Abstract
Background
Radical major hepatectomy (RMH) has been suggested as one of main options for cure of large/advanced hepatocellular carcinoma (HCC). However, its operative risk remains high and its effectiveness is still controversial, especially for patients with liver cirrhosis. The present study aims to investigate short- and long-term outcomes and to identify prognostic factors for cirrhotic patients with HCC after RMH.
Materials and Methods
Prospectively collected clinicopathological data of 81consecutive cirrhotic HCC patients who underwent RMH were reviewed retrospectively. The Kaplan-Meier method was adopted for evaluating long-term survival. Prognostic factors were identified by univariate and multivariate analyses.
Results
After RMH, perioperative mortality, overall morbidity, and life-threatening morbidity were 1.2%, 24.7%, and 12.3%, respectively. Overall and disease-free 5-year survival rates were 39.4% and 28.1%, respectively. Univariate analysis showed that presence of portal vein tumor thrombosis (PVTT) and satellite nodules, late TNM staging, high Edmondson-Steiner grading, and blood transfusion was associated with worsened prognosis. Of them, Edmondson-Steiner grading was identified as the sole independent prognostic factor for both overall and disease-free survival by multivariate analysis, whereas blood transfusion and the presence of PVTT independently predicted unfavorable overall or disease-free survival, respectively.
Conclusions
These data indicated that RMH was safe and appeared to be effective in treating cirrhotic patients with HCC. Some tumor-related and clinical variables influenced long-term outcome of these patients after RMH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It is well known that hepatocellular carcinoma (HCC) has been one of the most common and highest mortality cancers worldwide [1]. Hepatic resection, as the main curative option for treating this malignancy, has achieved highly satisfactory outcomes according to recent reports [2–4], especially for patients with small tumors [3]. However, a significant proportion of HCC patients have large tumors or multiple nodules and therefore need larger-volume hepatic resections to achieve this radical expectation. Major hepatectomy (MH) was virtually the only choice of radical therapies suitable for treatment of these HCCs. In fact, it has been reported that 76% of large HCCs require MH [5]. Nevertheless, disagreement still existed. First, different approaches to evaluating MH have been indicated by different authors [6, 7]; these different criteria for case selection might be part of the reason for the difference. Also, it is particularly important to note that two different definitions of MH (removal of at least 2 or 3 Couinaud segments [8)] have been applied in published articles [9, 10]. Second, surgery-related risk, often presented as perioperative morbidity and mortality rates, remains high, especially for patients with liver cirrhosis [10, 11].
Thus far, investigations designed to evaluate the role of MH in the treatment of HCC, and to define prognostic factors after MH, have not been adequate to the task [6, 7, 9–11]. Furthermore, these studies have not focused on cirrhotic patients with HCC after radical major hepatectomy (RMH), under a more extensive definition. Previously, we have discussed prognosis evaluation in some subgroups of liver cancer patients [12–14]. In the present study, we aim to clarify safety, effectiveness, and prognostic factors of RMH (removing at least 3 Couinaud segments, according to the recent consensus classification [15)] for cirrhotic patients with HCC.
Materials and Methods
Patients
From January 1995 to December 2002, we performed radical major hepatectomy (RMH) in 81 consecutive cirrhotic patients with HCC. As noted above, major hepatectomy was defined according to the consensus classification as removing at least three Couinaud segments. Radical hepatectomy was defined by the absence of remnant lesions immediately after surgery. Of our 81 patients, 76 (93.8%) were men and 5 (6.2%) were women. Ages ranged from 24 to 76 years (mean ± SD, 54.3 ± 11.0 years). Hepatitis B surface antigen (HBsAg) was positive in 72 patients (88.9%) and negative in 9 (11.1%). Seventy-five patients (92.6%) were preoperatively classified as grade A and 6 (7.4%) as grade B according to the Child-Pugh. A serum α-fetoprotein (AFP) level higher than 400 ng/ml was found in 45 patients (55.6%). Tumor sizes, defined as the largest dimension for solitary masses and the sum of the largest dimension of each mass for multiple masses, ranged from 4 to 30 cm (mean ± SD, 9.9 ± 4.5 cm). There were 73 patients (90.1%) with solitary tumors and 8 (9.9%) with multiple tumors. Sixty-six patients (81.5%) had tumors at least 5 cm in size. TNM staging [16] revealed that there were 18 patients in stage II, 41 in stage III, and 22 in stage IVA. Fourteen patients (17.3%) developed portal vein tumor thrombosis (PVTT), which was defined as macroscopic thrombi located in the main branches. Macroscopic satellite nodules were found in 10 patients (12.3%). Histological grading, according to Edmondson-Steiner criteria [17], showed that patients with grades I, II, III and IV numbered 10 (12.3%), 27 (33.3%), 30 (37.0%), and 14 (17.4%), respectively.
Preoperative evaluation and surgical procedures
The status of tumor masses was detected chiefly by image examinations, including B-type ultrasonography (B-US), computed tomography (CT), magnetic resonance imaging (MRI), and angiography. Liver function reserve was evaluated based on routine biochemical and coagulation tests, supplemented by the indocyanine green (ICG) test.
The procedures included right trisectionectomy in 16 patients, left trisectionectomy in 2, extended right hepatectomy in 10, extended left hepatectomy in 1, central hepatectomy in 2, right hepatectomy in 25, left hepatectomy in 11, combined resection of 3 Couinaud segments in 14. A cavitron ultrasonic surgical aspirator (CUSA system 200 Sonia Technology, Inc. Cheshire, CT, USA) was adopted for dissecting hepatic parenchyma. Intraoperative ultrasonography was used for ensuring negative margins, if necessary. All procedures were performed under normothermic continuous interruption of the porta hepatis. This interruption lasted 10–35 min (mean ± SD, 20.6 ± 5.9 min). Operating time ranged from 115 to 345 min (mean ± SD, 221 ± 51 min), and blood loss ranged from 300 to 2,600 ml (mean ± SD, 871 ± 547 ml). The amounts of blood transfusion ranged from 0 to 2,000 ml (mean ± SD, 625 ± 463 ml), and 35 patients (43.2%) did not require homologous blood transfusion during RMH.
Follow-up
Eighty patients (excluding one patient who died perioperatively) were involved in our follow-up system and they were reviewed at different time intervals. In the immediate postoperative period, patients were reviewed every 1–2 months. Beyond the first 2 months, survivors were reviewed at intervals from 3 to 6 months. All patients underwent at least one follow-up review. Thirty-nine patients censored during follow-up. Follow-up ended in December 2003, with terms ranging from 3 to 108 months. Serum AFP level, B-US, CT, MRI, and angiography were used as monitors of intrahepatic recurrence and distant metastasis postoperatively. If recurrence and metastasis occurred, transcatheter arterial chemoembolization (TACE), local therapies, and biological therapy were adopted for management.
Statistical analysis
Overall or disease-free survival was analyzed by the Kaplan-Meier method, and differences were verified by the log rank test. Cox regression (proportional hazard model) was adopted for multivariate analysis of prognostic predictors. The statistical software package SPSS11.5 (SPSS Inc, Chicago, IL) was employed in all analyses. A statistically significant p value was defined as < 0.05.
Results
Perioperative morbidity and mortality rates after RMH
Ten patients developed life-threatening complications after RMH, including secondary peritoneal bleeding in 5 patients, hepatic insufficiency in 2, biliary fistula in 2, and hemorrhage of the upper digestive tract in 1. Life-threatening morbidity rate was 12.3% (10/81). Six patients (all with secondary peritoneal hemorrhage and 1 with biliary fistula) and 3 patients (1 with hepatic insufficiency, 1 with biliary fistula, and 1 with hemorrhage of the upper digestive tract caused by stress ulcer of the stomach) recovered after reoperation or conservative treatment, respectively. In addition, pleural effusion and ascites without hepatic insufficiency were observed in 4 and 6 patients, respectively. These complications were managed successfully with conservative treatments. The overall morbidity rate was 24.7% (20/81 patients).
There were no operative deaths, but 1 patient died of hepatic failure perioperatively. The perioperative mortality rate was therefore 1.2% (1/81 patients).
Long-term survival of HCC patients after RMH
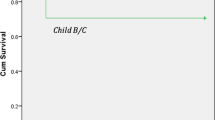
With the exception of the one patient who died, the postoperative overall survival at 1, 3, and 5 years was 77.7%, 47.3%, and 39.4% (median ± SE, 26 ± 9 [95% CI, 8–44] months), respectively. Correspondingly, the 1-, 3-, and 5-year disease-free survival rates were 62.9%, 33.2%, and 28.1% (17 ± 3 [95% CI, 11–23] months), respectively (Fig. 1).
Prognostic factors of HCC patients after RMH
Five clinicopathological variables were shown by univariate analysis as potential prognostic indicators of both overall and disease-free survival of cirrhotic HCC patients after RMH, including the presence of PVTT and satellite nodules, TNM staging, Edmondson-Steiner grading, and blood transfusion (p < 0.05; Table 1). After evaluating the aforementioned significant factors in the Cox regression system, Edmondson-Steiner grading was the sole independent indicator for both overall and disease-free survival. In addition, blood transfusion independently predicted overall survival, and presence of PVTT independently predicted disease-free survival (p < 0.05; Table 2).
Discussion
For HCC, one of the most prevalent and deadly malignancies around the world, hepatectomy has been proven as the first choice for radical treatment. In recent years there have been many clinical investigations concerning improved prognosis of HCC patients after hepatectomy [2–4]. At the same time, with advances in operative techniques and instruments, the risk of hepatic surgery, mainly expressed as mortality and morbidity rates, has markedly decreased. For instance, the mortality rate associated with major hepatectomy (MH) has gradually decreased from a level higher than 20% in a period of about 2 decades [18, 19]. Nevertheless, the procedure held many risk factors such as large removed volume, significant blood loss leading to homologous blood transfusion, and insufficient liver function reserve. Recent reports have shown that the mortality rate of MH was as high as 5% [8, 9, 20], with the lowest value of 2.9% in a series of MH under a limited definition (removing at least 2 segments) [21]. At the same time, associated morbidity was still around 40% according to some recent papers [9, 20]. Therefore, MH might be risky, especially for patients with liver cirrhosis.
In a period of 8 years, we successfully performed RMH in 81 cirrhotic HCC patients, with a low mortality rate of 1.2% and morbidity rate of 24.7%, indicating that the procedure could be safely carried out. We discussed two pivotal techniques that might contribute to this satisfactory perioperative outcome. The first was normothermic continuous interruption of the porta hepatis, and the second was routine use of the cavitron ultrasonic surgical aspirator (CUSA).
The significance of intermittent hepatic inflow occlusion for safe hepatectomy has been generally recognized [22]. It was easily understood that continuous interruption could further simplify procedures, shorten operating time, and reduce blood loss (especially during transection of liver parenchyma), as reported previously [23]. Obviously less blood loss and shorter operating time in our cohort have been achieved, in contrast to patients with similar general background reported previously [9]. Although some authors have argued that intermittent interruption of flow through the porta hepatis leads to less liver injury during hepatic resection than with continuous flow [23], different ischemic time might, at least in part, account for the result. In previous studies [20, 23], the mean ischemic time was approximately 40 min, far longer than in the present study (20.6 min). Our experience, similar to results of a recent prospective, randomized clinical trial from Italy [24], established that MH under normothermic continuous interruption of flow through the porta hepatis could be well tolerated by HCC patients, even those with liver cirrhosis, when the interruption time was well controlled. Thus, intermittent interruption of the porta hepatis might not be necessary.
The advantages of routine use of the CUSA system for hepatic parenchyma dissection have also been recognized. Among them are the significantly reduced operative blood loss and the associated lower need for homologous blood transfusion, both of which contribute to the safety of hepatectomy [25]. Furthermore, CUSA-based hepatic resection might result in excellent long-term survival [26]. Our data demonstrate the value of CUSA for MH, especially in patients with liver cirrhosis. However, portal vein embolization (PVE) a newly introduced technique for safe hepatectomy, was not used in our series. Although PVE was known to increase the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver [27], other authors have found that it might be associated with remote metastasis of HCC [28]. To avoid a poor long-term prognosis of patients, the technique was abandoned. However, the quite satisfactory safety in our series suggests that MH without PVE can be successfully carried out for cirrhotic patients with HCC.
For cirrhotic HCC patients with large tumor size (mean value of about 10 cm) in the cohort, RMH was associated with satisfactory long-term survival rates, that were comparable to those reported for relatively smaller tumors [9]. Thus MH was not only valuable for small HCCs, in accord with the findings by previous investigators [6], but also for large ones, although fundamental liver diseases and non-favorable factors were present.
Limited published data document that tumor-related factors, such as vascular invasion and tumor size, are more likely to be poor prognostic factors after MH [10, 11]. The evidence from our cohort was similar. Univariate and multivariate analyses showed that major variables defined as prognostic predictors, including presence of PVTT and satellite nodule, Edmondson-Steiner grading, and TNM staging, were cancer-associated clinical, biological, and pathological parameters. These results remind us of the impact of characteristics of tumor alone, especially pathological and biological ones, on postsurgical long-term survival of patients with HCC after MH. Such impacts should be further evaluated. Among these variables, the crucial impact of histological grade, in accordance with Edmondson-Steiner criteria [7], on prognosis of cirrhotic patients with HCC after RMH was first revealed in the present study, although it had been established by previous authors in small HCCs [29]. These grading criteria were mainly based on the features of HCC cells, such as size, morphology, and mitotic figures. The higher the grade, the poorer the differentiation presented by the tumor. The finding that differentiation of hepatocellular carcinoma cells was positively correlated with the invasive proclivity and tumor recurrence might account for the dismal prognosis of patients with poorly differentiated HCC [30]. Additionally, the predicting value of PVTT on disease-free survival should be comprehended easily, because its close relationship with postoperative recurrence has been established [31]. More importantly, our results first suggested that blood transfusion, a common event during surgery, independently influenced overall survival after RMH for HCC patients with underlying cirrhosis. Many investigators have suggested that perioperative blood transfusion promoted recurrence of HCC [32, 33], due to, at least in part, its immunosuppressive effects [34]. Because MH is one of the major procedures in hepatic surgery and is more likely to require blood transfusion than minor ones, more attention should be focused on careful preoperative evaluation and intraoperative manipulation in order to reduce blood loss and subsequent blood transfusion during MH. Contrarily, the fact that Child-Pugh grading was not shown to be of prognostic significance suggests that extensive hepatic resections could be carried out more aggressively, if these procedures were estimated to be well tolerated. In our series, in contrast to a previous report [35], we did not show the independent role of TNM staging in prognosis. This may have been because there was a stage distribution bias in the cohort we studied (no stage 1 tumors). Therefore, the data could not reduce the importance of TNM staging in the total spectrum of resectable HCC.
In conclusion, RMH can be regarded as a safe procedure that may be of benefit to cirrhotic patients with HCC. In our study, some biological, pathological, and surgery-related factors were closely associated with their long-term prognosis.
References
Parkin DM, Bray F, Ferlay J, et al. (2001) Estimating the world cancer burden: Globocan 2000. Int J Cancer 94:153–156
Poon RT, Fan ST, Lo CM, et al. (2001) Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 234:63–70
Shimozawa N, Hanazaki K (2004) Longterm prognosis after hepatic resection for small hepatocellular carcinoma. J Am Coll Surg 198:356–365
Lau WY, Ho SK, Yu SC, et al. (2004) Salvage surgery following downstaging of unresectable hepatocellular carcinoma. Ann Surg 240:299–305
Kianmanesh R, Regimbeau JM, et al. (2003) Selective approach to major hepatic resection for hepatocellular carcinoma in chronic liver disease. Surg Oncol Clin North Am 12:51–63
Lang BH, Poon RT, Fan ST, et al. (2003) Perioperative and long-term outcome of major hepatic resection for small solitary hepatocellular carcinoma in patients with cirrhosis. Arch Surg 138:1207–1213
Shimada M, Gion T, Hamatsu T, et al. (1999) Evaluation of major hepatic resection for small hepatocellular carcinoma. Hepatogastroenterology 46:401–406
Couinaud C (1999) Liver anatomy: portal (and suprahepatic) or biliary segmentation. Dig Surg 16:459–467
Capussotti L, Muratore A, Massucco P, et al. (2004) Major liver resections for hepatocellular carcinoma on cirrhosis: early and long-term outcomes. Liver Transpl 10(suppl 1):S64–S68
Nagasue N, Yamanoi A, el-Assal ON, et al. (1999) Major compared with limited hepatic resection for hepatocellular carcinoma without underlying cirrhosis: a retrospective analysis. Eur J Surg 165:638–646
Chan SC, Liu CL, Lo CM, et al. (2003) Value of live donor liver transplantation experience in major hepatectomy for hepatocellular carcinoma. Arch Surg 138:265–271
Zhou L, Rui JA, Wang SB, et al. (2003) Multi-modal serial therapy for primary liver cancer in senile patients: a report of 153 cases. Zhonghua Zhong Liu Za Zhi 25:404–406
Qu Q, Rui JA, Wang SB, et al. (2006) Comparison of different clinical staging systems for hepatocellular carcinoma. Zhonghua Zhong Liu Za Zhi 28:155–158
Zhou L, Rui JA, Wang SB, et al. (2006) Clinicopathological features, post-surgical survival and prognostic indicators of elderly patients with hepatocellular carcinoma. Eur J Surg Oncol 32:767–772
Terminology Committee of the International Hepato-Pancreato-Biliary Association (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB 2:333–339
Hermanek P, Sobin LH (1992) TNM Classification of Malignant Tumors. Berlin, Springer-Verlag, 104–112
Edmondson HA, Steiner PE (1954) Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7:462–503
Thompson HH, Tompkins RK, Longmire WP Jr. (1983) Major hepatic resection. A 25-year experience. Ann Surg 197:375–388
Tjandra JJ, Fan ST, Wong J (1991) Peri-operative mortality in hepatic resection. Aust N Z J Surg 61:201–206
Pol B, Campan P, Hardwigsen J, et al. (1999) Morbidity of major hepatic resections: a 100-case prospective study. Eur J Surg 165:446–453
Chang YC (2004) Low mortality major hepatectomy. Hepatogastroenterology 51:1766–1770
Man K, Lo CM, Liu CL, et al. (2003) Effects of the intermittent Pringle manoeuvre on hepatic gene expression and ultrastructure in a randomized clinical study. Br J Surg 90:183–189
Belghiti J, Noun R, Malafosse R, et al. (1999) Continuous versus intermittent portal triad clamping for liver resection: a controlled study. Ann Surg 229:369–375
Capussotti L, Nuzzo G, Polastri R, et al. (2003) Continuous versus intermittent portal triad clamping during hepatectomy in cirrhosis. Results of a prospective, randomized clinical trial. Hepatogastroenterology 50:1073–1077
Fan ST, Lai EC, Lo CM, et al. (1996) Hepatectomy with an ultrasonic dissector for hepatocellular carcinoma. Br J Surg 83:117–120
Hodgson WJ, Morgan J, Byrne D, et al. (1992) Hepatic resections for primary and metastatic tumors using the ultrasonic surgical dissector. Am J Surg 163:246–250
Azoulay D, Castaing D, Krissat J, et al. (2000) Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg 232:665–672
Wakabayashi H, Ishimura K, Okano K, et al. (2001) Is preoperative portal vein embolization effective in improving prognosis after major hepatic resection in patients with advanced-stage hepatocellular carcinoma? Cancer 92:2384–2390
Fukuda S, Itamoto T, Nakahara H, et al. (2005) Clinicopathologic features and prognostic factors of resected solitary small-sized hepatocellular carcinoma. Hepatogastroenterology 52:1163–1167
Ker CG, Chen HY, Chen KS, et al. (2003) Clinical significance of cell differentiation in hepatocellular carcinoma. Hepatogastroenterology 50:475–479
Park JH, Koh KC, Choi MS, et al. (2006) Analysis of risk factors associated with early multinodular recurrences after hepatic resection for hepatocellular carcinoma. Am J Surg 192:29–33
Makino Y, Yamanoi A, Kimoto T, et al. (2000) The influence of perioperative blood transfusion on intrahepatic recurrence after curative resection of hepatocellular carcinoma. Am J Gastroenterol 95:1294–1300
Hanazaki K, Kajikawa S, Shimozawa N, et al. (2005) Perioperative blood transfusion and survival following curative hepatic resection for hepatocellular carcinoma. Hepatogastroenterology 52:524–529
Kwon AH, Matsui Y, Kamiyama Y (2001) Perioperative blood transfusion in hepatocellular carcinomas: influence of immunologic profile and recurrence free survival. Cancer 91:771–778
Huang YH, Chen CH, Chang TT, et al. (2005) Evaluation of predictive value of CLIP, Okuda, TNM and JIS staging systems for hepatocellular carcinoma patients undergoing surgery. J Gastroenterol Hepatol 20:765–771
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, L., Rui, JA., Wang, SB. et al. Outcomes and prognostic factors of cirrhotic patients with hepatocellular carcinoma after radical major hepatectomy. World J Surg 31, 1782–1787 (2007). https://doi.org/10.1007/s00268-007-9029-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9029-z