Abstract
Background
Although total thyroidectomy is the procedure of choice in patients with thyroid carcinoma, this surgical approach has emerged as a surgical option to treat patients with benign multinodular goiter (BMNG), especially in endemically iodine-deficient regions. The aim of this study was to review our experience with patients with BMNG in an endemically iodine-deficient region treated by either subtotal or total/near-total thyroidectomy, and to document whether total or near-total thyroidectomy decreased the rate of completion thyroidectomy for incidentally diagnosed thyroid carcinoma in comparison to the patients with BMNG treated initially by subtotal thyroidectomy.
Methods
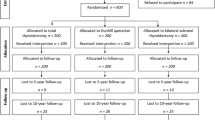
Two thousand five hundred ninety-two patients with BMNG were included. There were 1695 bilateral subtotal thyroidectomies (group 1) and 1211 total or near-total thyroidectomies (group 2) for BMNG during this period. All patients were euthyroid and had no history of hyperthyroidism, radiation exposure, or familial thyroid carcinoma. Any patient with preoperative or perioperative suspicion of malignancy or hyperthyroidism was excluded.
Results
Bilateral subtotal thyroidectomy was performed in 1695 patients (58.3%) in group 1 and total or near-total thyroidectomy in 1211 patients (41.7%), in group 2, respectively. The incidence of incidental thyroid carcinoma was found to be 7.2% (n = 210/2906). Although the rate of permanent hypoparathyroidim and transient or permanent unilateral recurrent laryngeal nerve (RLN) palsy were not significantly different between the two groups, transient hypoparathyroidism was significantly higher in group 2 than in group 1 (8.4% vs. 1.42%; p < 0.001, odds ratio [OR] = 52.98). The incidence of thyroid carcinoma was significantly higher in group 2 (10.7%, n = 129/1211) than in group 1 (4.68%, n = 81/1695) (p < 0.001; OR = 39.1).Thirty-eight patients in group 1 (2.24%) underwent completion thyroidectomy, whereas completion thyroidectomy has been not indicated in group 2 (p = 0.007). Two of 38 patients (5.26%) had thyroid papillary microcarcinoma on their remnant thyroid tissue. The rate of recurrent goiter was 7.1% in group 1. The average time to recurrence in group 1 was 14.9 ± 8.7 years. Six of 121 patients with recurrent disease (4.95%) has been operated on.
Conclusions
Subtotal thyroidectomy resulted in a significantly higher rate of completion thyroidectomy for incidentally diagnosed thyroid carcinoma compared with total or near-total thyroidectomy in patients with BMNG. The extent of surgical resection had no significant effect on the rate of permanent complications. We recommend total or near-total thyroidectomy in BMNG to prevent recurrence and to eliminate the necessity for early completion thyroidectomy in case of a final diagnosis of thyroid carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although total thyroidectomy is the procedure of choice in patients with thyroid carcinoma, Basedow-Graves disease, and toxic multinodular goiter, this surgical approach has emerged as a surgical option to treat patients with benign multinodular goiter (BMNG), especially in endemically iodine-deficient regions [1–9]. A considerable number of patients undergoing primary treatment with subtotal resection need reoperation for recurrence, which has a higher complication rate compared with primary procedures [3, 10–14]. The incidence of thyroid carcinoma varies from 7.5 to 13% in multinodular goiter [15–17]. The presence of multiple nodules decreases the diagnostic value of fine-needle aspiration biopsy, and thyroid carcinoma is frequently an incidental postoperative histologic finding in BMNG. In such patients treated with subtotal thyroidectomy, completion thyroidectomy might be necessary.
Subtotal thyroidectomy in patients with BMNG has resulted in reoperation for recurrence in 13–20% of patients, reaching a peak incidence 13 years after the primary operation [3]. To perform total thyroidectomy for BMNG is controversial. Although total thyroidectomy is not justified in BMNG, as the risk for malignancy is low and associated complication rates are high, it can be performed safely in BMNG, and reoperations have a greater risk [3, 5, 6, 8–10, 17–20]. We documented in a prospective study that total or near-total thyroidectomy decreased the rate of completion thyroidectomy for incidentally diagnosed thyroid carcinoma in BMNG in an endemically iodine-deficient region and that the incidence of thyroid carcinoma in BMNG without any previous suspicion of malignancy was 8.2% [21]. We concluded that subtotal thyroidectomy resulted in a significantly higher rate of completion thyroidectomy for incidentally diagnosed thyroid cancer compared with total or near-total thyroidectomy [21].
The aim of this retrospective study was to review our experience with patients with BMNG in an endemically iodine-deficient region who were treated with subtotal or total/near-total thyroidectomy and to document whether total or near-total thyroidectomy decreased the rate of completion thyroidectomy for incidentally diagnosed thyroid carcinoma.
Material and methods
From January 1, 1988, to December 31, 2007, 2906 patients with BMNG were treated at the Department of Surgery of Istanbul Faculty of Medicine. There were 1695 bilateral subtotal thyroidectomies (group 1) and 1211 total or near-total thyroidectomies (group 2) for BMNG during this period. Since 1998 total thyroidectomy has become the first preferred option for surgical treatment of patients with BMNG involving both lobes of the thyroid. All patients were euthyroid and had no history of hyperthyroidism, radiation exposure, or familial thyroid carcinoma. Any patient with preoperative or perioperative suspicion of malignancy, hyperthyroidism, or recurrent goiter, or who was previously treated by unilateral lobectomy were excluded. Thyroid scanning and ultrasonography revealed multinodular hyperplasia of the thyroid gland. The total amount of estimated remnant thyroid tissue was intended to be 5 g or more in group 1 and none or less than 1 g in group 2. Near-total thyroidectomy was performed by the capsular dissection method, leaving less than 1 g of remnant tissue. The amount of remnant tissue was estimated as 1 cm3 = 1 g. Postoperative complications, thyrotropin (TSH) values at the first postoperative month, and the incidence of thyroid carcinoma were assessed in both groups. Total serum calcium was measured in all patients before and after the operation at the first postoperative day and at the first postoperative month. Serum calcium was measured by using an automated analyzer. Vocal cord examination was performed by an otolaryngologist pre- and postoperatively. We investigated whether there was a significant difference in the postoperative complications and in the rate of thyroid carcinoma requiring radioactive iodine (RAI) ablation and completion thyroidectomy between the two groups. Histologic criteria for RAI therapy included tumor size greater than 1.5 cm, any size tumor with thyroid capsule or extrathyroidal invasion, or multicentricity (3 tumor foci) [21]. The TSH values were required to be more than 30 mIU/l to refer the patient to RAI ablation therapy. Patients who were treated with RAI were verified to have undetectable levels of serum thyroglobulin and no uptake at the thyroid bed or distant sites by iodine I131 (131I)-labeled thyroid and whole-body scans after the treatment. These patients received suppressive doses of thyroid hormone, and serum thyroglobulin assays were performed at 6-month intervals. All patients with benign pathology who underwent total or bilateral subtotal thyroidectomy received nonsuppressive doses of thyroid hormone. Thyroid and whole-body scans labeled with 131I were repeated if serum thyroglobulin levels increased during further follow-up. Patients with noninvasive microcarcinoma who did not receive RAI ablation received suppressive doses of thyroid hormone after thyroidectomy [21].
The follow-up schedule of all patients in both groups was neck examination and determination of serum TSH values every 6 months during the first 2 years following thyroidectomy, and then annually. Linear correlation, paired t test, Mann–Whitney U test, and Fisher’s exact test were used for statistical analysis, and p < 0.05 was accepted as significant.
Results
The mean ± SD (standard deviation) age was found to be significantly higher in group 2 (46 ± 13.3 years) compared with that of group 1 (41 ± 12.9 years) (p = 0.01) (Table 1). The female:male ratio was 5.83 and 4.55 in for groups 1 and 2, respectively (p = 0.70). Of the 2906 patients included in the study, bilateral subtotal thyroidectomy was performed in 1695 (58.3%) (group 1) and total or near-total thyroidectomy in 1211 patients (41.7%) (group 2) (Table 1).
Postoperative findings
Permanent hypoparathyroidism occurred in 7 patients of group 1 (0.41%) and in 10 patients of group 2 (0.83%) (p = 0.15), whereas transient hypoparathyroidism was significantly higher in patients of group 2 than in patients of group 1 (8.4% vs. 1.42%; p < 0.001, odds ratio [OR] = 52.98) (Table 2). There were 28 (1.65%) patients with transient unilateral recurrent laryngeal nerve (RLN) palsy in group 1 and 20 (1.65%) in group 2 (p = 0.99). In group 1, 11 (0.64%) patients developed permanent unilateral RLN palsy, and 12 (0.9%) in group 2 (p = 0.3) (Table 2). None of the patients in groups 1 and 2 had bilateral RLN palsy. The mean ± SD TSH value at the first postoperative month was significantly higher in group 2 than in group 1 (41.22 ± 16.7 vs. 9.14 ± 5.2 mIU/l) (p < 0.01) (Fig. 1).
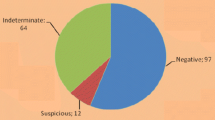
From 1988 to 1998 a total 1631 patients and from 1998 to 2007 a total 1275 patients were operated on for BMNG. The incidence of incidental thyroid carcinoma was significantly higher in patients operated on after 1998 (n = 150/1275) than in patients operated on between 1988 and 1998 (n = 60/1631) (11.8% vs. 3.7%; p < 0.001, OR = 70.24) (Fig. 2). The overall incidence of incidental thyroid carcinoma was found to be 7.2% (n = 210/2906). The incidence of thyroid carcinoma was significantly higher in group 2 (10.7%; n = 129/1211) than in group 1 (4.68%, n = 81/1695) (p < 0.001, OR = 39.1) (Table 1). The mean ± SD age of patients with thyroid carcinoma was not significantly different between patients of group 1 and group 2 (45 ± 13.5 vs. 46 ± 12.03 years) (p = 0.2) (Table 1).
Of those patients with thyroid carcinoma, 39 patients of group 1 (n = 39/81, 48.1%) had papillary microcarcinoma, with two tumor foci in 10 patients and three tumor foci in 5 patients, whereas 37 patients of group 2 (n = 37/129; 30.5%) had papillary microcarcinoma, with two tumor foci in 9, three tumor foci in 2, and four tumor foci in 2 patients. Multicentricity of papillary thyroid carcinoma was not significantly different between the two groups (p = 0.075; OR = 3.091). Follicular thyroid carcinoma has been found in two patients of group 1 and in one patient of group 2. There was only one patient with medullary thyroid carcinoma in group 2. Thirty-nine patients with thyroid carcinoma in group 1 (2.24%) underwent completion thyroidectomy (p = 0.007) (Table 1). There was only one transient hypocalcemia after completion thyroidectomy in those 38 patients. Two of 38 patients (5.26%) had thyroid papillary microcarcinoma on their remnant thyroid tissue.
The average time of follow-up is 11.7 years (range = 1–19 years). In group 1, 121 patients had recurrent nodular goiter (n = 121/1695; 7.1%), whereas no recurrence was observed in group 2 (p = 0.007) (Table 1). The average time to recurrence was 14.9 ± 8.7 years. Six patients (4.95%) were operated on. Histopathologic examination of residual tissue revealed benign nodular hyperplasia in all of these patients.
Discussion
In the present study, the incidence of incidental thyroid carcinoma was found to be 7.6% of patients who underwent an operation for multinodular euthyroid goiter without any preoperative or perioperative suspicion of malignancy. We documented that performance of total or near-total thyroidectomy instead of subtotal resection as the primary procedure significantly reduced the rate of completion thyroidectomy for incidentally found thyroid carcinoma in BMNG. The rate of permanent hypoparathyroidism and transient or permanent unilateral RLN palsy was not significantly different between patients treated by subtotal thyroidectomy and those treated by total or near-total thyroidectomy, whereas total or near-total thyroidectomy was associated with a statistically significant higher risk for transient hypoparathyroidism. However, the extent of surgical resection had no significant effect on the rate of permanent complications.
Total thyroidectomy is well accepted as the treatment for well-differentiated thyroid carcinoma. This approach has also been indicated for patients with hyperthyroidism, especially in patients with severe ophthalmopathy or thyroiditis who have a history of radiation to the head and neck, who have large thyroid glands, or who have nodules with suspicious cytology. If the the goiter is voluminous with symptoms of compression or if it is not possible to leave a grossly homogeneous thyroid remnant tissue because of the location of its possible nodules, total thyroidectomy is also recommended [6]. Total thyroidectomy has been accepted by many endocrine surgery centers, including ours, as the preferred approach for the surgical treatment of BMNG [1–9, 21]. This is a safe procedure with a minimal complication rate if performed by an experienced surgeon. The goal of surgical treatment in multinodular goiter should be to eliminate the disease with a low complication rate and to minimize the necessity for reoperation because the relative risk for permanent complications has been found to be higher in reoperations for recurrent disease than in primary operations with extensive resection. One of the advantages of total thyroidectomy is to eliminate the potential of a more hazardous thyroid reoperation. There is usually no normal tissue in patients with multinodular disease. Therefore, if a surgeon leaves abnormal thyroid tissue in a patient with bilateral multinodular disease, subsequent reoperation might be required [20]. Reoperations are undertaken if there is postoperative histologic evidence of thyroid carcinoma or uninodular/multinodular recurrent goiter during further follow-up and they are associated with higher complication rates compared with the primary procedures [1–3, 14, 17–20, 22]. RLN palsy rates depend on a surgeon’s patient volume, the type of thyroidectomy, and definition. Reeve et al. [2] documented that there was no permanent RLN palsy and permanent hypoparathyroidism in 115 primary total thyroidectomies, whereas the rate of permanent RLN palsy and permanent hypoparathyroidism increased to 3.1 and 3.7% respectively, after secondary thyroidectomy for multinodular goiter in 258 patients. Menegaux et al. [23] documented in 203 thyroid reoperations for benign thyroid disease that the permanent complication rate was higher in thyroid reoperations than in primary thyroid operations. In present study, we documented a significant increase in transient hypoparathyroidism in patients who underwent total or near-total thyroidectomy in comparison to the patients who had subtotal thyroidectomy (1.42% vs. 8.4%; p < 0.001 and 0.3% vs. 1.07%; p < 0.008). However, there was no significant difference for transient and permanent RLN palsy or permanent hypoparathyroidism in patients treated by either subtotal or total thyroidectomy. With experience in the surgical technique, total thyroidectomy has been recommended not only for the management of thyroid carcinoma, but also for BMNG, because total thyroidectomy is an appropriate approach to prevent recurrence of multinodular disease [6].
Bilateral subtotal thyroidectomy has been recommended as the preferred surgical treatment for multinodular goiter, and it was claimed that total thyroidectomy added an unnecessary risk of complications to patients with BMNG [3, 24]. The use of thyroid hormone supplementation has been suggested to efficiently prevent recurrence [24, 25]. Although postoperative thyroxine treatment reduced the rate of recurrence, limited unilateral procedures were associated with a high rate of recurrence [24]. The recurrence rate after subtotal resection is high, and the preventive effect of postoperative thyroid hormone therapy is highly questionable [25, 26]. We recommend postoperative nonsuppressive doses of thyroxine therapy to our patients treated by subtotal thyroidectomy. The incidence of recurrence has been directly related to a long postoperative follow-up period and to large amounts of remnant tissue [24–27]. Although some authors recommend 30 years of follow-up to determine the actual outcome, most of the recurrences developed 10–20 years after the primary surgery [3, 24–27]. Delbridge et al. [3] documented that subtotal thyroidectomy for multinodular goiter has resulted in reoperation for recurrence in 13–20% of patients, reaching a peak incidence 13 years after the primary operation. In the present study, the follow-up period was between 1 and 19 years and the mean time to postoperative recurrence was 11.7 years. The recurrence rate was 7.1% in patients with BMNG treated initially by subtotal thyroidectomy. However, secondary surgical therapy has been indicated in only 5% of those patients. These results might be associated with the fact that the subtotal thyroidectomies were performed mostly for large multinodular disease with the goal of removing all of the nodules and to leave a small thyroid remnant of less than 5 g and to use postoperative L-thyroxine therapy.
RAI ablation was found to be an important factor in prolonging the disease-free interval and survival in patients with well-differentiated thyroid carcinoma, even in low-risk patients [28–33]. Completion thyroidectomy should be performed in patients with incidentally found thyroid carcinoma if the histologic criteria mandate RAI ablation and there is a large volume of thyroid remnant. In the present study, 38 patients with thyroid carcinoma incidentally found after subtotal thyroidectomy underwent completion thyroidectomy as a result of an indication of radioiodine ablation therapy. It is preferred that TSH level be higher than 30 mIU/l for effective RAI ablation [34]. We performed completion thyroidectomy in patients with thyroid carcinoma who were treated initially by subtotal thyroidectomy for BMNG because postoperative TSH values of these patients were significantly lower than those of patients with thyroid carcinoma treated initially by total thyroidectomy for BMNG (p < 0.01). Thyroid carcinoma might be detected in approximately 10% of thyroidectomy specimens of recurrent goiter, although the preceding operations were performed for benign goiter [23]. Menegaux et al. [23] documented that 20% of such patients had multifocal cancer, lymph node metastasis, or distant metastasis. In the present study, we found that 5.26% of patients who had completion thyroidectomy had thyroid papillary microcarcinoma on their remnant thyroid tissue.
In conclusion, the incidence of thyroid carcinoma in patients with BMNG without any previous suspicion of malignancy was found to be 7.6%. Subtotal thyroidectomy resulted in a significantly higher rate of completion thyroidectomy for incidentally diagnosed thyroid carcinoma compared with total or near-total thyroidectomy. Total thyroidectomy for BMNG is safe and effective when performed by an experienced surgeon because the extent of surgical resection had no significant effect on the rate of permanent complications. We recommend total or near-total thyroidectomy in BMNG to prevent recurrence and to eliminate the necessity for early completion thyroidectomy in case of a final diagnosis of thyroid carcinoma if the entire gland is involved.
References
Siragusa G, Lanzara P, Di Pace G (1998) Subtotal thyroidectomy or total thyroidectomy in the treatment of benign thyroid disease: our experience [in Italian]. Minerva Chir 53:233–238
Reeve TS, Delbribge L, Cohen A, Crummer P (1987) Total thyroidectomy: the preferred option for multinodular goiter. Ann Surg 206:782–786
Delbridge L, Guinea AI, Reeve TS (1999) Total thyroidectomy for bilateral benign multinodular goiter: effect of changing practice. Arch Surg 134:1389–1393
Jacobs JK, Aland JW Jr, Ballinger JF (1983) Total thyroidectomy: a review of 213 patients. Ann Surg 197:542–549
Pappalardo G, Guadalaxara A, Frattaroli FM, Illomei G, Falaschi P (1998) Total compared with subtotal thyroidectomy in benign nodular disease: personal series and review of published reports. Eur J Surg 164:501–506
Liu Q, Djuricin G, Prinz RA (1998) Total thyroidectomy for benign thyroid disease. Surgery 123:2–7
Mishra A, Agarwal A, Agarwal G, Mishra SK (2001) Total thyroidectomy in benign thyroid disorders in an endemic region. World J Surg 25:307–310
Gough IR, Wilkinson D (2000) Total thyroidectomy for management of thyroid disease. World J Surg 24:962–965
Wheeler MH (1998) Total thyroidectomy for benign thyroid disease. Lancet 351:1526–1527
Reeve TS, Delbridge L, Brady, Crummer P, Smyth C (1988) Secondary thyroidectomy: a twenty-year experience. World J Surg 12:449–453
Pezzullo L, Delrio P, Losito NS, Caraco C, Mozzillo N (1997) Post-operative complications after completion thyroidectomy for differentiated thyroid cancer. Eur J Surg Oncol 23:215–218
Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP (1998) Morbidity of thyroid surgery. Am J Surg 176:71–75
Wilson DB, Staren ED, Prinz RA (1998) Thyroid reoperations: indications and risks. Am Surg 64:674–678
Beahrs OH, Vandertoll DJ (1963) Complications of secondary thyroidectomy. Surg Gynecol Obstet 117:535–539
McCall A, Jarosz H, Lawrence AM, Paloyan E (1986) The incidence of thyroid carcinoma in solitary cold nodules and in multinodular goiters. Surgery 100:1128–1132
Koh KBH, Chang KW (1992) Carcinoma in multinodular goitre. Br J Surg 79:266–267
Chao TC, Jeng LB, Lin JD, Chen MF (1997) Reoperative thyroid surgery. World J Surg 21:644–647
Gould EA, Hirsch E, Brecher I (1965) Complications arising in the course of thyroidectomy. Arch Surg 90:81–85
Foster RS Jr (1978) Morbidity and mortality after thyroidectomy. Surg Gynecol Obstet 146:423–429
Thomusch O, Machens A, Sekulla C et al (2000) Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 24:1335–1341
Giles Y, Boztepe H, Terzioglu T, Tezelman S (2004) The advantage of total thyroidectomy to avoid reoperation for incidental thyroid cancer in multinodular goiter. Arch Surg 139:179–182
Calabro S, Auguste LJ, Attie JN (1988) Morbidity of completion thyroidectomy for initially misdiagnosed thyroid carcinoma. Head Neck Surg 10:235–238
Menegaux F, Turpin G, Dahman M, Leenhardt L, et al (1999) Secondary thyroidectomy in patients with prior thyroid surgery for benign disease: a study of 203 patients. Surgery 125:479–483
Anderson PE, Hurley PR, Rosswick P (1990) Conservative treatment and long term prophylactic thyroxine in the prevention of recurrence of multinodular goiter. Surg Gynecol Obstet 171:309–314
Kraimps JL, Marechaud R, Gineste D et al (1993) Analysis and prevention of recurrent goiter. Surg Gynecol Obstet 176:319–322
Piraneo S, Vitri P, Galimberti A, Salvaggio A, Bastagli A (1997) Ultrasonographic surveillance after surgery for euthyroid goitre in patients treated or not with thyroxine. Eur J Surg 163:21–26
Rojdmark J, Jarhult J (1995) High long term recurrence rate after subtotal thyroidectomy for nodular goitre. Eur J Surg 161:725–727
Maxon HR, Englaro RE, Thomas SR et al (1992) Radioiodine-131 therapy for well-differentiated thyroid cancer—a quantitative radiation dosimetric approach: outcome and validation. J Nucl Med 33:1132–1136
Hay ID, Bergstralh EJ, Goellner JR, Ebersold, Grant CS (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1058
Mazzaferri EL (1987) Papillary thyroid carcinoma: factors influencing prognosis and current therapy. Semin Oncol 14:315–322; erratum in Semin Oncol 1988; 15(3):x
Shah JP, Loree TR, Dharker D, Strong EW, Begg C, Vlamis V (1992) Prognostic factors in differentiated carcinoma of the thyroid gland. Am J Surg 164:658–661
Baudin E, Travagli JP, Ropers J et al (1998) Microcarcinoma of the thyroid gland: the Gustave-Roussy Institute experience. Cancer 83:553–559
Samaan NA, Schultz PN, Hickey RC et al (1992) The results of various modalities of treatment of well differentiated thyroid carcinoma: a retrospective review of 1599 patients. J Clin Endocrinol Metab 75:714–720
Logue JP, Tsang RW, Brierley JD, Simpson WJ (1994) Radioiodine ablation of residual tissue in thyroid cancer: relationship between administered activity, neck uptake and outcome. Br J Radiol 67:1127–1131
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tezelman, S., Borucu, I., Senyurek (Giles), Y. et al. The Change in Surgical Practice from Subtotal to Near-Total or Total Thyroidectomy in the Treatment of Patients with Benign Multinodular Goiter. World J Surg 33, 400–405 (2009). https://doi.org/10.1007/s00268-008-9808-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9808-1