Abstract
Although the sensitivity of preoperative localization techniques is high for solitary parathyroid adenomas, negative imaging study results are inevitable. The weight and location of the parathyroid adenoma may contribute to the negative results. We aimed to study the impact of adenoma weight and ectopic location of the parathyroid adenoma on ultrasonography and sestamibi scan results. The patients were divided into two groups according to adenoma location. Group 1 consisted of 36 patients with ectopic location, and group 2 consisted of 149 patients with normal location. Parathyroid adenoma weight and the results of imaging studies were determined in all patients. Of 185 patients operated on for hyperparathyroidism, 36 (19.4%) had ectopic parathyroid glands. There was a positive correlation between adenoma weight and positive imaging studies, whereas ectopic location did not correlate with negative imaging study results. There was no significant difference between the ectopic adenoma ratio of patients with negative and positive imaging study results. The weight of the ectopic parathyroid adenoma was significantly lower in patients with negative imaging study results than in patients with positive imaging study results (p = 0.001). According to the analysis of variance, patients with higher-weight adenomas have positive imaging study results irrespective of ectopic location. For both normal and ectopic adenoma locations, adenoma weight was found only to be a factor that positively influences imaging study results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Primary hyperparathyroidism (pHPT) is a common endocrine disorder that occurs in approximately one in every 500 women and one in every 2000 men over the age of 40 years [1]. Although a solitary adenoma is responsible for hyperparathyroidism in 80% to 85% of patients, multiple glands (i.e., either multiple adenomas or hyperplasia) are involved in 15% of patients [1, 2].
Bilateral neck exploration has traditionally been considered the gold standard for treating patients with pHPT [3]. During the last decade, with the improvement of preoperative localization techniques and the rapid parathyroid hormone assay, minimally invasive surgery has been advocated for the treatment of pHPT. The success of minimally invasive surgery, however, depends on accurate preoperative localization of parathyroid adenomas [4, 5].
Ultrasonography (US) and sestamibi (MIBI) are currently the most widely used preoperative localization modalities. The sensitivity of US and MIBI identification of parathyroid adenomas ranges between 70% and 90% [6, 7]. Although the sensitivity of US and MIBI are high for solitary parathyroid adenomas, negative results of imaging studies are inevitable [8, 9]. The weight, localization, P-glycoprotein expression, and oxyphil cell content of the parathyroid adenoma may contribute to negative results of imaging studies [10–15]. US is favored because of its low cost, convenience, lack of radiation exposure, and ability to evaluate concomitant thyroid nodules; however, it may fail to detect ectopic parathyroid adenomas [7, 12]. Several studies documented that MIBI has higher sensitivity than US for detecting ectopic parathyroid adenoma [8, 14, 15].
To our knowledge, there have been no studies comparing the effect of adenoma weight and ectopic location on parathyroid adenoma preoperative imaging studies. We aimed to study the relation of parathyroid adenoma weight and ectopic location to the results of US and MIBI.
Materials and Methods
Patients
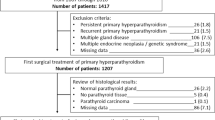
We performed a retrospective study from 2000 to 2007 that included 251 consecutive patients with pHPT who underwent bilateral neck exploration in the Department of General Surgery at the Istanbul Medical Faculty. The data from 185 patients were analyzed. The remaining 66 patients were excluded because of imaging studies performed at another institution (n = 14), parathyroid hyperplasia (n = 11), false-positive scans (n = 28), incomplete data (n = 9), or an ectopic location outside the neck (mediastinum) (n = 4). The patients were divided into two groups according to the parathyroid adenoma localization. Group 1 consisted of 36 (19.4%) patients with an ectopic location, and group 2 consisted of 149 (80.6%) patients with a normal location. In all patients, serum calcium and parathyroid hormone (PTH) levels were measured preoperatively. Serum calcium concentration was adjusted for serum albumin. Normal ranges of biochemical parameters were 8.5 to 10.5 mg/dl for serum calcium and 10 to 65 pg/ml for serum PTH concentrations. The study plan was reviewed and approved by our institutional ethics committee.
MIBI Parathyroid Imaging
A dual-head gamma camera system (ADAC Vertex Plus; ADAC Laboratories, Milpitas, CA, USA) was used for parathyroid imaging. The image matrix was 246 × 256 × 8. For the dual phase methoxyisobutylisonitrile (MIBI) study, 20 mCi 99mTc-MIBI was administered intravenously. Fifteen minutes after injection, the first image of the neck was acquired for 10 minutes. Then, a second image targeting the mediastinum was obtained for 10 minutes. These two images were repeated at the first and second hours. The same nuclear medicine physician reviewed and interpreted all of the scintigraphic images.
Parathyroid Ultrasonography
Neck US examinations were performed by the same skilled operator with a digital US scanner equipped with a 11.4-MHz linear transducer (Sonoline Antares, Siemens, Erlangen, Germany). The US examination was performed with the patient in a supine position with the neck extended, including the central neck from the subclavian vein to the submandibular glands, using the thyroid gland as a reference point. Enlarged parathyroid glands were recognized as a homogenously echogenic structure with less echogenecity than the thyroid gland.
Surgery
Bilateral neck exploration was performed through a standard collar incision with the goal of identifying at least four parathyroid glands; and parathyroid adenomas were excised. An ectopic inferior parathyroid gland was defined as a gland in a location other than on or immediately adjacent to the anterior or posterolateral surface of the inferior pole of the thyroid gland. An ectopic superior parathyroid gland was defined as a gland in a location other than juxtacricothyroidal posteriorly or within the capsule of the posterior surface of the superior pole of the thyroid gland [16, 17]. We confidently identified the ectopic superior versus inferior parathyroid glands, as all of our patients underwent bilateral neck exploration with the identification of all glands (at least four glands). The location of an ectopic parathyroid gland was classified as submandibular, retropharyngeal, retroesophageal, intrathyroidal, within the tracheoesophageal groove, carotid sheath, thyrothymic ligament, or intrathymic. The anatomic location of ectopic parathyroid adenomas was determined from operative reports and compared to the preoperative imaging study results. The weights of all removed parathyroid adenomas were noted.
Statistics
Data were analyzed using SPSS 11.0 for Windows. Results were expressed as means ± SD. Data comparisons were performed by Mann Whitney U-test and chi-squared test. Correlation analyses were performed using nonparametric Spearman’s correlation and two-way analysis of variance (ANOVA) tests. Results were considered statistically significant when p < 0.05 (two-tailed).
Results
Patients
The mean age of the whole group was 47.5 ± 12 years (range 22–77 years). The female/male ratio was 7.4:1.0 (n = 163/22). The mean serum calcium and PTH levels were 12.1 ± 1 mg/dl and 523.16 ± 465 pg/dl, respectively. The mean adenoma weight was 2304.73 ± 3865 mg (range 110–22,000 mg).
Evaluation of Ectopic Location
Of 185 patients operated on for hyperparathyroidism, 36 (19.4%) had ectopic parathyroid glands. Ectopic inferior glands (n = 24; 66.6%) were intrathymic (n = 11; 45.8%) and were found within the thyrothymic ligament (n = 13; 54.2%). Ectopic superior glands (n = 12; 33.3%) were in the tracheoesophageal groove (n = 3; 25%), carotid sheath (n = 4; 33.3%), intrathyroidal (n = 3; 25%) and paraesophageal (n = 2; 16.6%). The mean age was 48.6 ± 16 years in group 1 (ectopic location) and 47.3 ± 10 years in group 2 (normal localization), p > 0.05. The female/male ratio was 33:3 and 130:19 in groups 1 and 2, respectively, p > 0.05. There was not a significant difference between preoperative serum calcium and PTH levels, and adenoma weight of groups 1 and 2 (12.4 ± 0.9 mg/dl, 526 ± 367 pg/dl, and 2242 ± 3688, respectively vs. 12.0 ± 1.0 mg/dl, 522 ± 487 pg/dl, and 2319 ± 3918, respectively; p > 0.05).
Correlations
The ectopic location did not correlate with preoperative serum PTH and Ca levels or adenoma weight (r s = 0.063, p = 0.397; r s = 0.141, p = 0.060; and r s = 0.027, p = 0.715, respectively). There was a positive correlation between adenoma weight and positive US results (r s = 0.629, p = 0.0001), as well as between the adenoma weight and positive MIBI results (r s = 0.745, p = 0.0001) (Fig. 1).
Results of Imaging Studies According to Ectopic Location
In the patients with an ectopic location, US was negative in 11 (30.5%) and positive in 25 (69.5%) patients. There was no significant difference between serum Ca and PTH levels in patients with negative and positive US results (12.3 ± 0.8 vs. 12.5 ± 0.9 mg/dl and 503.09 ± 281.0 vs. 536.12 ± 404.0 pg/ml, p > 0.05). In the patients with negative US results, the mean parathyroid adenoma weights (376.54 ± 177.0 mg) were significantly lower relative to the patients with positive US results (3063.16 ± 4186.0 mg) (p = 0.001) (Fig. 2a).
In patients with an ectopic location, MIBI was negative in 9 (25%) and positive in 27 (75%) patients. There was no significant difference between serum Ca and PTH levels in the patients with negative and positive MIBI results (12.1 ± 0.8 vs. 12.5 ± 0.9 mg/dl and 513.55 ± 308 vs. 530.18 ± 390 pg/ml, p > 0.05). The mean parathyroid adenoma weight was significantly lower in patients with negative MIBI results (306.88 ± 390.0 mg) than in patients with positive MIBI results (2887.37 ± 4072 mg) (p = 0.001) (Fig. 2a). There was no significant difference between the ratio of the successful preoperative localization of ectopic parathyroid adenomas using MIBI and US (69.5% vs. 75%) (p > 0.05).
Evaluation of Positive and Negative Imaging Studies
In patients with parathyroid adenoma, US was negative in 46 (24.8%) and positive in 139 (75.2%) patients. There was no significant difference between serum Ca and PTH levels in patients with negative and positive US results (11.8 ± 1.0 vs. 12.2 ± 1.0 mg/dl and 523.78 ± 519.0 vs. 522.95 ± 448.0 pg/ml, p > 0.05).
In the patients with parathyroid adenoma, MIBI was negative in 41 (22%) and positive in 144 (78%) patients. There was no significant difference between serum Ca and PTH levels of the patients with negative and positive MIBI results (11.9 ± 1 mg/dl vs. 12.1 ± 1 mg/dl and 455.17 ± 519 pg/ml vs. 542.52 ± 498 pg/ml, p > 0.05).
In the patients with negative US and MIBI results, the mean parathyroid adenoma weights (1689 ± 1840 and 1689 ± 1840 mg, respectively) were significantly lower than in patients with positive US and MIBI results (513 ± 297 and 1689 ± 1840 mg, respectively) (p = 0.001) (Fig. 2b). There was no significant difference between the ectopic adenoma ratio of the patients with negative and positive US (23.9% vs. 17.9%) and MIBI results (21.9% vs. 18.7%) (p > 0.05).
Analysis of Variance
According to two-way ANOVA, positive US and MIBI results increased with an increase in adenoma weight (p = 0.001 and p = 0.001, respectively), but positive US and MIBI results decreased with the decrease adenoma weight (p = 0.001 and p = 0.001, respecitvely), independent of the ectopic adenoma localization (Fig. 3). Patients with higher-weight adenomas have positive US and MIBI results irrespective of ectopic location. Adenoma weight was found to be the only independent factor that positively influence imaging study results.
Follow-up
The criteria for success of the operative approaches included follow-up serum calcium and PTH levels. Eleven patients (5.9%) were lost to follow-up. The mean follow-up period of the patients was 33 ± 23 months (range 3–84 months). During this follow-up, two patients (1%) were suspected of having recurrent disease with elevated serum PTH levels. Eleven patients with parathyroid hyperplasia were excluded from this study. Of the 11 patients, 4 patients with previously failed operations were referred to us for recurrent hyperparathyroidism. We had two patients of our own that were operative failures; they were thought to have double adenomas that were not detected during the initial surgery.
Discussion
We compared the effects of adenoma weight and the ectopic location of parathyroid adenoma with the results of US and MIBI. The incidence of ectopic parathyroid adenoma was found to be 19.4%, and the inferior parathyroid adenomas accounted for most of the ectopic adenomas. Among our patients with ectopic parathyroid adenomas, we observed a higher incidence of ectopic adenomas in the thymus and thyrothymic ligament. There was a positive correlation between adenoma weight and positive imaging studies, whereas the ectopic location did not correlate with preoperative serum PTH or Ca levels, adenoma weight, or negative imaging study results. As the parathyroid adenoma weight increased, it significantly correlated with positive US and MIBI results, independent of the ectopic location. For both normal and ectopic adenoma locations, adenoma weight was found to be the only factor that positively influenced imaging study results.
The use of preoperative imaging studies for patients undergoing initial neck exploration for hyperparathyroidism is controversial [3, 4]. Recently, as a result of improved preoperative localization techniques and the rapid PTH assay, minimally invasive surgery has been advocated for pHPT treatment [4, 5, 18–20]. The success of this surgery for pHPT depends on accurate preoperative localization of parathyroid adenomas. Preoperative localization is essential for the safety and efficacy of surgery, particularly in the present era of minimally invasive surgery [4, 21, 22].
During embryogenesis, the upper and lower parathyroid glands descend into the neck. As a result, 20% of parathyroid glands are found in ectopic locations [23, 24]. We found that the incidence of ectopic parathyroid adenoma was 19.4%. The inferior parathyroid glands comprise most of the ectopic glands. Ectopic inferior parathyroid glands are due to abnormal migration during embryogenesis, whereas ectopic superior parathyroid glands are likely due to pathologic displacement from a normal anatomic position. The most common site of an ectopic inferior parathyroid gland is intrathymic, and the most common site of an ectopic superior parathyroid gland is within the tracheoesophageal groove. Ectopic parathyroid glands result from failed parathyroid exploration and increase morbidity [13, 23, 24].
The accuracy of parathyroid adenoma localization by US varies as a function of the size and location of the adenoma; location in the substernal, retrotracheal, and retroesophageal spaces entails poor sensitivity due to acoustic shadowing from overlying bone or air [7, 12]. Intrathyroid adenomas are usually hypoechoic but can be distinguished accurately from thyroid nodules by fine-needle aspiration biopsy. Parathyroid adenomas within the carotid sheath mimic enlarged cervical lymph nodes. Ectopic parathyroid glands are the most common reason for a false-negative US examination [7, 12, 25]. US is less effective than scintigraphy in patients who have ectopically located abnormal parathyroid glands [12, 25]. However, we discovered that MIBI was not superior to US in detecting ectopic parathyroid adenomas. There was no significant difference between the ectopic adenoma ratio in patients with negative and positive imaging study results.
The overall uptake in abnormal parathyroid glands is linked to blood flow, gland size, localization, and mitochondrial activity [6, 10, 26, 27]. Although the advantage of MIBI is its ability to detect ectopic parathyroid adenomas, the addition of single-photon emission computed tomography (SPECT) imaging considerably improved the localization of adenomas in the retroesophageal space [6]. An 81% sensitivity for detection of an ectopic parathyroid adenoma using MIBI is comparable to the 82% sensitivity for detection of all parathyroid adenomas reported in a recent meta-analysis [27]. However, the effect of ectopic adenoma weight on MIBI results was not evaluated in that study. In the present study, the mean parathyroid adenoma weights were significantly lower for ectopic adenomas with negative imaging study results than for those with positive imaging study results. To our knowledge, there have been no studies comparing the effect of adenoma weight and ectopic location. Several studies revealed that adenoma weight is associated with positive imaging study results, and we also found a correlation between adenoma weight and positive imaging study results. Patients with higher-weight adenomas had positive imaging study results, irrespective of adenoma localization.
Conclusions
MIBI was not more effective than US in patients with ectopic small parathyroid adenomas. Patients with higher gland weight were more likely to have a positive localizing study, irrespective of ectopic location.
References
Bilezikian JP, Silverberg SJ (2000) Clinical spectrum of primary hyperparathyroidism. Rev Endocr Metab Disord 1:237–245
Melton LJ (2002) The epidemiology of primary hyperparathyroidism in North America. J Bone Miner Res 17:12–17
Lal G, Clark OH (2003) Primary hyperparathyroidism: controversies in surgical management. Trends Endocrinol Metab 14:417–422
Sackett WR, Barraclough B, Reeve TS, et al (2002) Worldwide trends in the surgical treatment of primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Arch Surg 137:1055–1059
Siperstein A, Berber E, Mackey R, et al (2004) Prospective evaluation of sestamibi scan, ultrasonography, and rapid PTH to predict the success of limited exploration for sporadic primary hyperparathyroidism. Surgery 136:872–880
Smith JR, Oates ME (2004) Radionuclide imaging of the parathyroid glands: patterns, pearls, and pitfalls. Radiographics 24:1101–1115
Huppert BJ, Reading CC (2007) Parathyroid sonography: imaging and intervention. J Clin Ultrasound 35:144–155
Lo CY, Lang BH, Chan WF, et al (2007) A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg 193:155–159
Mihai R, Gleeson F, Buley ID, et al (2006) Negative imaging studies for primary hyperparathyroidism are unavoidable: correlation of sestamibi and high-resolution ultrasound scanning with histological analysis in 150 patients. World J Surg 30:697–704
Mehta NY, Ruda JM, Kapadia S, et al (2005) Relationship of technetium Tc 99m sestamibi scans to histopathological features of hyperfunctioning parathyroid tissue. Arch Otolaryngol Head Neck Surg 131:493–498
Pattou F, Torres G, Mondragon-Sanchez A, et al (1999) Correlation of parathyroid scanning and anatomy in 261 unselected patients with sporadic primary hyperparathyroidism. Surgery 126:1123–1131
Barraclough BM, Barraclough BH (2000) Ultrasound of the thyroid and parathyroid glands. World J Surg 24:158–165
Phitayakorn R, McHenry CR (2006) Incidence and location of ectopic abnormal parathyroid glands. Am J Surg 191:418–423
Haber RS, Chun K, Kim CK, et al (2002) Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with 99m technetium sestamibi scintigraphy. Clin Endocrinol (Oxf) 57:241–249
Lumachi F, Zucchetta P, Varotto S, et al (1999) Noninvasive localization procedures in ectopic hyperfunctioning parathyroid tumors. Endocr Relat Cancer 6:123–125
Dyson M (1995) Endocrine system. In: Williams PL, (eds). Gray’s anatomy, 38th edition. Churchill Livingstone, New York, pp 1881–1907
Wang CA (1976) The anatomic basis of parathyroid surgery. Ann Surg 183:271–275
Bhansali A, Masoodi SR, Bhadada S, et al (2006) Ultrasonography in detection of single and multiple abnormal parathyroid glands in primary hyperparathyroidism: comparison with radionuclide scintigraphy and surgery. Clin Endocrinol (Oxf) 65:340–345
Mariani G, Gulec SA, Rubello D, et al (2003) Preoperative localization and radioguided parathyroid surgery. J Nucl Med 44:1443–1458
Stephen AE, Roth SI, Fardo DW, et al (2007) Predictors of an accurate preoperative sestamibi scan for single-gland parathyroid adenomas. Arch Surg 142:381–386
Miccoli P, Berti P (2001) Minimally invasive parathyroid surgery. Best Pract Res Clin Endocrinol Metab 15:139–147
Miccoli P, Berti P, Raffaelli M, et al (2001) Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 130:1039–1043
Wang CA (1976) The anatomic basis of parathyroid surgery. Ann Surg 183:271–275
Vail AD, Coller FC (1967) The parathyroid glands: clinicopathologic correlation of parathyroid disease as found in 200 unselected autopsies. Mol Med 64:234–238
Kamaya A, Quon A, Jeffrey RB (2006) Sonography of the abnormal parathyroid gland. Ultrasound Q 22:253–262
Westreich RW, Brandwein M, Mechanick JI, et al (2003) Preoperative parathyroid localization: correlating false-negative technetium 99m sestamibi scans with parathyroid disease. Laryngoscope 113:567–572
Castellani M, Reschini E, Longari V, et al (2001) Role of Tc-99m sestamibi scintigraphy in the diagnosis and surgical decision-making process in primary hyperparathyroid disease. Clin Nucl Med 26:139–144
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erbil, Y., Barbaros, U., Tükenmez, M. et al. Impact of Adenoma Weight and Ectopic Location of Parathyroid Adenoma on Localization Study Results. World J Surg 32, 566–571 (2008). https://doi.org/10.1007/s00268-007-9389-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9389-4