Abstract
Purpose
Nonoperative management (NOM) of gunshot liver injuries (GLI) is infrequently practiced. The aim of this study was to assess the safety of selective NOM of GLI.
Methods
A prospective, protocol-driven study, which included patients with GLI admitted to a level 1 trauma center, was conducted over a 52-month period. Stable patients without peritonism or sustained hypotension with right-sided thoracoabdominal (RTA) and right upper quadrant (RUQ), penetrating wounds with or without localized RUQ tenderness, underwent contrasted abdominal CT scan to determine the trajectory and organ injury. Patients with established liver and/or kidney injuries, without the evidence of hollow viscus injury, were observed with serial clinical examinations. Outcome parameters included the need for delayed laparotomy, complications, the length of hospital stay and survival.
Results
During the study period, 54 (28.3%) patients of a cohort of 191 patients with GLI were selected for NOM of hemodynamic stability, the absence of peritonism and CT imaging. The average Revised Trauma Score (RTS) and Injury Severity Score (ISS) were 7.841 and 25 (range 4–50), respectively. 21 (39%) patients had simple (Grades I and II) and 33 (61%) patients sustained complex (Grades III to V) liver injuries. Accompanying injuries included 12 (22.2%) kidney, 43 (79.6%) diaphragm, 20 (37.0%) pulmonary contusion, 38 (70.4%) hemothoraces, and 24 (44.4%) rib fractures. Three patients required delayed laparotomy resulting in an overall success of NOM of 94.4%. Complications included: liver abscess (1), biliary fistula (5), intrahepatic A-V fistula (1) and hospital-acquired pneumonia (3). The overall median hospital stay was 6 (IQR 4–11) days, with no deaths.
Conclusion
The NOM of carefully selected patients with GLI is safe and associated with minimal morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The trauma fraternity is gradually embracing the selective nonoperative management (NOM) of penetrating abdominal trauma. The NOM of abdominal stab wounds (SW) is widely accepted and considered the standard of care. Conversely, the NOM of gunshot wounds to the abdomen is slowly gaining momentum in the context of concurrent use of computerized tomographic (CT) scanning in patients without peritonism or sustained hypotension. Patients who sustained a gunshot wound to the abdomen, not having an indication for emergency laparotomy, and undergoes CT imaging that shows liver injuries with or without other solid organ injuries and the absence of any evidence of hollow viscus injuries, are selected for NOM. This study sought to validate the feasibility and safety of the NOM of gunshot liver injuries (GLI).
Patients and methods
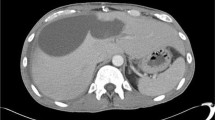
This study is a retrospective analysis of prospectively collected data of a University of Cape Town Human Research Ethics Committee approved protocol-driven study that was conducted over a 52-month period (September 2008–December 2012) at Groote Schuur Hospital Trauma Center (GSHTC) in Cape Town, South Africa. All patients with penetrating abdominal trauma presenting to the GSHTC were initially assessed and resuscitated according to the standard guidelines. The patients with hemodynamic instability, signs of peritonism (diffuse abdominal tenderness, rebound tenderness, guarding, or rigidity), and unreliable physical examination due to the associated brain and spinal cord injuries were taken to the theater for emergency laparotomy. Stable patients with intact sensorium and without signs of peritonism were selected for a trial of NOM. An abdominal CT scan was performed using a 16-channel scanner with a high-power injection of 100 mL of intravenous contrast at 5 mL/s on all patients with right upper quadrant (RUQ) and right-sided thoracoabdominal (RTA) penetrating injuries, with or without localized RUQ tenderness, to identify or exclude a liver injury. During CT imaging, arterial, porto-venous, and delayed phases were routinely acquired. The patients with CT confirmed liver injuries, without CT evidence of hollow-viscus injury (free air-related to hollow viscera, bowel wall thickening, mesentery stranding, close proximity of missile trajectory to hollow viscus) were admitted to a high-care observation area in the general trauma ward for continuous hemodynamic monitoring including blood-pressure, pulse rate, saturation, respiratory rate, 4-hourly hemoglobin, and physical examination at regular intervals. Intrahepatic pseudo-aneurysms or arteriovenous fistulae detected on the initial CT underwent peripheral percutaneous angiography and embolization. The patient is regularly reviewed on ward rounds with the on-call trauma operative team which includes a senior and junior trauma consultant (both board-certified surgeons) and general surgical trainees (3–4th year of training) at 08H00 and 16H00 daily. The surgical trainee on call will review the patient at least once between 08H00 and 16H00, and at least twice after 16H00 till the next morning at 08H00. On-call consultants are available to review the patient at the request of the on-call surgical trainee. Re-examination consists of documenting the BP, pulse, temperature, respiratory rate, hemoglobin check, enquiring about GIT symptoms (nausea, vomiting, and diarrhea) and abdominal examination focusing on any distension, increasing tenderness or frank peritonitis. A data sheet with standardized documentation of the abdominal exam is completed after each examination (Fig. 1). An immediate laparotomy was performed if there was development of peritonitis, increasing local tenderness, hemodynamic instability or significant hemoglobin drop needing more than four units of blood transfusion in 24 h at any time during admission. During the first 24 h, the patient is administered intravenous fluids and thereafter, an oral diet is introduced. The patient was transferred to the general ward section after 48 h of close observation once tolerating an oral diet. CT scan is repeated only for clinically suspected liver-related septic complications (infected biloma, liver abscess, subphrenic or perihepatic collections, thoracobiliary fistula) and haemobilia. On discharge from hospital, all patients were entered into a 3-month follow-up programe (2 weeks then monthly thereafter), and issued with a summary note detailing diagnosis and management, and a list of instructions: no contact sport for 8 weeks, and to return to the unit in the event of jaundice, abdominal pain or distension, vomiting, loss of appetite, fever and upper or lower gastrointestinal bleeding.
The severity of the injury was characterized using the Revised Trauma Score (RTS), Injury Severity Score (ISS) and American Association of Surgery for Trauma (AAST) grading for solid organ injury. The outcome was measured by the need for delayed laparotomy, liver-related complications, the duration of hospital stay and survival.
Results
A total of 278 patients were admitted with penetrating liver injuries during the study period. Of these, 87 (31.3%) liver stab wounds and 191 (68.7%) patients sustained GLI. Of 191 GLI patients, 137 (71.7%) required an emergency laparotomy. At laparotomy 65 (47.4%) patients did not have any surgical intervention related to the liver (Table 1).
By hemodynamic stability, the absence of peritonism and CT findings, 54 (28.3%) GLI patients were admitted for NOM. Of these, 51 were male, and 3 were female with a mean age of 27 (range 14–88) years. The average RTS and ISS was 7.841 and 25 (range 4–50), respectively. Although 18 patients had associated haematuria, CT revealed 12 patients with both liver and kidney injuries, and 42 patients with isolated liver injuries. 21 (39%) patients had simple (Grades I and II) and 33 (61%) patients sustained complex (Grades III–V) liver injuries (Table 2). Associated right-sided diaphragm injuries were recognized in the presence of right-sided hemo/pneumothoraces or lung contusion from the same missile trajectory (Table 3).
Of the 54 GLI, three (5.6%) patients failed abdominal observation and underwent delayed laparotomy; one with a grade 2 liver injury and two with Grade 4 liver injuries. This translates to a 95 and 93.9% NOM success rate for simple and complex liver injuries, respectively. No hollow viscus injuries were detected at laparotomy (Table 4). Complications related to liver injury were seen in seven (13%) patients, and all occurred during the acute index admission. One patient developed a liver abscess, confirmed with repeat CT scan based on increased septic markers (fever and neutrophilic leucocytosis) that was treated by ultrasound-guided percutaneous drainage. Cultures grew a cloxacillin sensitive Staphylococcus aureus. In one patient, admission CT revealed an arteriovenous fistula that underwent immediate successful angioembolization (AE). There were five biliary cutaneous fistulas of which, three fistulas developed through the drains placed at the time of laparotomy for failed conservative management and two in the NOM group. All three patients in the failed conservative management group who developed postoperative biliary cutaneous fistulas, required further intervention with an endoscopic retrograde cholangiogram (ERC) for persistent peripheral bile leaks (> 50 mL for > 14days). Biliary sphincterotomy and a 10 Fr stent were placed to manage these patients. The outcome of these patients was further uneventful except an extended hospital stay (mean 22 days). The two patients with the biliary fistulas in the NOM group, both underwent repeat CT scans to exclude intrahepatic/perihepatic septic collections. One intrahepatic culture-negative biloma was managed successfully by percutaneous drainage and the other fistula that developed through the GSW site, resolved spontaneously. Non-liver-related complications included nosocomial pneumonia or infected lung contusions established in three patients, treated successfully with intravenous antibiotics. The overall median hospital stay was 6 (IQR 4–11) days. There were no deaths and also, no new complications requiring readmission of any patients in the 2-week clinical follow-up of 100%. The follow-up at one-month and two months was 40% and 10%, respectively, with no new complications encountered. The three patients with biliary fistulas who had a stent placed had a repeat ERC at 6 weeks. All biliary leaks had resolved, and the stents were removed without any complications.
Discussion
Liver injuries commonly occur in both blunt and penetrating abdominal trauma. Management of liver trauma has radically changed over the last three decades. For blunt trauma to the liver, NOM has now become the standard of care in stable patients, irrespective of grades of injury. For penetrating liver injuries, selective NOM is also gaining popularity. Selective NOM for a stab wound to the liver is practical and safe in the absence of hemodynamic instability or without the evidence of concomitant hollow visceral injury. Although different authors described selective NOM for low-velocity GLI, it has not yet been widely practiced [1,2,3,4].
Demetriades et al. first described NOM in penetrating liver trauma in 1986. The authors assumed liver injuries based on the trajectories with penetrating trauma in the RUQ of the abdomen. In their prospective study, all 21(33%) patients selected for non-surgical treatment were managed successfully with serial physical examinations and blood transfusions when needed without any complications [5]. Since then, selective NOM has become a preferred strategy for penetrating liver trauma. Later, several reports were published in the literature, but most had a relatively small cohort of patients [6].
The reports of NOM related to GLI appeared more frequently since the nineties [4, 7,8,9,10,11,12,13,14]. Renz et al. [7] are attributed to reporting first successful NOM of GLI. In their small series of 13 patients with an RTA gunshot, 7 had CT confirmed liver injuries who were successfully managed nonsurgically without any liver-related complications [7]. In the following year, Chmielewski et al. described successful NOM in 12 patients with RUQ gunshot wound, of which eight sustained grade II–III liver injuries [8]. Demetriades et al. reported lower success rate (69%) for selective NOM in GLI. They managed to treat 11 of 16 patients nonsurgically successfully, and concluded that particular patients with simple (grade I/II) liver injuries can be managed nonoperatively [10]. Later in 2005, in a relatively larger series of patients by Omoshoro-Jones et al. described 97% success rate of NOM for GLI. In their series of 33 patients, 8, 14 and 11 patients had grade I/II, grade III and grade IV/V liver injuries, respectively. Only two patients failed conservative management and required delayed laparotomy unrelated to liver trauma [11]. More recently, in 2009, Navsaria et al. described 92% success of NOM for both simple and complex GLI. They treated 58 of 63 patients nonoperatively, the largest series in the literature so far, with overall liver-related complications seen in only 9.5% (three liver abscesses, and three biliary fistulas) of patients [4]. The overall success rate of NOM for GLI, identified in the English literature, is 93% (Table 5) that is similar to our current series (94.4%). The constant high success rate could be ascribed to the fact that most isolated GLI requires no treatment [15].
A ‘blush’ of contrast on CT scan, seen only once in this study, signifies a false aneurysm, arteriovenous fistula or intrahepatic bleeding. Hemodynamically stable patients should be immediately transferred for angioembolization (AE), which is essential for the success of NOM [16, 17]. The main complication after AE is hepatic necrosis [18]. Recently, Michailidou et al. [19] described a small pseudoaneurysm following blunt trauma that was successfully observed without intervention. As the risk of hepatic necrosis is high, Scalea in a recent review suggested avoiding AE for small pseudoaneurysm in asymptomatic patients and selective embolization for a large aneurysm with coils rather than the use of gel foam [6]. Hepatic necrosis can be managed better by early hepatic lobectomy than repeated attempts of debridement or interventional drain placement [20].
Missing a hollow visceral injury is the downside of the success of NOM following a gunshot wound to the abdomen in the absence of peritonism. The sensitivity and accuracy for diagnosing hollow visceral injury characterized by free intraperitoneal or retroperitoneal air, free fluid in the absence of a solid organ injury, hematoma adjacent to hollow viscera, thickening of the wall of the injured bowel, mesenteric stranding following penetrating abdominal trauma remain an apprehension even with modern, and sophisticated CT scanners [17, 21, 22]. Patients who are considered for NOM should undergo serial physical examination, and any signs of deterioration, warrants a laparotomy [4].
The number of right-sided diaphragm injuries may have been underestimated in this study; since CT scan is not a reliable method in diagnosing penetrating diaphragm injuries. Low-velocity gunshot injuries to the diaphragm tend to be minor Grade 1 injuries, and with the liver providing a protective covering of the entire diaphragm, herniation is very unlikely. In our experience, we have not seen a single right-sided hollow-visceral diaphragm herniation to date following low-velocity penetrating trauma.
Ongoing bile leak, perihepatic biliary collection, biliary fistula, infected biloma, liver abscess or bleeding from false aneurysms or AVF are the common liver-related complications. In symptomatic patient follow-up, ultrasound or CT scan can be used to diagnose these complications. Ongoing bile leak can be managed by ERC and stenting and/or biliary sphincterotomy. Biliary abscess and infected biloma can be drained percutaneously under cover of intravenous broad spectrum antibiotics [23]. Only one liver-related septic complication occurred in our study. The three patients treated with intravenous antibiotics for hospital-acquired pneumonia, or infected pulmonary contusions may have masked or inadvertently treated liver-related septic complications [4]. While beyond the scope of this report, all associated 12 renal injuries were successfully managed nonsurgically. The reports of conservative treatment of gunshot kidney injuries are few, and this study provides further evidence that NOM is also highly practical, and when associated with liver injuries, does not preclude the NOM of either solid organ [14, 24,25,26,27].
A major limitation of this study is the patients lost to follow-up. According to Leukhardt et al. [28], lower income, higher poverty rates, and lower education are significantly associated with failure to follow-up. The patient cohort in this study met the above criteria and that would possibly account for the high rate in the failure to follow-up. Second, in keeping with the theme of NOM, the patients who failed abdominal observation could have possibly been manged successfully, laparoscopically, an option we will consider including in our protocol. Finally, considering the small numbers of patients treated, it begs the question of whether one can maintain the consistency in the use of this protocol. In a center with a high incidence of penetrating trauma like ours, this management protocol was successful in avoiding a significant number of nontherapeutic laparotomies in 51 (94%) of the 54 patients reviewed in this study. In our center, it certainly appears to be a viable and successful management option.
In conclusion, our study validates the efficacy of NOM for GLI using serial clinical examination in a particular group of hemodynamically stable and clinically assessable patients. The candidates qualifying for NOM are selected by CT imaging that identifies liver injury following a RTA and RUQ gunshot wounds with or without a localized tenderness. In our current series, 26.7% (51/191) of GLI were managed without laparotomy with a 94.4% success rate, irrespective of the severity of the injury. An associated liver-related complication rate of 13% is acceptable but requires ongoing vigilance and intermittent minimally invasive therapies including AE, percutaneous interventional drainage techniques, ERC, and stenting. However, NOM of penetrating abdominal trauma is still mainly based on the findings of serial clinical examinations, irrespective of solid organ injury and cutting-edge CT technology.
References
Navsaria PH, Berli J, Edu S, Nicol AJ. Non-operative management of abdominal stab wounds: an analysis of 186 patients. S Afr J Surg. 2007;45:128–32.
Moore EE. When is nonoperative management of a gunshot wound to the liver appropriate? J Am Coll Surg. 1999;188:427–8.
Garrett KA, Stain SC, Rosati C. Nonoperative management of liver gunshot injuries. Curr Surg. 2006;63:169–73.
Navsaria PH, Nicol AJ, Krige JE, Edu S. Selective nonoperative management of liver gunshot Injuries. Ann Surg. 2009;249:653–6.
Demetriades D, Rabinowitz B, Sofianos C. Non operative management of penetrating liver injuries: a prospective study. Br J Surg. 1986;73:736–7.
Scalea TM. Penetrating Liver Injuries. Curr Trauma Rep. 2015;1(2):69–75.
Renz BM, Feliciano DV. Gunshot wounds to the right thoracoabdomen: a prospective study of nonoperative management. J Trauma. 1994;37:737–44.
Chmielewski GW, Nicholas JM, Dulchavsky SA, Diebel LN. Nonoperative management of gunshot wounds of the abdomen. Am Surg. 1995;61:665–8.
Ginzburg E, Carrillo EH, Kopelman T, McKenney MG, Kirton OC, Shatz DV, et al. The role of computed tomography in selective management of gunshot wounds to the abdomen and flank. J Trauma. 1998;45:1005–9.
Demetriades D, Gomez H, Chahwan S, Charalambides K, Velmahos G, Murray J, et al. Gunshot injuries to the liver: the role of selective nonoperative management. J Am Coll Surg. 1999;188:343–8.
Omoshoro-Jones JA, Nicol AJ, Navsaria PH, Zellweger R, Krige JE, Kahn D. Selective non-operative management of liver gunshot injuries. Br J Surg. 2005;92:890–5.
Pal KM, Khan A. Nonoperative management of penetrating liver trauma. Injury. 2000;31:199–201.
Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Scalea TM. Triple-contrast helical CT in penetrating torso trauma: a prospective study to determine peritoneal violation and the need for laparotomy. Am J Roentgenol. 2001;177:1247–56.
DuBose J, Inaba K, Teixeira PG, Pepe A, Dunham MB, McKenney M. Selective nonoperative management of solid organ injury following abdominal gunshot wounds. Injury. 2007;38:1084–90.
Marr JDF, Krige JEJ, Terblanche J. Analysis of 153 gunshot wounds of the liver. Br J Surg. 2000;87:1030–4.
Demetriades D, Hadjizacharia P, Constantinou C, Brown C, Inaba K, Rhee P, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg. 2006;244:620–8.
Renz BM, Bott J, Feliciano DV. Failure of nonoperative treatment of a gunshot wound to the liver predicted by computed tomography. J Trauma. 1996;40:191–93.
Dabbs DN, Stein DM, Scalea TM. Major hepatic necrosis: a common complication after angioembolization for treatment of high-grade liver injuries. J Trauma Acute Care Surg. 2009;66(3):621–9.
Michailidou M, Velmahos GC, Wilden G, Alam HB, de Moya M, Chang Y. Blush on trauma computed tomography: not as bad as we think. J Trauma Acute Care Surg. 2012;73(3):580–6.
Dabbs DN, Stein DM, Philosophe B, Scalea TM. Treatment of major hepatic venous: lobectomy versus serial debridements. J Trauma. 2010;69:562–67.
Philips T, Scalafini SJ, Goldstein A, Scalea T, Panetta T, Shaftan G. Use of contrast–enhanced CT enema in the management of penetrating trauma of the flank and back. J Trauma 986; 6:593–601.
Sherck J, Shatney C, Sensaki K, Selivanov V. The accuracy of computed tomography in the diagnosis of blunt small bowel perforation. Am J Surg. 1994;168:670–5.
Bala M, Gazalla SA, Faroja M, Bloom AI, Zamir G, Rivkind AI, et al. Complications of high grade liver injuries: management and outcome with focus on bile leaks. Scand J Trauma Resusc Emerg Med. 2012;20:20. https://doi.org/10.1186/1757-7241-20-20 (PMCID: PMC3352307).
Navsaria PH, Nicol AJ. Selective nonoperative management of kidney gunshot injuries. World J Surg. 2009;33:553–7.
Velmahos GC, Demetriades D, Cornwell EE III, et al. Selective management of renal gunshot wounds. Br J Surg. 1998;85:1121–4.
Wessells H, McAninch JW, Meyer A, Bruce J. Criteria for nonoperative management of significant penetrating renal lacerations. J Urol. 1997;157:2427.
Moolman C, Navsaria PH, Lazarus J, Pontin A, Nicol AJ. Nonoperative management of penetrating kidney injuries: a prospective audit. J Urol. 2012;188:169 – 73.
Leukhardt WH, Golob JF, McCoy AM, Fadlalla AM, et al. Follow-up disparities after trauma: a real problem for outcomes research. Am J Surg. 2010;199:348–53.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Pradeep Navsaria, Andrew Nicol, Jake Krige, Sorin Edu and Sharfuddin Chowdhury declare that they have no conflict of interest.
Ethical approval
The study has been approved by the institutional ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards: University of Cape Town Human Research Ethics Committee approved study: 048/2007.
Informed consent
This was a retrospective review of prospectively collected data (observational study); therefore, no consent was taken. The patients were managed according to standard Unit protocols. All data were collected by the first author on a password-protected computer and Excel sheet. None of the patients could be identified in the database as they were numbered consecutively from 1 to 278. The privacy and confidentiality interests of participants were preserved. No information can identify individuals.
Rights and permissions
About this article
Cite this article
Navsaria, P., Nicol, A., Krige, J. et al. Selective nonoperative management of liver gunshot injuries. Eur J Trauma Emerg Surg 45, 323–328 (2019). https://doi.org/10.1007/s00068-018-0913-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0913-z