Abstract
Background
Bone mineral density is one parameter used to decide whether patients with primary hyperparathyroidism (PHPT) should undergo parathyroidectomy. However, the influence of bone mineral density and parathyroidectomy on subsequent fracture risk is unclear.
Methods
The authors conducted a retrospective cohort study of patients with PHPT based on administrative discharge abstract data. The dual energy x-ray absorptiometry (DEXA) scan T-scores at the femur were collected by chart review, and 10-year fracture-free survival (FFS) was the main outcome measured.
Results
A total of 533 patients were identified, most of them ≥ 50 years old (89%) and female (87%). Seventeen percent of the patients were black. Mean initial calcium, parathormone, and creatinine levels were 11.1 mg/dl, 116 pg/ml, and 0.9 mg/dl, respectively. Parathyroidectomy was performed in 159 (30%) patients, and 374 (70%) were observed. The 10-year FFS after PHPT diagnosis was 94% in patients treated with parathyroidectomy and 81% in those observed (p = 0.006). Compared to observation, parathyroidectomy improved the 10-year FFS by 9.1% (p = 0.99), 12% (p = 0.92), and 12% (p = 0.02) in patients with normal bones (T-score ≥ −1.0), osteopenia (T-score ≤ −1.0, ≥ −2.5), and osteoporosis (T-score < −2.5), respectively. On multivariate analysis, parathyroidectomy was independently associated with decreased fracture risk (HR = 0.41; 95%CI 0.18, 0.93), whereas non-black race (HR = 2.94; 95%CI 1.04, 8.30) and T-score < −2.5 (HR = 2.29; 95%CI 1.08, 4.88) remained independently associated with increased fracture risk.
Conclusions
Parathyroidectomy decreases the risk of fracture in patients with normal, osteopenic, and osteoporotic bones. The largest impact from parathyroidectomy is in patients with osteoporosis. The highest risk of fracture is in non-blacks and in patients with osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (PHPT) is now commonly diagnosed in the asymptomatic stages of the disease. Worsening bone mineral density (BMD) is one indication for operative intervention. Current National Institutes of Health (NIH) guidelines recommend parathyroidectomy for patients with a T-score < 2.5 at the lumbar spine, hip, or wrist [1]. Parathyroidectomy has been found to halt bony deterioration and even improve BMD [2−5]. Even more important, parathyroidectomy may reduce the risk of fracture in patients with PHPT [6, 7].
In 2006, in a retrospective study based on a large population database, we reported that in patients with PHPT parathyroidectomy, as compared to observation, reduced the risk of fracture, regardless of age, calcium, or parathormone level [7]. A criticism of the study was the lack of information regarding BMD and its effect on risk of fracture.
Therefore, the objective of this study was to update our published data and attempt to determine the influence of BMD together with parathyroidectomy on fracture risk in patients with primary hyperparathyroidism.
Methods
Data sources and study cohort
We used the cohort of patients with primary hyperparathyroidism previously defined in our published article [7]. The dual energy x-ray absorptiometry (DEXA scan) T-score at the femur was then abstracted from the medical record. This study was approved by the Institutional Review Board of Kaiser Permanente Southern California, protocol number 4422.
Definition of fracture
The Permanente Discharge Abstract Database was used to identify patients who were hospitalized with the outcome variable of fracture [hip fracture (ICD-9 code 820); spine fracture (ICD-9 codes 805, 806); pelvis fracture (ICD-9 code 808); upper extremity fracture (ICD-9 codes 812, 813); lower extremity fracture (ICD-9 codes 821, 823)] that occurred at least one day after the diagnosis of PHPT up to the study completion date of 31 May 2004.
Statistical analysis
The data were exported to SAS version 8 (SAS Institute, Inc. Cary, NC) statistical software for all analyses. Associations between predictor variables and fractures were assessed with Cox proportional hazards modeling. Variables analyzed for their influence on fractures were age (in categories ≤50, ≥50 years), gender, race, Charlson co-morbidity index (CCI) [8], T-score at the femur, calcium level, parathormone level, creatinine level, and whether parathyroidectomy was or was not performed. The strength of associations was expressed as hazard ratios (HR) and 95% confidence intervals (CI) for having a fracture. Multivariable Cox regression modeling was used to assess the independent effect of potential predictor variables, adjusting for the same variables used in the univariate analysis. Fracture-free survival time, estimated by the Kaplan–Meier method, was calculated as the time elapsed from the diagnosis of hyperparathyroidism until a fracture, last follow-up, or 31 May 2004, whichever came first. Fracture-free survival (FFS) curves were compared with the log rank test. The chi-square test was used to compare differences in categorical variables, and Wilcoxon signed rank test was used to compare differences in means between continuous variables. All p values reported were two-tailed.
Results
Patient demographics
Of the original 1,569 patients with primary hyperparathyroidism, 533 had femur T-score data. The majority of patients were women and older than 50 years of age. Most of the patients were of Caucasian race (65%), with 17% black, 4% Asian/Pacific Islander, and 14% other or unknown (Table 1). Mean initial calcium and PTH levels were 11.1 mg/dl and 116 pg/ml, respectively. Bone study revealed that 186 patients (35%) had normal bones (T-score ≥ −1.0), 232 patients (43%) had osteopenia (T-score ≤ 41.0, ≥ −2.5), and 115 patients (22%) had osteoporosis (T-score ≥ −2.5).
Parathyroidectomy versus observation
Parathyroidectomy was performed in 159 (30%) patients, and 374 (70%) patients were observed. Patients who were treated operatively were similar with regard to age, gender, and race, but were more likely to have higher calcium (p = 0.001) and PTH levels (p = 0.001) than patients who were observed. Furthermore, those who were observed were more likely to have osteoporosis (p = 0.018) (Table 2).
Fractures
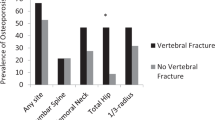
Patients were followed for an average of 7.4 years (range: 13 days to 10 years). In the course of the study period 59 patients experienced fractures: 14 of the hip, 12 of the spine, 6 of the pelvis, and 33 of bones in the upper extremities. Patients with normal bones (T-score ≥ −1.0) had a 10-year FFS of 92%, compared with 85% in patients with osteopenia (T-score ≤ −1.0, ≥ −2.5) and 72% in patients with osteoporosis (T-score ≥ −2.5) (Fig. 1).
The overall 10-year FFS after the diagnosis of PHPT was 94% in patients treated with parathyroidectomy compared to 81% in those who were observed [Hazard Ratio (HR) = 0.35; 95% CI 0.17, 0.74; p = 0.006] (Fig. 2). Parathyroidectomy increased the 10-year FFS by 9.1% (p = 0.99), 12% (p = 0.92), and 12% (p = 0.02) in patients with normal bones (T-score ≥ −1.0), osteopenia (T-score ≤ −1.0, ≥ −2.5), and osteoporosis (T-score < −2.5), respectively (Figs. 3–5). Osteoporosis (HR = 3.67; 95% CI 1.79, 7.51) and non-black race (HR = 2.46; 95% CI 0.98, 6.15) were associated with an increased risk of fracture, whereas age, gender, and initial calcium levels were not (Table 3).
Multivariate analysis confirmed that parathyroidectomy was independently associated with a decreased fracture risk (HR = 0.41; 95% CI 0.18, 0.93; p = 0.03) after accounting for all other variables. Osteoporosis (HR = 2.29; 95% CI 1.07, 4.88; p = 0.03) and non-black race (HR = 2.94; 95% CI 1.04, 8.30; p = 0.04) remained independently associated with increased fracture risk. Age ≥ 50, gender, and calcium level were not independently associated with fracture risk (Table 3).
Discussion
Parathyroidectomy reduced the 10-year risk of fracture in patients with primary hyperparathyroidism by 13%. Patients with evidence of osteoporosis, as measured by bone mineral density, had the greatest risk of fracture, and in these patients, 10-year FFS was improved by 12% in those who had parathyroidectomy. Black patients were found to have a decreased risk of fracture when compared to non-black patients, regardless of BMD.
The limitations of this study have been previously addressed and include its retrospective design [7]. Additionally, there may be a selection bias within the study given the method of patient selection, as BMD data were not available for all patients identified with PHPT. Finally, we did not evaluate the use of bisphosphonate therapy in this population, although these medications have been suggested in the nonoperative management of PHPT [9–11].
Current NIH and American Association of Clinical Endocrinologists American Association of Endocrine Surgeons (AACE/AAES) guidelines for the treatment of PHPT recommend parathyroidectomy in patients with a T-score ≤ 2.5 [1]. In this study, patients with osteoporosis and osteopenia, as measured by T-score at the femur, were at increased risk of fracture compared to patients with normal bones. Our findings confirm that DEXA scan is a useful screening tool to help predict fracture risk in patients with PHPT, just as it has been used in the geriatric and osteoporotic population [12].
Even more important, however, are the findings that parathyroidectomy was independently associated with a decreased risk of fracture and that all patients, regardless of bone density, had a decreased risk of fracture following parathyroidectomy. Therefore, while measuring BMD may serve as an appropriate method of risk-stratifying patients, is should not be used as a guideline for parathyroidectomy. Our study suggests that all patients with PHPT be offered parathyroidectomy, regardless of underlying BMD.
Recently, two randomized controlled trials have been published comparing parathyroidectomy to observation in patients with asymptomatic PHPT and the effect on BMD and quality of life. Bollerslev et al. found that patients that underwent parathyroidectomy had significant improvement in BMD at the lumbar spine but minimal change in quality of life (QoL) measurements. Patients who did not have parathyroidectomy continued to have stable BMD but had a slightly decreased QoL [13]. Ambrogini et al. found that while the observed patients had stable BMD and QoL measurements, those who underwent parathyroidectomy had significantly improved BMD and QoL [14]. While these studies suggest it is reasonable to observe asymptomatic PHPT patients closely, there are benefits to proceeding with parathyroidectomy, even in asymptomatic patients.
Our study suggests that patients with PHPT should be offered parathyroidectomy, regardless of age, calcium levels, or bone mineral density. This is contrary to current consensus recommendations, and like other authors, we question whether the NIH guidelines are too narrow [15]. Additionally, a recent cost analysis study emphasizes the importance of early parathyroidectomy, demonstrating that parathyroidectomy is cost-saving compared to observation and serial monitoring of patients with PHPT [16]. This cost data further underscores the need to consider parathyroidectomy in all patients with PHPT.
In conclusion, parathyroidectomy reduced the risk of fracture in all patients with primary hyperparathyroidism, when compared with observation. Parathyroidectomy should be offered to all patients with PHPT, regardless of age, calcium level, or bone mineral density.
References
AACE/AAES Task Force on Primary Hyperparathyroidism (2005) AACE/AAES position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract 11:49–54
Rao DS, Wallace EA, Antonelli RF et al (2003) Forearm bone density in primary hyperparathyroidism: long-term follow-up with and without parathyroidectomy. Clin Endocrinol (Oxf) 58:348–354
Nordenstrom E, Westerdahl J, Bergenfelz A (2004) Recovery of bone mineral density in 126 patients after surgery for primary hyperparathyroidism. World J Surg 28:502–507
Hagstrom E, Lundgren E (2006) Positive effect of parathyroidectomy on bone mineral density in mild asymptomatic primary hyperparathyroidism. J Intern Med 259:191–198
Almqvist EG, Becker C, Bondeson AG et al (2004) Early parathyroidectomy increases bone mineral density in patients with mild primary hyperparathyroidism: a prospective and randomized study. Surgery 136:1281–1288
Vestergaard P, Mosekilde L (2004) Parathyroid surgery is associated with a decreased risk of hip and upper arm fractures in primary hyperparathyroidism: a controlled cohort study. J Intern Med 255:108–114
VanderWalde LH, Liu IL, O’Connell TX et al (2006) The effect of parathyroidectomy on bone fracture risk in patients with primary hyperparathyroidism. Arch Surg 141:885–889
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Cummings SR, Black DM, Karpf DB et al (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 280:2077–2082
Khan AA, Bilezikian JP, Kung AW et al (2004) Alendronate in primary hyperparathyroidism: a double-blind, randomized, placebo-controlled trail. J Clin Endocrinol Metab 89:3319–3325
Horiuchi T, Onouchi T, Inoue J et al (2002) A strategy for the management of elderly women with primary hyperparathyroidism: a comparison of etidronate therapy with parathyroidectomy. Gerontology 48:103–108
Kern LM, Powe NR, Levine MA et al (2005) Association between screening for osteoporosis and the incidence of hip fracture. Ann Intern Med 142:173–181
Bollerslev J, Jansson S, Mollerup CL et al (2007) Medical observation, compared with parathyroidectomy, for asymptomatic primary hyperparathyroidism: a prospective, randomized trial. J Clin Endocrinol Metab 92:1687–1692
Ambrogini E, Cetani F, Cianferotti L et al (2007) Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial. J Clin Endocrinol Metab 92:3114–3121
Eigelberger MS, Cheah WK, Ituarte PH et al (2004) The NIH criteria for parathyroidectomy in asymptomatic primary hyperparathyroidism: are they too limited? Ann Surg 239:528–535
Zanacco K, Angelos P, Sturgeon C (2006) Cost-effectiveness analysis of parathyroidectomy for asymptomatic primary hyperparathyroidism. Surgery 140:874–882
Acknowledgement
The senior author Philip I. Haigh would like to dedicate this manuscript to Orlo H. Clark, a mentor, colleague, friend, and master endocrine surgeon.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
VanderWalde, L.H., Liu, IL.A. & Haigh, P.I. Effect of Bone Mineral Density and Parathyroidectomy on Fracture Risk in Primary Hyperparathyroidism. World J Surg 33, 406–411 (2009). https://doi.org/10.1007/s00268-008-9720-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9720-8