Abstract
Background
The 6th edition TNM staging (TNM-6) for hepatocellular carcinoma (HCC) has been recommended. However, its superiority, in contrast to the previous 5th edition (TNM-5), has not been fully recognized. Besides, tumor differentiation was not included. The current study was designed to compare the value of these two staging systems and, more importantly, to elucidate whether Edmondson-Steiner grading, a well-acknowledged histological classification, is helpful in further discriminating different prognosis of HCC.
Methods
Prospectively collected clinicopathological and follow-up data of consecutive 171 patients with HCC undergoing curative hepatic resection (CHR) were reviewed retrospectively. The impacts of variables on survival were determined by univariate and multivariate statistical analyses.
Results
The differences of survival between stages of the TNM-6 and TNM-5 were almost significant, except for disease-free survival for TNM-5. Moreover, TNM-6 might be a more powerful prognostic predictor compared with TNM-5, although their impacts on survival were all not independent, unlike Edmondson-Steiner grading. For patients with each stage of TNM-6, Edmondson-Steiner grade was the sole significant variable in both univariate and multivariate analyses. Finally, a novel scoring criteria (prognostic scoring for CHR, PSCHR) integrating Edmondson-Steiner grading and TNM-6 was attempted and statistically shown to be of independent significance and stronger predicting value for prognosis of curatively resected HCC.
Conclusion
TNM-6 revealed to be more significantly prognostic than TNM-5 in patients with HCC after curative hepatic resection. Edmondson-Steiner grading could raise the predictive efficiency of TNM-6 for postresectional survival of patients with HCC. Therefore, PSCHR containing Edmondson-Steiner grading was preliminarily proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) has long been regarded as one of the human malignant tumors with high incidence and poor prognosis [1, 2]. In accordance with the recent report, HCC has been the sixth most common cancer worldwide in terms of numbers of cases and the third most common cause of death from cancer [3]. So far, the outcome of HCC remains dismal. To direct treatment more effectively and predict long-term prognosis more accurately, many efforts have been focused on staging for HCC for several decades. These staging systems included Primack staging [4], Okuda staging [5], the Cancer of the Liver Italian Program (CLIP) score [6], the Barcelona Clinic Liver Cancer (BCLC) staging [7], the Chinese University Prognostic Index [8], and the Japan Integrated Staging (JIS) Score [9]. Besides, tumor-node-metastasis (TNM) staging [10] by American Joint Committee on Cancer (AJCC)/International Union Against Cancer (UICC) has been acknowledged as widely used and authoritative and was shown to be superior to some other staging systems by some authors [11]. However, other investigators supported the opposite opinion [12]. Recently, the 6th edition TNM staging (TNM-6) was introduced [13], based on the proposal of Vauthey et al [14]. The main differences between TNM-5 and TNM-6 were almost for T categories, such as the weakened impact and the different cutoff value of tumor size. It was indicated that TNM-6 was simpler and revealed higher prognostic power than TNM-5 [15–17]. Most recently, a novel modified TNM-6 and The Liver Cancer Study Group (LCSG) staging have been suggested [18, 19]. Certainly, further studies are expected.
The above-mentioned staging systems mainly considered clinicopathological factors that were revealed to influence prognosis of HCC, such as tumor size, number of nodules, vascular invasion, and liver function status [20–22]. However, what calls for special attention is that differentiation grade, which has been shown to be of comprehensive prognostic significance for HCC patients undergoing different kinds of therapies, including hepatic resection, orthotopic liver transplantation, percutaneous ethanol injection, radiofrequency (RF) ablation, acetic acid injection, and microwave coagulation [23–31], has not been enrolled in any previous staging system. On the basis of our previous works, which discussed prognosis in several subsets of liver cancer patients and suggested the strong prognostic impact of tumor differentiation [32–36], the present study was designed to compare the predicting values of TNM-5 and TNM-6 for prognosis of HCC and investigate whether Edmondson-Steiner grading [37], an authorized and extensively used histological classification [23, 29–31, 38], is helpful for more accurate prognosis discrimination, based on a Chinese cohort of patients with HCC undergoing curative hepatic resection.
Patients and methods
Characteristics of patients
A total of 171 consecutive patients with hepatocellular carcinoma (HCC) who underwent curative hepatic resection and accepted follow-up at least one time were recruited. They were hepatomized between January 1995 and December 2002. The patients were selected in accordance with the following criteria: 1) solitary or multiple tumors (no more than 3) were limited with at least 2 segments free of lesion; 2) no evidence of tumor thrombus in the trunk of portal vein; 3) no evidence of extrahepatic metastasis; and 4) Child-Pugh grading was not worse than class B. Three patients who died of hepatic failure perioperatively were excluded. Among the patients enrolled, 149 (87.1%) were men and 22 (12.9%) were women. Ages ranged from 15 to 77 (mean ± SD, 50.7 ± 12) years. Hepatitis B surface antigen (HBsAg) was positive in 142 patients (83%) and negative in 29 (17%). There were 138 cases (80.7%) with liver cirrhosis and 33 (19.3%) without; 156 patients (91.2%) were grade A and 15 (8.8%) were grade B of Child-Pugh’s classification before surgical procedures. Serum α-fetoprotein (AFP) was greater than 400 ng/ml in 62 patients (36.3%) and lower than the level in 109 patients (63.7%). Tumor sizes, defined as the largest dimension for solitary masses and the size of the largest tumor for multiple masses, ranged from 0.7 to 30 (mean ± SD, 7.8 ± 4.8) cm; 116 patients (67.8%) had tumors at least 5 cm in size. Nineteen cases (11.1%) developed portal vein tumor thrombosis (PVTT), which was defined as cancer involvement in the main branches of portal vein. Based on postoperative examinations, microvascular invasion was histologically detected in 62 patients (36.3%). Macroscopic satellite nodules, one kind of intrahepatic metastasis that was close to the main tumor, also were present in 19 patients. Pathological grading, according to Edmondson-Steiner criteria that considered the characteristics, such as size, morphology, and mitotic figures, of HCC cells to reflect the differentiation of the tumor [37] was mainly given by a pathologist (DXY) and showed that numbers of patients with grades I, II, III, and IV were 19 (11.1%), 72 (42.1%), 61 (35.7%), and 19 (11.1%), respectively. There was a statistical relationship between tumor size and tumor grading (grade III-IV/I-II: 63/53 in tumors ≥ 5 cm and 17/38 in those < 5 cm, χ2 = 7.294; P = 0.007). Two cases (1.2%) had well-differentiated early HCC of < 2 cm.
Patient distribution according to TNM-5, TNM-6, and prognostic scoring for curative hepatic resection (PSCHR) and criteria for PSCHR
According to TNM-5 [10], 4, 69, 61, and 37 patients were classified as stage I, II, III, and IVA, respectively. Using TNM-6 staging system [13], 65, 59, and 47 patients were classified as stage I, II, and III. The criteria of these two editions of TNM staging were presented in Table 1. When Edmondson-Steiner grading was considered as a supplemented variable, prognostic scoring for curative hepatic resection (PSCHR) was preliminarily proposed and shown in Table 2. Forty-six, 51, 40, and 34 patients were divided into score 1, 2, 3, and 4, respectively. However, what calls for special attention is that no patients were stage IVB of TNM-5 or stage IV of TNM-6, because none of them developed distant metastasis before surgery.
Identification of clinical and pathological variables
Thirteen variables that might influence prognosis of HCC were selected to be estimated parameters for statistical analyses, including those related to general situation, hepatic underlying diseases, and tumor-associated factors, such as age, sex, HBsAg, HCV, liver cirrhosis, Child-Pugh grading, Serum AFP value, tumor size, PVTT, microvascular invasion, satellite nodule, Edmondson-Steiner grading, and different editions of TNM staging or PSCHR.
Follow-up
All patients were enrolled in our strict follow-up system, with intervals ranging 1 to 3 months. Imaging examinations, such as B-type ultrasonography (BUS), computed tomography (CT), magnetic resonance imaging (MRI) and angiography, and AFP level were used in monitoring disease progression. Follow-up terms ranged from 3 to 108 (median, 37) months and ended in December 2003.
Statistical analyses
Survival curves were calculated by Kaplan-Meier method and compared by log-rank test. Cox regression (proportional hazard model) was adopted for multivariate analysis. Log-rank test was used for evaluating homogeneity. Higher log-rank value indicated better homogeneity. Linear trend χ2 test was performed for estimating monotonicity of the gradient. Higher χ2 value meant better monotonicity. According to the method introduced by Chen et al. [39], the value of -2 log likelihood with in the Cox regression model was calculated for measuring the overall discriminatory ability of a staging model. A better stratifying model had a lower -2 log likelihood value. Statistical software package SPSS11.5 (SPSS Inc., Chicago, IL) was used for all analyses. Statistical significance was defined as P < 0.05.
Results
Impacts of TNM-5, TNM-6, and PSCHR on overall and disease-free survival of HCC patients after curative resection
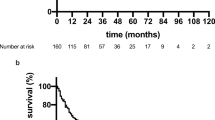
As shown in Fig. 1 and Table 3, log-rank test established almost all prognostic implications of TNM-5, TNM-6, and PSCHR (P < 0.05), except for TNM-5 for disease-free survival (P > 0.05). In Cox regression analysis, TNM-5 and TNM-6 were all not identified as independent prognostic factors (P > 0.05; Table 4). However, the independent role of PSCHR, in which Edmondson-Steiner grading was included, was revealed for both overall and disease-free survival (P < 0.05; Table 4).
Survival curves in accordance with various editions of TNM staging for HCC. (a) and (b) TNM-5 for overall and disease-free survival (stage I, black solid line, n = 4; stage II, gray solid line, n = 69; stage III, black dashed line, n = 61; stage IVA, gray dashed line, n = 37; P = 0.0007 and 0.1756, respectively). (c) and (d) TNM-6 for overall and disease-free survival (stage I, black solid line, n = 65; stage II, gray solid line, n = 59; stage III, black dashed line, n = 47; P < 0.0001 and 0.0001, respectively). (e) and (f) PSCHR for overall and disease-free survival (score 1, black solid line, n = 46; score 2, gray solid line, n = 51; score 3, black dashed line, n = 40; score 4, gray dashed line, n = 34; P < 0.0001 and 0.0001, respectively)
Other factors predictive for prognosis of HCC patients after curative resection
Five clinicopathological variables, including AFP > 400 ng/ml, higher Edmondson-Steiner grading, presence of microvascular invasion, PVTT, and satellite nodule were shown to be associated with shorter overall and disease-free survival of HCC patients after curative hepatic resection by univariate analysis. Meanwhile, tumor size ≥ 5 cm affected overall survival only. In Cox regression tests enrolling TNM-5 and TNM-6, respectively, Edmondson-Steiner grading was the sole independent predictor of overall and disease-free survival for both. Besides, satellite nodule independently influenced prognosis when enrolling TNM-5. In addition, no other independent prognostic marker for overall or disease-free survival was found when PSCHR was introduced (Table 4).
Stage-specific prognostic predictors of TNM-6 and TNM-5 staging systems for HCC patients after curative resection
According to univariate analysis, Edmondson-Steiner grading was the only predictor for both overall and disease-free survival of each stage of TNM-6 (Fig. 2). Serum AFP level and microvascular invasion significantly impacted overall and disease-free survival of patients with stage II disease. Edmondson-Steiner grading was further identified by multivariate analysis as an independent prognostic determinant of each stage of TNM-6 (Table 5). Furthermore, Edmondson-Steiner grading was of independent prognostic significance for stage II, III, and IVA of TNM-5, although its role in stage I was difficult to evaluate because of the small case amount (data not shown).
Impact of Edmondson-Steiner grading on postresectional survival of different TNM-6 stages of HCC. (a) and (b) Overall and disease-free survival of stage I (grade I and II, black solid line, n = 46; grade III and IV, gray solid line, n = 19; P < 0.0001 and 0.0001, respectively). (c) and (d) Overall and disease-free survival of stage II (grade I and II, black solid line, n = 32; grade III and IV, gray solid line, n = 27; P < 0.0001 and 0.0001, respectively). (e) and (f) Overall and disease-free survival of stage III (grade I and II, black solid line, n = 13; grade III and IV, gray solid line, n = 34; P = 0.0222 and 0.0021, respectively)
Evaluation of TNM-5, TNM-6, and PSCHR on HCC patients after curative resection
As shown in Table 6, the log rank and linear trend χ2 values for overall and disease-free survival gradually increased from TNM-5 to PSCHR. In contrast, PSCHR possessed lowest -2 log likelihood values, which meant highest discriminatory ability for both overall and disease-free survival compared with TNM-6 and TNM-5.
Discussion
Hepatocellular carcinoma, a lethal malignancy, has increased its incidence and mortality rate worldwide [1, 2]; and 55% of cases and deaths are in China alone [3]. Thus far, many efforts focused on the establishment of a satisfactory staging system for HCC to direct treatment and predict prognosis more accurately [4–9], including the suggestion based on Chinese patients [8]. However, TNM staging has been extensively used [10]. It was greatly controversial for the comparison of TNM and some newly developed staging systems in reliability and accuracy of survival prediction for HCC [8, 11, 12]. Since TNM-6 was proposed and recommended [13, 14], its advantages compared with TNM-5, such as convenience and predicting power for prognosis, has been described by some authors [15–17]. In the present study, we consented to the opinion based on comprehensive evaluation for these two staging systems in homogeneity, monotonicity of the gradient, and overall discriminatory ability (Fig. 1; Tables 4 and 6). Of course, all aforementioned agreements focused on resected patients with HCC. Some investigators have shown that TNM-6 failed to predict survival of patients after orthotopic liver transplantation [40]. Therefore, the predictive power of TNM-6 for a wider range of patients with HCC remains to be elucidated.
Although modification for TNM-6 and a new T classification have been recently reported [18, 19], all previous staging criteria, including different editions of TNM staging and those developed by different authors, has not included a potentially significant variable for prognosis of HCC, namely differentiation grade [4–10, 13, 18, 19]. In fact, differentiation status was long proven to be of prognostic significance for HCC patients who underwent a wide range of treatments, such as resection, transplantation, and local regional ablative therapies [23–31, 34–36]. The findings that poorer differentiation was associated with higher proliferative and angiogenic activity, larger tumor size, more vascular invasion, higher ratio of AFP > 400 ng/ml, and those who needed major hepatic resection might account in part for the impact of differentiation on prognosis of HCC [23, 38, 41, 42]. However, it was regretted that such an easily understood and strong prognostic marker was not included in some previous investigations [20, 43]. In the current study, we first showed that the Edmondson-Steiner grade [37]—a well-acknowledged histological classification of HCC—was greatly helpful in stratifying different survival after curative hepatic resection for patients with each stage of TNM-6 (Fig. 2; Table 5). On the basis of this finding, a novel prognostic scoring system that integrated TNM-6 and Edmondson-Steiner grade (PSCHR; Table 2) was preliminarily attempted. In our cohort, it was found to be of better homogeneity, monotonicity of the gradient, and overall discriminatory ability than TNM-6 and TNM-5 (Table 6) after comprehensive estimation of these parameters. Therefore, PSCHR seemed to be of a higher prognostic efficiency for patients with HCC after curative resection. However, what needs to be specially noticed is the fact that the low resectability rate of HCC limited the applicability of PSCHR. Besides, the difficulty in evaluation of the system for patients undergoing local ablation therapies, which may still be curative but without histological data, also restricted its validation and application. Therefore, further verifications for this preliminary proposal based on patients who belonged to different subsets and were treated with different kinds of modality, if a preoperative biopsy could be performed, should be expected and welcomed, because a successful prognostic model should be suited to as many patients as possible.
Conclusion
Our data suggested that TNM-6 was an advantage for prognosis prediction in patients with HCC after curative hepatic resection compared with TNM-5. Edmondson-Steiner grading could effectively distinguish postresectional survival of patients with each TNM-6 stage of HCC. Therefore, PSCHR covering Edmondson-Steiner grading was shown to be a better prognostic model than TNM-6 and TNM-5 and was preliminarily recommended.
References
Parkin DM, Pisani P, Ferlay J (1993) Estimates of the worldwide incidence of eighteen major cancers in 1985. Int J Cancer 54:594–606
Pisani P, Parkin DM, Bray F, Ferlay J (1999) Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer 83:18–29
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Primack A, Vogel CL, Kyalwazi SK, Ziegler JL, Simon R, Anthony PP (1975) A staging system for hepatocellular carcinoma: prognostic factors in Ugandan patients. Cancer 35:1357–1364
Okuda K, Ohtsuki T, Obata H et al (1985) Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer 56:918–928
The Cancer of the Liver Italian Program (CLIP) Investigators (1998) A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients. Hepatology 28:751–755
Llovet JM, Bru C, Bruix J (1999) Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 19:329–337
Leung TW, Tang AM, Zee B et al (2002) Construction of the Chinese University Prognostic Index for hepatocellular carcinoma and comparison with the TNM staging system, the Okuda staging system, and the Cancer of the Liver Italian Program staging system: a study based on 926 patients. Cancer 94:1760–1769
Kudo M, Chung H, Osaki Y (2003) Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan integrated staging score (JIS score). J Gastroenterol 38:207–215
Fleming I, Cooper J, Hensen D (1997) Liver AJCC cancer staging manual. 5th edn. Lippincott-Raven, Philadelphia
Huang YH, Chen CH, Chang TT et al (2005) Evaluation of predictive value of CLIP, Okuda, TNM and JIS staging systems for hepatocellular carcinoma patients undergoing surgery. J Gastroenterol Hepatol 20:765–771
Farinati F, Rinaldi M, Gianni S, Naccarato R (2000) How should patients with hepatocellular carcinoma be staged? Validation of a new prognostic system. Cancer 89:2266–2273
Anonymous (2002) Liver including intrahepatic bile ducts. In: Greene F, Page D, Fleming I (eds) American Joint Committee on cancer staging manual. 6th edn. Springer, New York, pp 131–144
Vauthey JN, Lauwers GY, Esnaola NF et al (2002) Simplified staging for hepatocellular carcinoma. J Clin Oncol 20:1527–1536
Lei HJ, Chau GY, Lui WY et al (2006) Prognostic value and clinical relevance of the 6th Edition 2002 American Joint Committee on Cancer staging system in patients with resectable hepatocellular carcinoma. J Am Coll Surg 203:426–435
Ramacciato G, Mercantini P, Cautero N et al (2005) Prognostic evaluation of the new American Joint Committee on Cancer/International Union Against Cancer staging system for hepatocellular carcinoma: analysis of 112 cirrhotic patients resected for hepatocellular carcinoma. Ann Surg Oncol 12:289–297
Varotti G, Ramacciato G, Ercolani G et al (2005) Comparison between the fifth and sixth editions of the AJCC/UICC TNM staging systems for hepatocellular carcinoma: multicentric study on 393 cirrhotic resected patients. Eur J Surg Oncol 31:760–767
Kee KM, Wang JH, Lee CM et al (2007) Validation of clinical AJCC/UICC TNM staging system for hepatocellular carcinoma: analysis of 5,613 cases from a medical center in southern Taiwan. Int J Cancer 120:2650–2655
Minagawa M, Ikai I, Matsuyama Y, Yamaoka Y, Makuuchi M (2007) Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,772 patients in Japan. Ann Surg 245:909–922
Qiang L, Huikai L, Butt K, Wang PP, Hao X (2006) Factors associated with disease survival after surgical resection in Chinese patients with hepatocellular carcinoma. World J Surg 30:439–445
Shah SA, Greig PD, Gallinger S et al (2006) Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg 202:275–283
Martins A, Cortez-Pinto H, Marques-Vidal P et al (2006) Treatment and prognostic factors in patients with hepatocellular carcinoma. Liver Int 26:680–687
Tanigawa N, Lu C, Mitsui T, Miura S (1997) Quantitation of sinusoid-like vessels in hepatocellular carcinoma: its clinical and prognostic significance. Hepatology 26:1216–1223
Horigome H, Nomura T, Saso K, Itoh M (1999) Standards for selecting percutaneous ethanol injection therapy or percutaneous microwave coagulation therapy for solitary small hepatocellular carcinoma: consideration of local recurrence. Am J Gastroenterol 94:1914–1917
Tamura S, Kato T, Berho M et al (2001) Impact of histological grade of hepatocellular carcinoma on the outcome of liver transplantation. Arch Surg 136:25–30
Si MS, Amersi F, Golish SR et al (2003) Prevalence of metastases in hepatocellular carcinoma: risk factors and impact on survival. Am Surg 69:879–885
Roayaie S, Schwartz JD, Sung MW et al (2004) Recurrence of hepatocellular carcinoma after liver transplant: patterns and prognosis. Liver Transpl 10:534–540
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC (2004) Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma ≤4 cm. Gastroenterology 127:1714–1723
Kubo S, Tanaka H, Shuto T et al (2005) Clinicopathologic features and outcome after liver resection for hepatocellular carcinoma in patients with concurrent versus previous chronic hepatitis B. Surg Today 35:216–222
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC (2005) Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut 54:1151–1156
Qian YB, Zhang JB, Wu WZ et al (2006) P48 is a predictive marker for outcome of postoperative interferon-alpha treatment in patients with hepatitis B virus infection-related hepatocellular carcinoma. Cancer 107:1562–1569
Zhou L, Rui JA, Wang SB et al (2003) Multi-modal serial therapy for primary liver cancer in senile patients: a report of 153 cases. Zhonghua Zhong Liu Za Zhi 25:404–406
Qu Q, Rui JA, Wang SB et al (2006) Comparison of different clinical staging systems for hepatocellular carcinoma. Zhonghua Zhong Liu Za Zhi 28:155–158
Zhou L, Rui JA, Wang SB et al (2006) Clinicopathological features, post-surgical survival and prognostic indicators of elderly patients with hepatocellular carcinoma. Eur J Surg Oncol 32:767–772
Zhou L, Rui JA, Wang SB et al (2007) Factors predictive for long-term survival of male patients with hepatocellular carcinoma after curative resection. J Surg Oncol 95:298–303
Zhou L, Rui JA, Wang SB et al (2007) Outcomes and prognostic factors of cirrhotic patients with hepatocellular carcinoma after radical major hepatectomy. World J Surg 31:1782–1787
Edmondson HA, Steiner PE (1954) Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7:462–503
Suehiro T, Matsumata T, Itasaka H, Yamamoto K, Kawahara N, Sugimachi K (1995) Clinicopathologic features and prognosis of resected hepatocellular carcinomas of varied sizes with special reference to proliferating cell nuclear antigen. Cancer 76:399–405
Chen TW, Chu CM, Yu JC et al (2007) Comparison of clinical staging systems in predicting survival of hepatocellular carcinoma patients receiving major or minor hepatectomy. Eur J Surg Oncol 33:480–487
Zavaglia C, De Carlis L, Alberti AB et al (2005) Predictors of long-term survival after liver transplantation for hepatocellular carcinoma. Am J Gastroenterol 100:2708–2716
Wada H, Nagano H, Yamamoto H et al (2006) Expression pattern of angiogenic factors and prognosis after hepatic resection in hepatocellular carcinoma: importance of angiopoietin-2 and hypoxia-induced factor-1 alpha. Liver Int 26:414–423
Oishi K, Itamoto T, Amano H et al (2007) Clinicopathologic features of poorly differentiated hepatocellular carcinoma. J Surg Oncol 95:311–316
Le Treut YP, Hardwigsen J, Ananian P et al (2006) Resection of hepatocellular carcinoma with tumor thrombus in the major vasculature. A European case-control series. J Gastrointest Surg 10:855–862
Acknowledgements
The authors thank all of the colleagues of the Department of Pathology, Peking Union Medical College Hospital, who took part in determination of Edmondson-Steiner grading.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, L., Rui, JA., Ye, DX. et al. Edmondson-Steiner Grading Increases the Predictive Efficiency of TNM Staging for Long-term Survival of Patients with Hepatocellular Carcinoma After Curative Resection. World J Surg 32, 1748–1756 (2008). https://doi.org/10.1007/s00268-008-9615-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9615-8