg 236:304–312 discussion 312–314
Mansour KA, Thourani VH, Odessey EA et al (2003) Thirty-year experience with repair of pectus deformities in adults. Ann Thorac Surg 76:391–395 discussion 395
Jaroszewski DE, Fonkalsrud EW (2007) Repair of pectus chest deformities in 320 adult patients: 21 year experience. Ann Thorac Surg 84:429–433
Kim do H, Hwang JJ, Lee MK et al (2005) Analysis of the Nuss procedure for pectus excavatum in different age groups. Ann Thorac Surg 80:1073–1077
Aronson DC, Bosgraaf RP, van der Horst C et al (2007) Nuss procedure: pediatric surgical solution for adults with pectus excavatum. World J Surg 31:26–29 discussion 30
Coln D, Gunning T, Ramsay M et al (2002) Early experience with the Nuss minimally invasive correction of pectus excavatum in adults. World J Surg 26:1217–1221
Schalamon J, Pokall S, Windhaber J et al (2006) Minimally invasive correction of pectus excavatum in adult patients. J Thorac Cardiovasc Surg 132:524–529
Olbrecht VA, Arnold MA, Nabaweesi R et al (2008) Lorenz bar repair of pectus excavatum in the adult population: should it be done? Ann Thorac Surg 86:402–408 discussion 408–409
Pilegaard HK, Licht PB (2008) Routine use of minimally invasive surgery for pectus excavatum in adults. Ann Thorac Surg 86:952–956
Teh SH, Hanna AM, Pham TH et al (2008) Minimally invasive repair for pectus excavatum in adults. Ann Thorac Surg 85:1914–1918
Hebra A, Jacobs JP, Feliz A et al (2006) Minimally invasive repair of pectus excavatum in adult patients. Am Surg 72:837–842
Goretsky MJ, Kelly RE Jr, Croitoru D et al (2004) Chest wall anomalies: pectus excavatum and pectus carinatum. Adolesc Med Clin 15:455–471
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoon, Y.S., Kim, H.K., Choi, Y.S. et al. A Modified Nuss Procedure for Late Adolescent and Adult Pectus Excavatum. World J Surg 34, 1475–1480 (2010). https://doi.org/10.1007/s00268-010-0465-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0465-9