Abstract
Background
Nonoperative management (NOM) of kidney gunshot injuries as an alternative to surgical exploration is rarely reported. The aim of this study was to assess the feasibility and safety of selective NOM of such injuries.
Methods
A 4-year prospective study was conducted that included all patients admitted to a Level I trauma center with kidney gunshot injuries. Patients with abdominal gunshot wounds and hematuria with no indications for immediate laparotomy (peritonitis, hemodynamic instability, head or spinal cord injury) underwent intravenous contrast abdominal computed tomography. Patients with confirmed kidney injuries were observed with serial clinical examinations. Outcome parameters included the need for delayed laparotomy, complications, length of hospital stay, and survival.
Results
During the study period, 33 patients with kidney gunshot injuries were selected for NOM without laparotomy. The mean Injury Severity Score was 10.5 (range 4–25). Simple kidney injuries (grades I, II) occurred in 15 (45.5%) patients and complex kidney injuries (grades III, IV) in 18 (54.5%) patients. Associated injuries included 14 of the liver (42.4%), 4 (12.1%) of the spleen, and 6 (18.2%) each of the diaphragm, lung (contusion), and hemothorax. Three patients required delayed laparotomy: two for nonrenal indications, and one patient had a delayed nephrectomy for a grade IV injury. The overall successful NOM rate was 90.9%. The mean hospital stay was 5.9 days (range 2–23 days). There were no kidney-related complications and no mortality.
Conclusion
Selective NOM of patients with kidney gunshot injuries is a feasible, safe, effective alternative to routine exploration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The nonoperative management (NOM) of abdominal gunshot wounds has yet to be accepted as the standard of care. Patients selected for NOM of kidney gunshot injuries are those who have sustained an abdominal gunshot wound(s) without an immediate indication for emergency laparotomy, who undergo contrast computed tomography (CT) to confirm a kidney injury, and are then managed without surgical exploration. This practice is not widely accepted. This study attempted to verify the feasibility and safety of selective NOM of kidney gunshot injuries as an alternative to routine exploration.
Patients and methods
This prospective, ethics committee-approved study was conducted in the Trauma Center in Groote Schuur Hospital in Cape Town, South Africa over a 4-year period (April 2004 to March 2008). All patients presenting with abdominal gunshot wounds were initially assessed and resuscitated along Advanced Trauma Life Support guidelines. Indications for emergency laparotomy were peritonitis (diffuse tenderness, rebound tenderness, guarding, rigidity), hemodynamic instability, and abdominal gunshot wounds with associated head and spinal cord injuries that precluded serial abdominal examination. Hemodynamically stable patients (sustained systolic blood pressure >100 mmHg, pulse rate <100, no more than 1 to 2 l of crystalloid transfusion) presenting with hematuria, with no signs of peritonitis, and with intact sensorium were selected for a trial of NOM.
The patients underwent a CT scan with intravenous contrast to identify or exclude a kidney injury. Patients with confirmed kidney injuries (grades I–IV) were admitted to a high-care observation area for continuous hemodynamic monitoring, 4-hourly hemoglobin estimation, and serial clinical examination. After 48 h in the high-care unit, once stabilized and tolerating food patients were transferred to a general trauma surgical ward. In the event of the development of peritonitis or hemodynamic instability at any time, laparotomy was promptly performed. Conservatively managed patients were treated with bed rest until any gross hematuria had resolved. Same-admission repeat CT scans were reserved for patients with clinical manifestations of kidney-related complications, such as a significant drop in the hemoglobin level without hemodynamic compromise, pyrexia with elevated white blood cell counts, and/or worsening flank pain. Patients with persistent macroscopic hematuria (>72 hours) underwent renal angiography. The injury severity was categorized using the Revised Trauma Score (RTS), Injury Severity Score (ISS), and American Association for Surgery of Trauma (AAST) organ injury scores. Outcome was determined by the need for delayed laparotomy, kidney-related morbidity, length of hospital stay, and survival. All patients were followed up 2 weeks from discharge.
Results
A total of 95 patients with kidney gunshot injuries were treated during the study period. Among them, 62 (65.3%) had an indication for emergency laparotomy and underwent therapeutic laparotomy, with a 66.1% nephrectomy rate.
Altogether, 38 CT scans were performed because of hematuria in stable patients. The scans revealed that 33 patients had kidney injuries. This cohort was selected for a trial of NOM and forms the basis of further analysis in this study. There were 32 males and 1 female with a mean age of 22.8 years (range 17–52) years. All had sustained low-velocity gunshot wounds and were hemodynamically stable on admission. In 14 of these patients, the gunshot trajectory involved the right thoracoabdominal region.
Computed tomography revealed 33 kidney, 14 liver, and 4 splenic injuries. There were 15 (45.5%) patients with isolated kidney injuries, 14 (42.4%) with combined liver and kidney injuries, 3 with combined kidney and splenic injuries, and 1 with a combination of kidney, spleen, and liver injuries. The remaining five CT scans either showed an extraperitoneal missile tract or a trajectory completely away from the upper urinary tract. The mean RTS and ISS were 7.841 and 10.5 (range 4–34), respectively. The kidney, liver, and spleen injury grading is shown in Table 1. Simple kidney injuries (grades I and II) and complex kidney injuries (grades III and IV) occurred in 15 (45.5%) and 18 (54.5%) patients, respectively.
To simplify the analysis, associated injuries were stratified according to those that were due to the same missile that caused the kidney injury and those that resulted from other missile trajectories (Table 2). Right-sided diaphragm injuries were accepted as being present when either lung contusion and/or hemo/pneumothorax was diagnosed with a liver and kidney injury caused by the same missile trajectory. Three patients with spinal cord injury (two with thoracic segments 9 and 11 and one with lumbar segment 1 spinal cord levels) were considered for NOM (breach of protocol). In these patients, the CT scan showed the bullet tract away from both the esophagus and aorta. Three Gastrografin esophageal studies were done and were normal. In two patients with a mediastinal hematoma, the thoracic aortograms were normal. All three patients were successfully managed without laparotomy.
Three patients failed abdominal observation and underwent delayed laparotomy. One patient developed signs of peritonitis and underwent laparotomy for a colon injury that was exteriorized. Another patient required a 5-unit transfusion in less than 12 hours, and at laparotomy a hemoperitoneum of 1,200 ml was found. A distal pancreatectomy and splenectomy was performed. Both patients had their liver injuries drained, and the kidney injuries were not explored. The third patient developed a spiking pyrexia with new chest radiographic opacities and worsening respiratory function requiring intubation and ventilation. Laparotomy prior to intensive care unit (ICU) admission to exclude any missed bowel injury resulted in nephrectomy due to difficulty when attempting to repair the shattered kidney. No missed bowel injury was detected. The first two patients also underwent repair of right-sided diaphragm injuries.
No kidney-related complications occurred in any of the patients. Liver-related complications occurred in two patients: one pleurobiliary fistula and one liver abscess. Both complications were treated successfully by endoscopic techniques: One patient underwent endoscopic retrograde cholangiography and stent placement, and the other underwent ultrasound-guided percutaneous drainage. Non-liver-related and non-kidney-related complications included one right-sided recurrent hemothorax that was treated with repeat tube thoracostomy. Two patients developed nosocomial pneumonia and were managed with antibiotics.
The mean hospital stay for patients undergoing successful NOM for isolated kidney injury was 3.1 days (range 2–4 days), for kidney and liver injury 7.5 days (range 4–23 days), and for patients undergoing nephrectomy 8.1 days (range 5–63 days). There were no deaths. A 2-week clinical follow-up of 100% revealed no new complications or patients requiring readmission. At 1 month and at 6 weeks, 13 (39.4%) and 9 (27.3%) patients, respectively, attended the follow-up clinic and had no clinically relevant problems.
Discussion
The selective NOM of penetrating abdominal trauma has evolved over the last two decades. While clinically evaluable patients with abdominal stab wounds are safely managed with serial clinical examination [1], the same approach to low-velocity abdominal gunshot wounds has not been readily accepted. There is, however, increasing evidence that the NOM of abdominal gunshot wounds is practical and safe, with up to one-third of all abdominal gunshot wounds being managed successfully nonoperatively [2–6]. The NOM of blunt solid organ injuries is widely accepted, with success rates of up to 95%. Conversely, selective NOM of solid-organ gunshot injuries, in particular kidney gunshot injuries, has not been widely practiced.
In our center, the only absolute criterion for immediate surgical intervention for kidney trauma is hemodynamic instability. Intraoperative renal exploration is also indicated for all suspected kidney injuries in patients without complete preoperative imaging. Patients with a vascular pedicle and renal pelvis and ureteral injuries require immediate exploration. In this series, 41 (66.1%) nephrectomies were performed in 62 patients who underwent immediate laparotomy for peritonitis or hemodynamic instability. The most common indications for nephrectomy were hilar injuries (n = 19, 46.3%) and severe parenchymal disruption that precluded repair (n = 17, 41.5%). Furthermore, 16 (39%) patients in whom time-consuming renal salvage procedures were clearly contraindicated underwent damage-control laparotomy; and among them only 5 patients had grade III or lesser injuries that may have been amenable to renorrhaphy. All patients in this series undergoing nephrectomy had sustained gunshot injuries, all had associated intraabdominal injuries, and 36 (87.8%) of the patients had high-grade injuries (17 with grade IV injuries and 19 with grade V injuries). This is in keeping with the predictors of nephrectomy, which includes factors such as gunshot injuries, high renal injury grades, and hemodynamic instability [7–9].
The percentage of kidney stab wounds amenable to NOM ranges between 51 and 77%, with success rates of >95% [10–12]. It has been reported, though, that gunshot wounds are significantly more likely to result in severe kidney injuries than stab wounds [9]—hence the reluctance perhaps to manage these patients nonoperatively. It has also been suggested that the threshold for exploring urinary extravasation for gunshot wounds should be lower than that for stab wounds because of the increased risk of delayed complications due to extensive tissue damage from the projectile’s blast effect.
All the studies on conservatively managed gunshot wounds have been retrospective in nature. Although there is some evidence to support the idea that with accurate preoperative imaging and grading of the kidney injury, grades I–III need not be explored at the time of laparotomy for other injuries, the evidence to support NOM of isolated kidney gunshot injuries is sparse [13]. Overall, among the 63 cases of nonoperatively managed kidney gunshot injuries identified in the English-language literature, a success rate of almost 99% has been reported (Table 3). This is comparable to our success rate of 91%. McAninch and colleagues reported a series of 87 gunshot kidney units, of which 10 were not explored at laparotomy for associated injuries and 8 (9.2%) were managed with a 100% success rate without laparotomy [14]. Similarly, Velmahos et al. managed four patients in a series of 52 consecutive kidney gunshot injuries successfully nonoperatively without laparotomy [15].
One of the major concerns regarding NOM of abdominal gunshots wounds is missing a hollow viscus injury. Although modern imaging performed by experienced radiologists using state of the art scanners can demonstrate ongoing hemorrhage and corroborate evidence of hollow viscus injury (free air, free fluid in the absence of solid organ injury, localized bowel wall thickening, mesentery stranding, hematoma surrounding a hollow viscus), the level of accuracy and sensitivity for diagnosing bowel injuries following penetrating trauma remains a source of concern [16–18]. It is therefore essential that the attending surgeon employ continuous serial clinical examinations to identify such injuries in patients who are considered for NOM. Although no renal-related complications were noted in this series, complications that may occur with expectant management are ongoing bleeding or rebleeding (increase in perinephric hematoma, appearance of macroscopic hematuria; persistent microscopic hematuria), infected perinephric fluid collections, and persistent urinary leaks. These problems can usually be managed by interventional radiologic and endoscopic techniques with excellent success rates. Although outside the scope of this report, all 14 liver injuries and 3 of the 4 splenic injuries were successfully managed conservatively.
This study is the first prospective and largest series of NOM kidney gunshot injuries managed without laparotomy. It contributes to the small growing body of evidence in support of NOM of kidney gunshot injuries in a select group of clinically evaluable, hemodynamically stable patients. When selecting patients for NOM of kidney gunshot injuries, CT is essential for grading the injury accurately. Altogether, 33.7% of all kidney gunshot injuries were managed nonoperatively without laparotomy with a 90.9% success rate. The surgeon must recognize the risks of NOM of kidney gunshot injuries and have the resources (angiography with angioembolization and percutaneous radiologic interventional techniques) available to address potential complications.
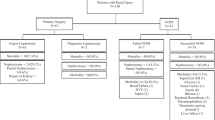
Our institutional management algorithm for penetrating kidney injuries is shown in Fig. 1. However, NOM of abdominal gunshot wounds, with or without kidney injury and with or without advanced CT technology, is still based largely on the findings from serial clinical examinations.
References
Navsaria PH, Ju Berli, Edu S et al (2007) Non-operative management of abdominal stab wounds: an analysis of 186 patients. S Afr J Surg 45:128–132
Demetriades D, Charalambides D, Lakhoo M et al (1991) Gunshot wound of the abdomen: role of selective conservative management. Br J Surg 78:220–222
Velmahos GC, Demetriades D, Foianini E et al (1997) A selective approach to the management of gunshot wounds to the back. Am J Surg 174:342–346
Velmahos GC, Demetriades D, Toutouzas KG et al (2001) Selective nonoperative management in 1,856 patients with abdominal gunshot wounds: should routine laparotomy still be the standard of care? Ann Surg 234:395–402
Demetriades D, Velmahos G, Cornwell E III et al (1997) Selective nonoperative management of gunshot wounds of the anterior abdomen. Arch Surg 132:178–183
Pryor JP, Reilly PM, Dabrowski GP et al (2004) NOM of abdominal gunshot wounds. Ann Emerg Med 43:344–353
Thall EH, Stone NN, Cheng DL et al (1996) Conservative management of penetration and blunt type III renal injuries. J Urol 77:512–517
Wessels H, McAninch JW, Meyer A et al (1997) Criteria for nonoperative treatment of significant penetrating renal lacerations. J Urol 157:24–27
Armenakas NA, Duckett CP, McAninch JW (1999) Indications for nonoperative management of renal stab wounds. J Urol 161:768–771
Davis KA, Reed RL 2nd, Santaniello J et al (2006) Predictors of the need for nephrectomy after renal trauma. J Trauma 60:164–169
Kansas BT (2004) Incidence and management of penetrating renal trauma in patients with multiorgan injury. J Urol 172:1355–1360
Shariat SF, Roehrborn CG, Karakiewicz PI et al (2007) Evidence-based validation of the predictive value of the American Association for the Surgery of Trauma Kidney Injury Scale. J Trauma 62:933–939
Heyns CF (2004) Renal trauma: indications for imaging and renal exploration. BJU Int 93:1165–1170
McAninch JW, Carroll PR, Armenakas NA et al (1993) Renal gunshot wounds: methods of salvage and reconstruction. J Trauma 35:279–283
Velmahos GC, Demetriades D, Cornwell EE et al (1998) Selective management of renal gunshot wounds. Br J Surg 85:1121–1124
Renz BM, Bott J, Feliciano DV (1996) Failure of nonoperative treatment of a gunshot wound to the liver predicted by computed tomography. J Trauma 40:191–193
Philips T, Scalafini SJ, Goldstein A et al (1986) Use of contrast-enhanced CT enema in the management of penetrating trauma of the flank and back. J Trauma 26:593–601
Sherck J, Shatney C, Sensaki K et al (1994) The accuracy of computed tomography in the diagnosis of blunt small bowel perforation. Am J Surg 168:670–675
Cheng DLW, Lazan D, Stone N (1994) Conservative treatment of type III renal trauma. J Trauma 36:491–494
Hammer CC, Santucci RA (2003) Effect of an institutional policy of nonoperative treatment of significant penetrating renal lacerations. J Urol 169:1751–1753
DuBose J, Inaba K, Teixeira PG et al (2007) Selective non-operative management of solid organ injury following abdominal gunshot wounds. Injury 38:1084–1090
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Navsaria, P.H., Nicol, A.J. Selective Nonoperative Management of Kidney Gunshot Injuries. World J Surg 33, 553–557 (2009). https://doi.org/10.1007/s00268-008-9888-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9888-y