Abstract
Background
Although the degree of hepatic resection has been found to be a key aspect of tumor stimulation, the differences in clinical outcome between a massive liver resection and a less extensive resection for multiple colorectal metastases have not been well studied. The purpose of this study was to clarify the impact of the extent of liver resection on survival outcome.
Methods
Clinicopathologic data were available for 85 patients who were surgically treated for four or more liver metastases. Forty-nine patients who underwent a major hepatic resection were compared with patients who underwent minor hepatic resections (n = 36).
Results
As the patients undergoing major resection were more likely to have multiple (p = 0.014) and large tumors (p = 0.021) compared to the minor-resection patients, their overall survival was worse (p = 0.046) and the disease-free rate tended to be poorer. By multivariate analysis of the cohorts, the only independent factor affecting survival was the number of liver tumors (≤5 or ≥6; relative risk [RR] = 0.427; p = 0.014). When patients with six or more metastases were selected and analyzed, the overall survival of patients who had a major resection was significantly poorer than those who had minor resections (p = 0.028), although the clinical characteristics were comparable between the two groups.
Conclusion
Although the extent of hepatectomy was not an independent prognosticator, minor resections for multiple colorectal metastases may offer a long-term survival advantage compared to a major resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatic resection is the only form of treatment that currently offers a chance of long-term survival in patients with colorectal liver metastases, with an approximate 5-year survival rate of 40–49% [1–4]. Classically, most reported surgical experience has involved patients with a small number of metastatic lesions in a distribution confined to the hemiliver, and so only 5–10% of patients with metastatic colorectal cancer are candidates for liver resection, with resection frequently precluded by multisegment involvement [5, 6]. Extensive hepatectomy often is necessary to curatively resect multiple metastases in the liver. In up to 45% of both primary and secondary liver tumors, extended liver resection is necessary to achieve clear resection margins [7]. General agreement has been reached that resection with a clear surgical margin is adequate for the resection of colorectal liver metastases. However, extensive hepatectomy involves a considerable reduction of hepatic mass that can lead to clinical manifestations of decompensation, including hepatic insufficiency. In recent reports, preoperative portal vein embolization (PVE) [8, 9], and two-stage resections [10, 11] have increased the number of patients eligible for potentially curative treatment resulting in favorable short-term and long-term outcomes. The rationale for PVE and/or two-stage hepatectomy is to minimize the risk of liver failure by completing the resection after regeneration has occurred. With improvements in these surgical techniques and perioperative care, major liver resections now are performed increasingly for metastatic liver cancer with a generally low rate of major technical complications and fatal liver failure.
On the other hand, the degree of hepatic resection has been found to be a key factor in tumor stimulation. A number of studies have found that the larger the percentage of liver resection, the higher the incidence and volume of recurrence [12, 13]. Many of the factors upregulated during liver regeneration after a hepatectomy have been implicated in tumor growth and recurrence [14–16] and the extent of the upregulation of these factors correlated with the degree of liver resection. Numerous studies have suggested that regenerative growth factors, many of which are elevated immediately after hepatectomy, play a role in tumor recurrence by stimulating tumor cells to proliferate following resection [14]. PVE also stimulates the growth of hepatic tumors [17–19].
From an oncologic perspective in treating multiple metastases, an extended hepatectomy is an effective way to remove tumors with a sufficient tumor-free margin, while multiple minor resections might reduce tumor proliferation that may be stimulated by a massive liver resection. Given the implications of such recent advances that have extended the indications for hepatectomy in the treatment for colorectal cancer metastases as well as the positive and negative effects of an extended liver resection, there needs to be a reassessment of which hepatectomy procedure, i.e., an extended resection with or without some minor resections vs. multiple minor resections, is the most suitable for multiple colorectal metastases. We therefore retrospectively analyzed patients with four or more liver metastases from colorectal cancer treated at our institution to estimate the differences in the survival benefit from different hepatectomy procedures categorized according to the extent of liver resection.
Patients and methods
Patients
From 1987 to 2006, our Department of Gastroenterological Surgery at the Yokohama City University Graduate School of Medicine treated 320 patients in whom colorectal liver metastases were diagnosed by liver resection with curative intent. Of these, one patient (0.3%) died within 60 days of surgery from multiple organ failure caused by postoperative bleeding and sepsis. Macroscopic residual disease was found in five patients during surgical exploration at the site of liver metastases, and concomitant extrahepatic disease precluded a macroscopic curative resection in 15 other patients who had a macroscopic curative liver resection. One patient was lost to follow-up with no information available concerning survival relative to each time point and therefore was excluded from the study. Of the remaining 298 patients, 213 (71.5%) had three or fewer metastases and were also excluded. Accordingly, data from 85 patients (28.5%) with four or more liver metastases who were surgically treated were subjected to the analysis. The median follow-up duration for these 85 patients was 26 months (range = 3–158). Among these, en masse removal at least a hemiliver (hemihepatectomy, extended hemihepatectomy, or trisectionectomy), with or without some partial resections of the contralateral hemiliver, was performed in 49 patients, and these patients were defined as the major-hepatectomy group. The other 36 patients undergoing several minor resections (one section or less) were defined as the minor-hepatectomy group. The study was approved by our institutional review board and written informed consent was obtained from all patients.
Preoperative staging included a physical examination, measurement of serum carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19-9, colonoscopy, barium enema, abdominal ultrasonography, abdominal computed tomography (CT), and chest imaging by routine chest radiography or CT. Imaging by positron emission tomography (PET) was introduced for preoperative staging after 2002.
Hepatectomy procedures
The hepatectomy was not necessarily performed according to anatomic principles of resection; the guiding principle was assurance of tumor-free margins. The decision regarding which hepatectomy procedure (en masse major hepatectomy or several minor hepatectomies) to perform was made on a case-by-case basis according to tumor number, distribution, and location. To determine whether a hepatectomy procedure was acceptably safe for the patient, we used a prediction score (PS) system introduced by Yamanaka et al. [20]. The PS was calculated using the formula PS = −84.6 + 0.933a + 1.11b + 0.999c, where a is the anticipated resection fraction (%) calculated from CT volumetry, b is the indocyanine green retention rate at 15 min (%), and c is the age (years) of the patient. A PS < 50 indicated that a given hepatectomy would be acceptable. Patients with PS ≥ 50 underwent either a two-stage hepatectomy or prehepatectomy PVE.
Intraoperative ultrasonography was used to identify any occult tumors not detected preoperatively and to confirm the relationships between the tumors and vasculobiliary structures. Parenchymal dissection was performed using ultrasonic dissectors. When necessary, the liver pedicle was clamped intermittently in cycles including 15 min of clamping and 5 min of reperfusion. The Brisbane 2000 terminology of the International Hepato-Pancreato-Biliary Association was used to categorize the operative procedures [21]. Tumor-free margins of 0 mm in this study was defined as a part of a tumor exposed microscopically on the cutting plane with neither macroscopic exposure nor evidence of residual tumor tissue. The use of microwave ablation in combination with resection was reserved for patients for whom no procedure that permitted complete resection of neoplasms that preserved sufficient vascularized hepatic parenchyma to support postresection hepatic function could be designed, or in whom some tumors were ill located. Microwave ablation was used in combination with resection. All patients underwent resection and ablation during open laparotomy by a hepatobiliary surgeon. Intraoperative ultrasound (IOUS) was used to guide placement of the ablation needle into the lesions to be treated with microwave therapy. All patients who underwent microwave ablation were treated using the Microtaze AZM-520 system (Azwell, Osaka, Japan). Microwave energy was delivered at 70 W for 45 s, followed by a 15-s pause. The needle then was repositioned. Four or five cycles of ablation were performed with the aim of obtaining at least a 1-cm zone of coagulation surrounding the liver tumors. To accomplish complete destruction of the neoplasms and to avoid bile duct injury, we used microwave ablation only for relatively small neoplasms (2 cm or less in diameter) that were not located near the main Glisson sheath. Recognition of complete ablation status after treatment was made from the findings of IOUS after ablation and from the findings of complete diminishment of enhancement in the postoperative arterial phase of CT.
All extrahepatic metastases were resected whenever possible, as decided on a case-by-case [22]. For cases of resectable metastases in both the liver and the lung, liver resection and primary tumor resection were performed prior to pulmonary resection, aiming to eliminate the liver as a source of potentially disseminating neoplastic cells. When liver metastases were associated with extrahepatic intra-abdominal metastases, both were resected at the same time.
The principles underlying the selection criteria for the resection of recurrent hepatic metastases were the same as those for the initial hepatectomy. Technical considerations predominated in surgical decisions regarding the feasibility of repeat hepatic resection. Because the quality and quantity of the remaining hepatic parenchyma were extremely important factors, patients were excluded from repeat hepatic resection when the PS, based on volumetry, indocyanine green retention rate, and patient age, was greater than 50 [20].
Whenever safe and macroscopic complete resection of all sites of extrahepatic disease was deemed possible after the identification of any extrahepatic recurrences, a resection was performed irrespective of the recurrence sites.
Neoadjuvant chemotherapy
Some patients with multiple liver metastases whose metastases initially would have posed difficulties in their safe removal first received neoadjuvant hepatic arterial chemotherapy with a combination of 5-fluorouracil (5-FU), l-folinic acid (FA), and cisplatin (CDDP). Treatment consisted of a 5-day course of infusions into the hepatic artery through an implanted arterial access port (Vital-Port, Cook Vascular, Leechburg, PA). On each day, 5-FU (500–600 mg/m2/day), FA (100 mg/m2/day), and CDDP (10 mg/m2/day) were delivered. This 5-day course was repeated four or more times at 9-day intervals.
Adjuvant therapy
All surgically treated patients generally received additional adjuvant chemotherapy via hepatic artery constant-rate infusion of 5-FU (1500 mg over 24 h) and FA (50 mg over 24 h) once a week for 8 weeks after surgery or they received an intravenous infusion generally of 5-FU and FA with or without the addition of CDDP or irinotecan.
Patient follow-up
Patients underwent follow-up evaluation monthly at our outpatient clinic. Data were obtained and recorded from each patient’s clinical record. Long-term outcome was ascertained through clinical follow-up, tumor registry follow-up, and, when necessary, contact with the patient, family, or referring physician. Serum CEA was measured every month, a CT was performed every 3 months, and a chest roentgenogram was obtained every 6 months for 5 years after the most recent operation.
Statistical analysis
Statistical comparisons of the baseline data were performed using the Mann-Whitney U test, the χ2 test, or Fisher’s exact test. Survival rates were calculated using the Kaplan-Meier method. Cutoff values of continuous variables were determined by the median values for univariate analysis. Multivariate regression analysis was carried out by a proportional hazards method using a Cox model, beginning with the factors identified in the univariate analysis with a p < 0.05. Differences between the survival curves were analyzed by the log-rank test. A difference was considered significant when the two-sided p value was less than 0.05.
Results
The rates for the 1-, 3-, 5-, and 10-year overall survival of all 85 patients after hepatectomy were 89.0%, 51.8%, 40.9%, and 13.2%, respectively; the rates for disease-free survival at these time points were 37.0%, 16.0%, 12.0%, and 12.0%, respectively.
Comparison of clinical characteristics and survival outcome between the major-hepatectomy group and the minor-hepatectomy group
The hepatectomy procedure in each group is shown in Table 1. Local ablations in addition to the hepatectomy were conducted in 12 patients (24.5%) in the major-hepatectomy group and in 9 patients (25%) in the minor-hepatectomy group (p > 0.99). When the demographic and clinical characteristics were compared between the patients undergoing a major resection with those undergoing a minor resection, the patients undergoing a major resection were more likely to have multiple (p = 0.014), and large liver tumors (p = 0.021, Table 2). As for the treatment-related variables, a higher proportion of patients in the major-hepatectomy group underwent prehepatectomy PVE (49%, 24/49) than in the minor-hepatectomy group (8.3%, 3/39; p < 0.001), and a staged hepatectomy procedure was conducted more frequently in the major-hepatectomy group (34.7%, 17/49) than in the minor-hepatectomy group (5.6%, 2/36; p = 0.01). The three patients who underwent a PVE and a two-staged procedure in the minor-hepatectomy group were initially to undergo an extended resection following PVE or a second liver resection, but extended resections were precluded by insufficient liver volume regeneration following PVE or the first liver resection. The median resected liver weight in the major-hepatectomy group was larger than that in the minor-hepatectomy group (610 vs. 326 g, p < 0.001). As for surgical variables, the incidence of blood transfusion was 59.2% (29/49) in the major-hepatectomy group and 41.7% (15/36) in the minor-hepatectomy group (p = 0.13). The operative morbidity rate (20.4% in the major group vs. 13.9% in the minor group, p = 0.57) and the median length of the postoperative hospital stay (17 vs. 15 days, respectively; p = 0.36) also were similar.
During follow-up, recurrence was found in 42 patients (86%) in the major-resection group. Sites of initial recurrence were the liver in 15, the lung in 10, multiple organs in 8, and other sites in 9. In the minor-resection group, recurrence was seen in 26 patients (72%), the liver being the initial recurrence site in 11, the lung in 6, multiple organs in 2, and other sites in 7 (p = 0.61 vs. major-resection group). Hepatic recurrences developed at some time in 28 of the patients who had a major resection and in 20 of the patients who had a minor resection. A second liver resection for recurrence was performed in 7 (25%) of the 28 patients with a liver recurrence in the former group and in 7 (35%) of the 20 patients in the latter group (p = 0.53). A surgical resection was undertaken in 10 (27%) of the 37 patients in the major-hepatectomy group who developed an extrahepatic recurrence at some time, while 5 (24%) of the 21 patients in the minor-hepatectomy group had a resection for an extrahepatic recurrence (p > 0.99, Table 2).
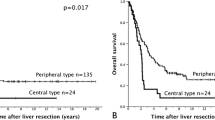
When survival was compared between the patients who underwent a major resection and a minor resection, the 1-, 3-, and 5-year overall survival rates of the patients in the major-hepatectomy group were 83.2%, 41.4%, and 33.1%, respectively, which was poorer than those of the patients in the minor-hepatectomy group (97.2%, 67.9%, and 52.0%, respectively; Fig. 1A, p = 0.046). The disease-free survival rates in the major-hepatectomy group (28.7%, 11.5%, and 8.6%, respectively) also tended to be poorer than those in the minor-hepatectomy group (48.5%, 23.6%, and 17.7%, respectively; Fig. 1B, p = 0.11).
Overall and disease-free survival in postoperative years for 85 patients with four or more liver metastases from colorectal cancer. (A) When patients were divided into those who underwent a major resection (broken lines, n = 49) versus a minor resection (solid lines, n = 36), overall survival was worse in the major-hepatectomy group (p = 0.046). (B) The disease-free survival rate tended to be poorer in the major-hepatectomy group than in the minor-hepatectomy group (p = 0.110)
Prognostic factors for patients with four or more metastases
The influence of various clinicopathologic variables on survival after hepatectomy is shown in Table 3. According to univariate analysis using the data of all 85 patients with multiple metastases, the number of liver tumors (p = 0.003), the maximum size of the metastatic lesions (p = 0.03), the prehepatectomy serum CEA (p = 0.016), the extent of hepatectomy (major resection vs. minor resection, p = 0.046), and the administration of adjuvant chemotherapy after hepatectomy (p = 0.019) were identified as significant prognostic determinants. Specifically, survival was significantly worse in patients with six or more nodules, a maximum liver neoplasm diameter of more than 38 mm, a serum CEA concentration before hepatectomy exceeding 10 ng/ml, performing an en masse hepatectomy (at least a hemiliver) with or without some contralateral partial resections, and no adjuvant chemotherapy. By multivariate analysis, the only independent factor affecting survival was the number of liver tumors (5 or fewer vs. 6 or more; relative risk [RR] = 0.427; p = 0.014; Table 4).
Comparison of clinical characteristics and survival outcome of patients with at least six metastases between the major-hepatectomy group and the minor-hepatectomy group
In the second phase of the analysis, in order to overcome the effects of differences in the number of liver tumors that might influence patient survival between the major- and the minor-hepatectomy groups, patients with six or more metastases were selected and analyzed. When the clinical characteristics were compared between the patients undergoing a major resection (n = 27) with those undergoing a minor resection (n = 13), no significant difference in any of the variables, including the number of liver tumors, was observed between the two groups (Table 5). Due to differences in the extent of liver removal, a higher proportion of patients in the major-hepatectomy group underwent prehepatectomy PVE (55.6%, 15/27) than in the minor-hepatectomy group (15.4%, 2/13; p = 0.020). Furthermore, the proportion of staged hepatectomy procedures tended to be more frequent in the major-hepatectomy group (37%, 10/27) than in the minor-hepatectomy group (7.7%, 1/13; p = 0.068). The proportion of patients with a liver recurrence who underwent a repeat resection and those with extrahepatic metastases who underwent a resection were comparable.
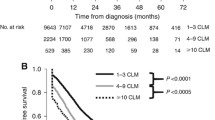
During follow-up, recurrence became evident in 24 patients (89%) in the major-resection group and in 9 (69%) in the minor-resection group. As for the sites of initial recurrence, remaining liver and pulmonary recurrence tended to be higher in the major-resection group (liver and lung, 58%; multiple organs, 21%; other sites, 21%), while recurrence in other sites tended to be highest in the minor-resection group (liver and lung, 33%; multiple organs, 11%; other sites, 56%). The 1-, 3-, and 5-year overall survival rates after hepatectomy were 77.6%, 24.1%, and 12.1%, respectively, in the major-hepatectomy group vs. 92.3, 62.2, and 31.1%, respectively, in the minor-hepatectomy group (p = 0.028, Fig. 2A). The 1- and 3-year disease-free survival rates in the major-hepatectomy group were 16.9% and 8.5%, respectively, which also tended to be poorer than those in the minor-hepatectomy group (53.8 and 28.8%, respectively; Fig. 2B, p = 0.058).
Overall and disease-free survival rates in postoperative years for the 40 patients with six or more liver metastases from colorectal cancer. (A) When the patients were divided into those who underwent a major resection (broken lines, n = 27) versus a minor resection (solid lines, n = 13), overall survival was worse in the major-hepatectomy group (p = 0.028). (B) The disease-free rate tended to be poorer, and almost reached statistical significance, in the major-hepatectomy group compared to the minor-hepatectomy group (p = 0.058)
On the other hand, in patients with five or fewer metastases, the 1-, 3-, and 5-year overall survival rates were 90.5%, 60.5%, and 55.0%, respectively, in the major-hepatectomy group (n = 22) vs. 100, 70.7, and 57.2% in the minor-hepatectomy group (n = 23, p = 0.879), and the disease-free survival rates at each time point were 43.3%, 16.2%, and 10.8%, respectively, in the major-hepatectomy group vs. 45.2, 21.5, and 14.3%, respectively, in the minor-hepatectomy group (p = 0.817). However, no significant difference in the clinical characteristics of the two groups was observed except for the median age of the patients (the major group vs. the minor group, 56 vs. 68 years; p = 0.007), the percentage undergoing prehepatectomy PVE (40.9% vs. 4.3%, p = 0.004), and the percentage having a staged hepatectomy procedure (31.8 vs. 4.3%, p = 0.022).
Impact of degree of hepatectomy and prehepatectomy chemotherapy on patient survival
When all 85 patients were divided into four groups based on the extent of the hepatectomy (major vs. minor resection) and the administration of prehepatectomy chemotherapy (performed vs. not performed), the number of liver tumors was lower in the patients in the minor resection without chemotherapy group than in the patients in the major resection and chemotherapy group (p < 0.001), the major resection alone group (p = 0.002), and the minor resection with chemotherapy group (p = 0.005). Although there was no significant difference in the number of tumors between the groups (except for the minor resection alone group), the number of tumors in the major resection alone group tended to be lower than those of the major resection with chemotherapy group and minor resection with chemotherapy group. There was no difference between the groups in median survival time; however, the survival of the patients who underwent a minor resection with chemotherapy tended to be longer than those of the major resection with or without chemotherapy groups (Table 6).
Discussion
In general, tumor recurrence in the liver has been linked to several factors, including the accuracy of the staging techniques and the presence or absence of positive resection margins. Another factor may be liver regeneration following a hepatic resection, which may stimulate occult tumor growth at both intrahepatic and extrahepatic sites. Growth factors such as hepatocyte growth factor, epidermal growth factor, and insulin-like growth factor are generally upregulated early in liver regeneration, producing a mitogenic response and resulting in rapid hepatocyte cell proliferation. Many of these factors, however, have also been implicated in stimulating tumor growth [23]. It has also been suggested that these growth factors have a greater stimulatory effect on tumor cells than on hepatocytes [24]. Some other studies have shown that liver resection does not result in tumor stimulation; however, in all these studies, the resections performed were less than 50% hepatectomies and would be considered as minor resections [25–27]. A larger resection causes the liver to express higher levels of growth factors and cytokines to restore the liver to its functional size in approximately the same time as for a smaller hepatectomy [28, 29].
PVE also may stimulate the growth of hepatic tumors [17–19, 30]. Elias et al. [30] performed studies which looked at liver regeneration following right portal embolization in patients who had undergone a hepatic resection to induce hypertrophy of the left hemiliver. It was found that the growth rate of liver metastases exceeded that of the normal liver parenchyma, suggesting that the process of regeneration has a significant proliferative effect on tumors. Kokudo et al. [19] assessed the proliferative activity of intrahepatic metastases in the embolized liver after PVE in 18 patients with colorectal metastases and found a significantly increased tumor Ki-67 labeling index in the metastases group with PVE compared to those with hepatic metastases but not treated with PVE. Tumor growth after PVE also has been postulated to be controlled by changes in cytokines or growth factors induced by PVE and changes in blood supply after PVE.
In this study, a major resection was defined as en masse removal of at least a hemiliver (hemihepatectomy, extended hemihepatectomy, or trisectionectomy) with or without some contralateral partial resections. Several minor resections (sectionectomy or less) conducted for multiple metastases were defined as a minor resection. Resected liver weights may include multiple tumors and may not correctly reveal the differences in the amount of functional liver volume removed. Accordingly, we used the definitions of major and minor resections as mentioned above. The decision about which procedure to use for the hepatectomy was made on a case-by-case basis but mainly depended on the intrahepatic tumor locations. A major resection was more likely to be performed when one or some of the liver metastases were located in the deep liver portion or near the main Glisson sheath and/or the hepatic vein. On the other hand, a minor resection was performed more often when the tumors were located in the relative vicinity of the liver surface.
When a comparison was made between the major- and the minor-hepatectomy groups, the overall survival was poorer and the disease-free survival tended to be poorer in the major-hepatectomy group compared to the minor-hepatectomy group; however, the number of liver tumors and the maximum tumor size were greater in the major-hepatectomy group than in the minor hepatectomy group. A higher proportion of patients in the major-hepatectomy group underwent prehepatectomy PVE and a staged hepatectomy procedure compared to the minor-hepatectomy group to minimize the risk of liver failure. The other tumor-related variables and treatment-related variables such as the percentage of those receiving perioperative chemotherapy or repeat resections for recurrences were comparable between the two groups. With respect to factors that affect survival after hepatectomy, by multivariate analysis tumor number was the only independent prognostic factor after hepatectomy in this cohort. Because there is a notable impact of the number of liver tumors on survival after hepatectomy, a comparison was made again between the major- and the minor-hepatectomy groups but restricted to patients with at least six metastatic tumors. Although there was no significant difference between the groups in terms of tumor-related and treatment-related factors except for the proportion receiving PVE or a staged procedure, the overall survival was superior and the disease-free survival tended to be superior in the minor-hepatectomy group.
General agreement has been reached that patients with four or more metastatic nodules receive little benefit from liver resection [1, 31], because most patients with multiple liver tumors whose macroscopic tumors are completely resected still harbor microscopic disease and therefore have a much higher probability of recurrence and poorer survival [32]. More recent reports have demonstrated that with recent advances in chemotherapy, long-term survival is possible in patients who have four or more metastases, especially when the treatments include administration of a monoclonal antibody. However, the disease of most patients will ultimately recur after resection [33, 34]. A trend toward increased frequency of micrometastases with increasing numbers of macroscopic tumors can be easily understood. In this setting, the elimination of all micrometastases is impossible, even with a major hepatectomy. The better survival outcome of the minor-resection group compared to the major-resection group in the subset having six or more metastases but no survival difference between the groups with five or fewer metastases in this study may suggest that recurrences after a hepatectomy may result from the more accelerated growth of the micrometastases left behind from a large hepatectomy compared to the growth of micrometastases left behind after a minor hepatectomy. Although the prognostic significance of micrometastases after a hepatectomy is still controversial, a less extensive hepatectomy should always be considered to avoid the possibility of an accelerated growth of tumor tissue left in place after a hepatectomy. With respect to the site of initial recurrence, no difference was observed between groups. However, when patients with six or more metastases were selected and analyzed, the remaining liver recurrence and pulmonary recurrence tended to be higher in the major-resection group, and recurrence in the other sites tended to be highest in the minor-resection group.
In the major-hepatectomy group, a two-stage procedure together with portal vein embolization was conducted in 13 patients, a two-stage procedure alone in 4 patients, and portal vein embolization alone in 11 patients. Of the other 21 patients who did not have portal vein embolization or a staged procedure, 11 had six or more metastases and 10 had five or fewer. When comparison of survival was made between the 11 patients with six or more metastases who had no portal vein embolization or a staged procedure in the major-hepatectomy group and the 10 patients with six or more metastases who had no portal vein embolization or staged procedure in the minor-hepatectomy group, although no significant difference between groups was observed because of the small number of patients, 1- and 3-year overall and disease-free survival in the minor-hepatectomy group was 92.3% vs. 62.2% and 53.8% vs. 28.8%, respectively, which tended to be greater than those of 90.9% vs. 35.4% and 22.7% vs. 22.7%, respectively, in the major-hepatectomy group (data not shown). According to these results, although portal vein embolization or the staged procedure has some effect on patient survival, minor liver resections may offer the possibility of long-term survival for patients with multiple liver metastases.
Combined resection/ablation was considered a poor prognostic factor after hepatic resection [35]. However, as we reported previously [36], similar overall survival was observed even when patients were divided on the basis of whether or not ablation therapy was performed as an adjunct to hepatectomy, the 1-, 3-, and 5-year survival rates in patients with resection/ablation being 85.2%, 51.3%, and 27.3%, respectively, and 90.1%, 51.7%, and 43.0%, respectively, in patients who underwent hepatectomy alone (p = 0.646). Furthermore, when patients with six or more metastases were divided into three groups, namely, patients receiving adequate tumor-free margin resection, those with resection margins of 0 mm, and those with resection/ablation, and when survival outcome was compared between patients with major and minor hepatectomy in each group, although no significant difference was observed because of the small number of patients, the 3-year survival of 40% in patients with minor hepatectomy tended to be greater than that of 20% seen in patients with major hepatectomy among the group receiving adequate margin resection. The same tendency was observed both in patients with resection margins of 0 mm (3-year survival: 50% in minor hepatectomy vs. 28.6% in major hepatectomy) and in patients with resection/ablation (3-year survival: 100% in minor hepatectomy vs. 56% in major hepatectomy, data not shown).
Regarding prehepatectomy chemotherapy, when a comparison was made between the patients who underwent a major resection without prehepatectomy chemotherapy and patients who received chemotherapy followed by a minor resection, the median survival time of the group with a minor resection and chemotherapy tended to be longer than that of the group with a major resection alone, although the number of liver tumors was higher in the former than in the latter group. Current chemotherapy regimens can achieve either stabilization or a response in more than 80% of patients [37, 38], and neoadjuvant chemotherapy given prior to hepatectomy allows us to extend the indications for surgery in the presence of multiple metastases, permitting long-term survival especially in chemotherapy responders [32, 39, 40]. Furthermore, neoadjuvant chemotherapy-associated decreases in micrometastases surrounding liver tumors are related to clinical responses and a favorable outcome [32], and so the complete removal of liver tumors could be achieved by a less extensive resection. Some changes in liver function postoperatively and an increase in the proportion of morphologic changes in nonmalignant livers occur after prehepatectomy chemotherapy; however, this therapeutic approach was not associated with increased morbidity or mortality unless the administration of chemotherapy was prolonged [41–43]. Therefore, in treating multiple liver metastases, chemotherapy before a hepatectomy followed by a minor resection may offer the possibility of long-term survival especially in chemoresponders. In the present study, HAI was used both as neoadjuvant and as adjuvant chemotherapy. Some reports demonstrated a significant decrement in hepatic recurrence when HAI adjuvant chemotherapy was given. While this treatment given alone did not reliably yield an overall survival benefit [44, 45], Kemeny et al. reported that HAI therapy increased overall survival for patients with unresectable colorectal liver metastases [46] and that postoperative treatment with a combination of HAI and intravenous chemotherapy improved outcomes for patients who underwent resection of liver metastases [47]. Oxaliplatin has been approved for use by the Japanese health insurance system only since April 2005, and at present a combination of HAI and an intravenous oxaliplatin-based regimen is given to patients as both neoadjuvant and adjuvant treatment in our institution. Better survival may be obtained by including administration of oxaliplatin and/or a monoclonal antibody. According to a recent report [48], imaging showed that approximately 80% of liver metastases having a complete response after chemotherapy had persistent macro- or microscopic residual disease or recurrence. Therefore, we should try, as far as possible, to eliminate all liver metastases during the operation, especially with minor resections. However, when it is difficult to recognize whether there is a tumor remnant, frequent follow-ups should be performed, and resection should be repeated if a remnant tumor increases in size.
In conclusion, although the degree of hepatic resection was not an independent prognosticator, the prognosis of patients with a major resection with or without PVE or a staged resection was poorer than that of patients with multiple minor resections, perhaps due to the induction of the proliferation of micrometastases by upregulating the expression of cytokines and growth factors after a massive hepatectomy. The number of patients in this study was limited; however, the results of this retrospective study may suggest a survival advantage for patients with multiple liver metastases who were treated with multiple minor liver resections. In addition, neoadjuvant chemotherapy followed by multiple minor liver resections may offer long-term survival. Further studies on a larger number of patients and a prospective randomized controlled study are needed to confirm this preliminary finding.
Abbreviations
- CA:
-
Carbohydrate antigen
- CDDP:
-
Cisplatin
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
- FA:
-
l-Folinic acid
- 5–FU:
-
5-Fluorouracil
- Major:
-
En masse removal of at least half the liver with or without some contralateral partial resections
- Minor:
-
Multiple minor (one section or less) resections
- Moderate:
-
Moderately differentiated adenocarcinoma
- PET:
-
Positron emission tomography
- PS:
-
Prediction score
- PVE:
-
Portal vein embolization
- RR:
-
Relative risk
References
Registry of Hepatic Metastases (1988) Resection of the liver for colorectal carcinoma metastases: a multiinstitutional study of indications for resection. Surgery 103:278–288
Minagawa M, Makuuchi M, Torzilli G et al (2000) Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 231:487–499
Shaw IM, Rees M, Welsh KS et al (2006) Repeat hepatic resection for recurrent colorectal liver metastases is associated with favorable long-term survival. Br J Surg 93:457–464
Arru M, Aldrighetti L, Castoldi R et al (2007) Analysis of prognostic factors influencing long-term survival after hepatic resection for metastatic colorectal cancer. World J Surg 32:93–103
Fortner JG, Silva JS, Golbey RB et al (1984) Multivariate analysis of a personal series of 247 consecutive patients with liver metastases from colorectal cancer. I. Treatment by hepatic resection. Ann Surg 199:306–316
August DA, Ottow RT, Sugarbaker PH (1984) Clinical perspective of human colorectal cancer metastasis. Cancer Metastasis Rev 3:303–324
Broering DC, Hillert C, Krupski G et al (2002) Portal vein embolization vs. portal vein ligation for induction of hypertrophy of the future liver remnant. J Gastrointest Surg 6:905–913
Abdalla EK, Hicks ME, Vauthey JN (2001) Portal vein embolization: rationale, technique and future prospects. Br J Surg 88:165–175
Athoulay D, Castaing D, Smail A et al (2000) Resection of nonresectable liver metastases from colorectal cancer after percutaneous portal vein embolization. Ann Surg 231:480–486
Adam R, Laurent A, Azoulay D et al (2000) Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg 232:777–785
Kianmanesh R, Farges O, Abdalla EK et al (2003) Right portal vein ligation: a new planned two-step all-surgical approach for complete resection of primary gastrointestinal tumors with multiple bilateral liver metastases. J Am Coll Surg 197:164–170
Ikeda Y, Matsumata T, Takenaka K et al (1995) Preliminary report of tumor metastasis during liver regeneration after hepatic resection in rats. Eur J Surg Oncol 21:188–190
Mizutani J, Hiraoka T, Yamashita R et al (1992) Promotion of hepatic metastases by liver resection in the rat. Br J Cancer 65:794–797
Jiang W, Hiscox S, Matsumoto K et al (1999) Hepatocyte growth factor/scatter factor, its molecular, cellular and clinical implications in cancer. Crit Rev Oncol Hematol 29:209–248
Lukomska B, Dluzniewska J, Polanski J et al (2004) Expression of growth factors in colorectal carcinoma liver metastatic patients after partial hepatectomy: implications for a functional role in cell proliferation during liver regeneration. Comp Hepatol 3(Suppl 1):S52
Yoon SS, Kim SH, Gonen M et al (2006) Profile of plasma angiogenic factors before and after hepatectomy for colorectal cancer liver metastases. Ann Surg Oncol 13:353–362
Hemming AW, Reed AI, Howard RJ et al (2003) Preoperative portal vein embolization for extended hepatectomy. Ann Surg 237:686–693
Barbaro B, Di Stasi C, Nuzzo G et al (2003) Preoperative right portal vein embolization in patients with metastatic liver disease. Metastatic liver volumes after RPVE. Acta Radiol 44:98–102
Kokudo N, Tada K, Seki M et al (2001) Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization. Hepatology 34:267–272
Yamanaka N, Okamoto E, Oriyama T et al (1994) A prediction scoring system to select the surgical treatment of liver cancer. Further refinement based on 10 years of use. Ann Surg 219:342–346
The Brisbane (2000) Terminology of Liver Anatomy and Resection (2000) Terminology Committee of the International Hepato-Pancreato-Biliary Association. HPB 2:333–339
Elias D, Ouellet JF, Bellon N et al (2003) Extrahepatic disease does not contraindicate hepatectomy for colorectal liver metastases. Br J Surg 90:567–574
Harun N, Nikfarjam M, Muralidharan V et al (2007) Liver regeneration stimulates tumor metastases. J Surg Res 138:284–290
Jiang WG, Hallett MB, Puntis MC (1993) Hepatocyte growth factor/scatter factor, liver regeneration and cancer metastasis. Br J Surg 80:1368–1373
Castillo MH, Doerr RJ, Paolini N Jr et al (1989) Hepatectomy prolongs survival of mice with induced liver metastases. Arch Surg 124:167–169
Doerr R, Castillo M, Evans P et al (1989) Partial hepatectomy augments the liver’s antitumor response. Arch Surg 124:170–174
Ono M, Tanaka N, Orita K (1986) Complete regression of mouse hepatoma transplanted after partial hepatectomy and the immunological mechanism of such regression. Cancer Res 46:5049–5053
Fausto N (2000) Liver regeneration. J Hepatol 32(1 Suppl):19–31
Mangnall D, Bird NC, Majeed AW (2003) The molecular physiology of liver regeneration following partial hepatectomy. Liver Int 23:124–138
Elias D, De Baere T, Roche A et al (1999) During liver regeneration following right portal embolization the growth rate of liver metastases is more rapid than that of the liver parenchyma. Br J Surg 86:784–788
Nordlinger B, Guiguet M, Vaillant JC et al (1996) Surgical resection of colorectal carcinoma metastases to the liver: a prognostic scoring system to improve case selection, based on 1568 patients. Cancer 77:1254–1262
Tanaka K, Shimada H, Kubota K et al (2005) Effectiveness of prehepatectomy intra-arterial chemotherapy for multiple bilobar colorectal cancer metastases to the liver: a clinicopathologic study of peritumoral vasculobiliary invasion. Surgery 137:156–164
Kornprat P, Jarnagin WR, Gonen M et al (2007) Outcome after hepatectomy for multiple (four or more) colorectal metastases in the era of effective chemotherapy. Ann Surg Oncol 14:1151–1160
Weber SM, Jarnagin WR, DeMatteo RP et al (2000) Survival after resection of multiple hepatic colorectal metastases. Ann Surg Oncol 7:643–650
Abdalla EK, Vauthey JN, Ellis LM et al (2004) Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 239:818–827
Tanaka K, Shimada H, Nagano Y et al (2006) Outcome after hepatic resection versus combined resection and microwave ablation for multiple bilobar colorectal metastases to the liver. Surgery 139:263–273
Giacchetti S, Perpoint B, Zidani R et al (2000) Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol 18:136–147
Douillard JY, Cunningham D, Roth AD et al (2000) Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trial. Lancet 355:1041–1047
Bismuth H, Adam R, Levi F et al (1996) Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg 224:509–520
Adam R, Avisar E, Ariche A et al (2001) Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal [liver] metastases. Ann Surg Oncol 8:347–353
Parikh AA, Gentner B, Wu TT et al (2003) Perioperative complications in patients undergoing major liver resection with or without neoadjuvant chemotherapy. J Gastrointest Surg 7:1082–1088
Tanaka K, Shimada H, Ueda M et al (2006) Perioperative complications after hepatectomy with or without intra-arterial chemotherapy for bilobar colorectal cancer liver metastases. Surgery 139:599–607
Karoui M, Penna C, Amin-Hashem M et al (2006) Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg 243:1–7
Lorenz M, Müller H, Schramm H et al (1998) Randomized trial of surgery versus surgery followed by adjuvant hepatic arterial infusion with 5-fluorouracil and folinic acid for liver metastases of colorectal cancer. Ann Surg 228:756–764
Onaitis M, Morse M, Hurwitz H et al (2003) Adjuvant hepatic arterial chemotherapy following metastasectomy in patients with isolated liver metastases. Ann Surg 237:782–789
Kemeny NE, Niedzwiecki D, Hollis DR et al (2006) Hepatic arterial infusion versus systemic therapy for hepatic metastases from colorectal cancer: a randomized trial of efficacy, quality of life, and molecular markers (CALGB 9481). J Clin Oncol 24:1395–1403
Kemeny N, Huang Y, Cohen AM et al (1999) Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med 341:2039–2048
Benoist S, Brouquet A, Penna C et al (2006) Complete response of colorectal liver metastases after chemotherapy: does it mean cure? J Clin Oncol 24:3939–3945
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanaka, K., Shimada, H., Matsumoto, C. et al. Impact of the Degree of Liver Resection on Survival for Patients with Multiple Liver Metastases from Colorectal Cancer. World J Surg 32, 2057–2069 (2008). https://doi.org/10.1007/s00268-008-9610-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9610-0